Using Simulation Modeling to Guide the Design of the Girl Scouts Fierce & Fit Program
Abstract
Objective
The study aim was to help the Girl Scouts of Central Maryland evaluate, quantify, and potentially modify the Girl Scouts Fierce & Fit program.
Methods
From 2018 to 2019, our Public Health Informatics, Computational, and Operations Research team developed a computational simulation model representing the 250 adolescent girls participating in the Fierce & Fit program and how their diets and physical activity affected their BMI and subsequent outcomes, including costs.
Results
Changing the Fierce & Fit program from a 6-week program meeting twice a week, with 5 minutes of physical activity each session, to a 12-week program meeting twice a week with 30 minutes of physical activity saved an additional $84,828 ($80,130-$89,526) in lifetime direct medical costs, $81,365 ($76,528-$86,184) in lifetime productivity losses, and 7.85 (7.38-8.31) quality-adjusted life-years. The cost-benefit of implementing this program was $95,943. Based on these results, the Girl Scouts of Central Maryland then implemented these changes in the program.
Conclusions
This is an example of using computational modeling to help evaluate and revise the design of a program aimed at increasing physical activity among girls.
Study Importance
What is already known?
- ► The ongoing childhood obesity and physical inactivity epidemics have motivated the development of programs to increase the amount of time adolescents are physically active. However, designing such programs can be challenging because the connections between different aspects of the programs and the health outcomes can be complex.
- ► Computational simulation modeling has been used to transform decision-making for programs in other fields such as transportation and meteorology.
What does this study add?
- ► This study is an example of how computational modeling can help guide the design of a program aimed at increasing physical activity among adolescent girls.
- ► As a result of model simulations, Girl Scouts of Central Maryland changed its Fierce & Fit program by doubling the length and frequency of the program and increasing physical activity during sessions sixfold, which is expected to deliver lifetime direct and indirect health cost savings nearly 2.5 times greater than the cost of implementing the program.
How might these results change the direction of research?
- ► There remain significant opportunities for computational modeling to more directly guide the design of strategies and programs to address a wider variety of health issues. As this study demonstrates how computational modeling can inform decision-making, it can help shift how research is conducted.
Introduction
The ongoing childhood obesity and physical inactivity epidemics have motivated efforts to get adolescents to be more physically active. The adolescent years are particularly crucial because that is when children begin to make more autonomous decisions, establishing behaviors that may last well into adulthood, and experience substantial amounts of growth. Evidence has suggested that 95% of adolescents with obesity will continue to have obesity into adulthood.
Designing such programs can be challenging because the connections between different aspects of the programs and the health outcomes can be complex. For example, there are significant time lags between physical activity levels and health outcomes, many of which occur well into adulthood. Questions about the relative benefits and long-term outcomes of adjusting meeting frequency and program duration can be difficult to answer within the short time frame of most clinical trials. Population cohort studies over extended periods of time can show general associations but may lack the fidelity to guide program design.
Computational simulation modeling is used in other fields such as air traffic control to design procedures and coordinate daily operations ((1)). The Girl Scouts of Central Maryland (GSCM) were interested in evaluating and potentially modifying the Girl Scouts Fierce & Fit program. Therefore, this represented an opportunity to utilize computational modeling to evaluate the potential daily effects of the program, to evaluate how these effects may progress throughout the program and over the course of the participants’ lifetimes, and then to recommend whether and how the program should be modified.
Methods
Girl Scouts Fierce & Fit program
Established in 2016, Fierce & Fit is a daytime and afterschool program designed for girls in kindergarten through eighth grade that puts lessons about physical activity and nutrition into action during program sessions.
Our partnership with the GSCM originally stemmed from GSCM’s strong interest in evaluating the Fierce & Fit program, improving it based on the findings, and ultimately demonstrating the impact to funders and policy makers.
Model structure
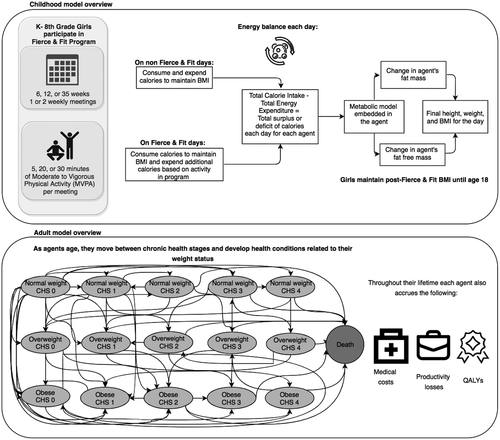
To quantify the health and economic impact of different configurations of the Fierce & Fit program, we developed a computational simulation model of virtual Girl Scouts Fierce & Fit participants or agents, ages 5 to 14 years (kindergarten through eighth grade) in Baltimore City.
Each day, each virtual Fierce & Fit participant has an opportunity to participate in additional physical activity, depending on whether the program is hosted on a particular day. If it is a day when the program is offered, each agent is physically active for the amount of time that physical activity is incorporated into the curriculum for that session. Girls who participate in physical activity during the Fierce & Fit program increase their caloric expenditure.
Each virtual girl also has an embedded metabolic model (adapted from previously published models ((2, 3))) that represents the processes by which the agent’s body translates consumed and expended calories into daily changes in weight. This translation occurs in a series of steps. First, when a virtual girl consumes food or drink, the resulting calories enter the metabolic model. Ingested calories first satisfy energy needs for the basal metabolic rate, thermic effect of feeding, adaptive thermogenesis, and physical activity. Basal metabolic rate is the energy needed to keep a body functioning when at rest and is calculated for each girl by summing the energy needs of the girl’s fat mass, fat-free mass, and organs ((4-6)). The thermic effect of feeding refers to the energy needed by the girl to process food ((3)). Adaptive thermogenesis is the regulation of metabolic speed based on changes in energy intake ((3)). Supporting Information Table S1 provides values for the specific components. To obtain daily caloric expenditure from physical activity, we multiplied physical activity intensity measured in metabolic equivalents, physical activity duration, and the girl’s current body weight. The values for intensity and duration vary based on the changes to the program delineated under “Simulation Experiments” and “Sensitivity Analyses.” When calculating the energy needs for each of these components, the model determines the energy needed to grow along the Centers for Disease Control and Prevention projection of the girl’s weight ((7)), meaning these caloric needs change each day to account for growth. For this study, we assume girls consume the number of calories needed to maintain their starting BMI percentile; this amount does not change when we adjust the amount of physical activity in the experiments. At the end of each day, if the caloric intake is greater than the calories needed to achieve desired growth, the girl gains extra weight. If the total caloric intake does not meet the number of calories needed to maintain her weight, the girl metabolizes energy stores, resulting in weight loss.
After a Girl Scout completes an entire Fierce & Fit program, we assume that she maintains her end-of-program BMI until 18 years of age. This assumption is conservative, as current studies have indicated that BMI percentiles of females during early adolescence often persist or increase as they age into adulthood ((8-10)). At age 18, virtual girls move to the adult portion of the model, a Markov model developed in TreeAge Pro ((11, 12)). This model simulates changes in the female’s obesity status and obesity-associated health conditions (Supporting Informations Table S2-S6). Each girl that enters the Markov model begins in 1 of 15 health states based on a well-established clinical staging system for obesity ((13)). As shown in Supporting Information Table S2, each health state includes BMI category and has a probability of the following four obesity-associated health outcomes: stroke, cancer, coronary heart disease, and type 2 diabetes mellitus complications. After each simulated year, girls transition between BMI and health states based on age-related changes in weight status, physical activity habits, and dietary habits, as reflected in the Coronary Artery Disease Risk Development in Young Adults (CARDIA) ((14)) and Atherosclerosis Risk in Communities (ARIC) ((15)) studies. On a yearly basis starting at age 18, each girl/woman accrues state-, health outcome–, and age-specific medical costs, lost productivity, and quality-adjusted life-years (QALYs) (Figure 1).
Baltimore City girls population
We represented the 250 girls from 16 schools in the Fierce & Fit program, as 250 girls participated in the Fierce & Fit program in 2018. As already described, we virtually represented each girl in the program with a computational agent. Like real girls, each virtual Girl Scout participant had an age, race/ethnicity, height, and weight (fat and fat-free mass). Girls in the program were predominantly African American. Each girl’s height and fat and fat-free mass were sampled from girls with matching demographics from the 2013-2014 National Health and Nutrition Examination Survey (NHANES). The resulting BMIs corresponded to the overweight and obesity prevalence for the initial population. Of the total, 21.2% fell into the overweight category, and 21.6% had obesity. This translated to 53 girls with overweight and 54 girls with obesity.
Simulation experiments
The original Fierce & Fit program met once a week for 60 minutes for 6 weeks and involved girls in approximately 5 minutes of moderate to vigorous physical activity (MVPA) each session. We simulated the current Fierce & Fit program and then adjusted the program. The intensity of physical activity during each Fierce & Fit session was set as an average of six metabolic equivalents based on the types of activities reported in the original Fierce & Fit curriculum. We simulated programs that met for different periods of time ranging from 6 weeks to 35 weeks. We then increased the frequency of the program from meeting once a week to twice a week. We also tested changes to the physical activity portion of the curriculum by ranging the amount of MVPA time in the program from 5 minutes to 30 minutes each session. We then combined changes to the program duration, frequency, and amount of time active. For each scenario, we ran the model 100 times and reported mean and 95% uncertainty interval. We applied changes to the Fierce & Fit program uniformly across program participants regardless of race or age.
Sensitivity analyses
While our model was able to recreate overweight prevalence among African American girls (21.1%) compared with 20.7% ((16)) of third-grade Baltimore students whose weight status was overweight, we varied the overweight and obesity prevalence of the population to quantify how the program affected populations of different weight statuses. For example, the national average obesity rate for 6- to 11-year-old girls is 16.3% ((17)). We tested the following overweight and obesity prevalences: (1) 10% with overweight, 10% with obesity; (2) 15% with overweight, 15% with obesity; and (3) 25% with overweight, 25% with obesity.
Prior studies have shown that participants in programs similar to Fierce & Fit increase their daily physical activity outside of the program ((18, 19)). We tested this carry-over effect in simulations in which girls were active for an additional 3 minutes per day on nonmeeting days during each program, for a year after the end of each program, and until each girl turned 18 and entered our adult model.
Peers of a participant can affect the girl’s participation in two primary ways. First, they can either encourage (e.g., if she likes her peers, she may be more likely to attend) or discourage (e.g., dislike or lack of connection may make her less likely to attend) the Girl Scout from attending sessions. Second, while the Girl Scout is in a session, the amount of time she remains active may depend on peers as well. For example, if her peers are active throughout the session, the Girl Scout may be more likely to do so too. Conversely, if her peers want to spend time doing other things such as talking, the Girl Scout may not remain as active during the sessions. In order to represent all of these possibilities, different scenarios varied the probability that a Girl Scout (25%-75%) would attend each session and the amount of time that a Girl Scout would remain active during a given session (5-30 minutes).
We also explored how participants may influence peers not in the program to become more active. For example, if the program convinces participants to be more active outside of the program, her peers who are not in the program may be active with her. To represent these effects, scenarios simulated a participant influencing one to three friends to increase their MVPA by 3 minutes a day for 1 year following the program.
We also varied the proportion of participants who maintained their BMI from the end of the program until age 18 (e.g., 75%-25% of girls maintain end of Fierce & Fit program BMI, and the remaining proportion go back to their BMI prior to participating in the program).
Additionally, we evaluated how changes to program duration, meeting frequency, and amount of MVPA during the program would impact attendance, varying the proportion of girls (25%-75%) who attend each session.
Other sensitivity analyses examined how changes to the duration, frequency, and amount of MVPA may result in program participants compensating by both reducing MVPA outside of the program and increasing calorie consumption outside of the program such that their additional caloric expenditure from MVPA is only 75% to 25% of physical activity during the program (e.g., a girl at age 10, weighing 103.8 pounds, eats between 170 and 211 additional calories per week).
Results
Original Fierce & Fit program
In 2018, the Fierce & Fit program met once per week for 6 weeks and averaged about 5 minutes of MVPA per session. In our simulations, this resulted in an average of $2,465 ($1,366-$3,564) in savings from direct medical costs, $1,825 ($1,011-$2,639) in averted productivity loss, and 0.30 (0.17-0.44) in saved QALYs over the lifetime of the participating population (Table 1).
| Reduction in cases of OWO, mean (CI) | Reduction in direct medical costs, mean (CI) | Reduction in productivity loss, mean (CI) | Saved QALYs, mean (CI) | Average change in BMI percentile, mean (CI) | |
|---|---|---|---|---|---|
| Current MVPA per session (5 minutes) | |||||
| 6-week program length | |||||
| 1 × per week | 0.0 | $2,465 ($1,366 to $3,564) | $1,825 ($1,011 to $2,639) | 0.3 (0.2 to 0.4) | −0.0006 (−0.0040 to 0.0027) |
| 2 × per week | 0.0 | $2,191 ($1,137 to $3,246) | $1,622 ($841 to $2,403) | 0.3 (0.1 to 0.4) | −0.0013 (−0.0046 to 0.0020) |
| 12-week program length | |||||
| 1 × per week | 0.0 | $2,465 ($1,366 to $3,564) | $1,825 ($1,011 to $2,639) | 0.3 (0.2 to 0.4) | −0.001 (−0.004 to 0.002) |
| 2 × per week | 0.0 | $7,944 ($5,858 to $10,029) | $5,881 ($4,337 to $7,425) | 1.0 (0.7 to 1.2) | −0.002 (−0.005 to 0.001) |
| 35-week program length | |||||
| 1 × per week | 0.24 (0.15 to 0.33) | $11,600 ($9,066 to $14,135) | $9,883 ($7,803 to $11,962) | 1.2 (0.9 to 1.5) | −0.003 (−0.006 to 0.001) |
| 2 × per week | 1.1 (0.9 to 1.3) | $23,685 ($20,055 to $27,315) | $23,576 ($20,023 to $27,129) | 2.1 (1.7 to 2.4) | −0.005 (−0.008 to −0.002) |
| Increasing MVPA per session (20 minutes) | |||||
| 6-week program length | |||||
| 1 × per week | 0.13 (0.06 to 0.20) | $9,593 ($7,701 to $11,486) | $7,803 ($6,207 to $9,399) | 1.1 (0.9 to 1.3) | −0.003 (−0.006 to 0.000) |
| 2 × per week | 1.1 (0.9 to 1.3) | $21,726 ($18,703 to $24,748) | $22,180 ($19,119 to $25,241) | 1.8 (1.5 to 2.1) | −0.006 (−0.009 to −0.002) |
| 12-week program length | |||||
| 1 × per week | 1.1 (0.9 to 1.3) | $21,630 ($18,366 to $24,895) | $22,055 ($18,876 to $25,234) | 1.8 (1.5 to 2.1) | −0.005 (−0.008 to −0.002) |
| 2 × per week | 2.7 (2.5 to 3.0) | $59,572 ($54,695 to $64,449) | $58,829 ($54,348 to $63,310) | 5.3 (4.7 to 5.8) | −0.010 (−0.014 to −0.007) |
| 35-week program length | |||||
| 1 × per week | 3.0 (2.7 to 3.4) | $76,538 ($70,570 to $82,506) | $73,007 ($67,184 to $78,831) | 7.1 (6.5 to 7.7) | −0.011 (−0.013 to −0.008) |
| 2 × per week | 6.7 (6.3 to 7.1) | $133,647 ($126,067 to $141,227) | $134,976 ($127,641 to $142,311) | 11.4 (10.7 to 12.2) | −0.023 (−0.026 to −0.020) |
| Increasing MVPA per session | |||||
| 6-week program length | |||||
| 1 × per week | 0.8 (0.6 to 1.0) | $16,854 ($14,154 to $19,554) | $16,901 ($14,225 to $19,577) | 1.5 (1.2 to 1.7) | −0.004 (−0.008 to −0.001) |
| 2 × per week | 2.4 (2.1 to 2.7) | $42,142 ($38,004 to $46,279) | $44,199 ($40,031 to $48,367) | 3.4 (3.0 to 3.8) | −0.009 (−0.013 to −0.005) |
| 12-week program length | |||||
| 1 × per week | 1.6 (1.3 to 1.9) | $35,339 ($31,737 to $38,942) | $34,847 ($31,086 to $38,609) | 3.1 (2.8 to 3.5) | −0.008 (−0.011 to −0.004) |
| 2 × per week | 3.4 (3.1 to 3.8) | $87,293 ($81,496 to $93,090) | $83,181 ($77,539 to $88,823) | 8.2 (7.6 to 8.8) | −0.016 (−0.019 to −0.012) |
| 35-week program length | |||||
| 1 × per week | 4.9 (4.5 to 5.3) | $117,380 ($110,678 to $124,082) | $113,493 ($107,007 to $119,979) | 10.7 (10.0 to 11.4) | −0.017 (−0.020 to −0.014) |
| 2 × per week | 9.5 (9.0 to 10.0) | $187,872 ($179,148 to $196,596) | $190,386 ($182,073 to $198,700) | 15.9 (15.0 to 16.9) | −0.034 (−0.037 to −0.030) |
- OWO, overweight and obesity.
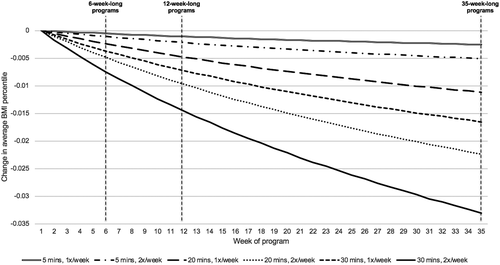
Varying length of program
When MVPA remained at 5 minutes per session, as it was in the original Fierce & Fit program, the most significant difference occurred when the model increased program length to 35 weeks and meetings to twice per week. Results from this simulation determined that the lifetime savings of the 250 participants was $23,685 ($20,055-$27,315) in direct medical costs, $23,576 ($20,023-$27,129) in productivity loss, and 2.07 (1.71-2.43) QALYs (Table 1).
Varying amount of physical activity each session
When we increased MVPA to 20 minutes per session and kept the current program’s length and number of meetings per week, the program saved $9,593 ($7,701-$11,486) in direct medical costs, $7,803 ($6,207-$9,399) in productivity loss, and 1.08 (0.87-1.30) QALYs. This represented a significant increase in savings from the baseline, with an additional $7,128 ($6,335-$7,922) in direct medical costs, $5,978 ($5,196-$6,760) in productivity loss, and 0.78 (0.7-0.86) in saved QALYs (Table 1).
Varying frequency of meetings each week
At the current program length of 6 weeks, increasing the frequency of meetings from once to twice per week did not make a significant difference in health and economic outcomes. Though frequency of meetings alone did not make a significant difference in outcomes, combinations of the three variables did yield further savings (Table 1).
Combining variations on length, frequency, and amount of physical activity each session
Increasing program length to 35 weeks and the frequency of sessions to twice per week saved $133,647 ($126,067-$141,227) in direct medical costs, $134,976 ($127,641-$142,311) in productivity loss, and 11.41 (10.65-12.16) QALYs.
Increasing MVPA to 30 minutes per session for a 35-week program that met twice a week averted an additional $187,872 ($179,148-$196,596) in direct medical costs, $190,386 ($182,073-$198,700) in productivity losses, and 15.94 (15.02-16.87) QALYs. In this simulation, the number of cases of overweight and obesity dropped by 9.51(8.99-10.03).
The simulations showed that it was not necessary to increase all variables to maximum in order to gain significant savings from changes in the program structure. Changing the program to 12 weeks in length and meeting twice per week, with 30 minutes of activity per session, reduced cases of overweight and obesity by 3.44 (3.07-3.81) and saved an additional $84,828 ($80,130-$89,526) in direct medical costs, $81,356 ($76,528-$86,184) in productivity loss, and 7.85 (7.38-8.31) QALYs (Table 1). Figure 2 also shows how changes to the program impacted the participant’s BMI percentile.
Ranging initial overweight and obesity prevalence
Adjusting the starting overweight and obesity prevalence from 20% to 50% showed that while greater impacts typically occurred among populations with higher overweight and obesity prevalence, the Fierce & Fit program was still impactful among populations with only 20% overweight and obesity prevalence. For example, we observed $63,777 ($58,323-$69,231) in direct medical cost savings over a 12-week program that met twice a week with 20 minutes of MVPA among a population with 50% prevalence of overweight and obesity compared with $29,289 ($25,703-$32,875) in direct medical cost savings over the same program hosted across a population with a prevalence of overweight and obesity of 20% (Supporting Information Tables S7-S9).
Varying carry-over of physical activity behavior outside of program sessions
During a 12-week-long program meeting twice per week with 20 minutes of MVPA per meeting, increasing daily MVPA by 3 minutes on nonmeeting days led to 0.54 (0.48-0.60) fewer cases of overweight and obesity and the extra MVPA saved 3.57 (3.44-3.69) QALYs.
A 3-minute daily increase of MVPA that lasted for a year after the end of this 12-week-long program reduced the number of overweight and obesity cases by 2.09 (1.92-2.26) and saved 4.92 (4.74-5.10) additional QALYs. It also saved $52,788 ($50,610-$54,966) in direct medical costs and averted $50,354 ($47,918-$52,790) in productivity losses.
Finally, when girls sustained 3 minutes of additional daily activity until they turned 18, cases of overweight and obesity declined by 5.59 (5.38-5.80), and 7.80 (7.67-7.92) QALYs were saved. Additionally, $97,648 ($96,060-$99,235) in direct medical costs and $102,446 ($100,319-$104,573) in productivity losses were averted (Supporting Information Table S10).
Varying attendance rates
When 75% of participants attended each session during the 35-week program that met twice a week and were active for 30 minutes each session, the program still averted $159,149 ($151,990-$166,309) in direct medical costs, and when 25% of participants attended a given session, there was a reduction in direct medical costs of $55,309 ($50,385-$60,232). We also observed a reduction in the number of overweight and obesity cases ranging from 8.35 (7.87-8.83) to 2.8 (2.45-3.15). Fierce & Fit may continue to see economic and health benefits even when attendance rates vary during the program (Supporting Information Table S11).
Participants convincing their peers to increase physical activity after Fierce & Fit program
When each of the 250 girls in the 35-week program, meeting twice a week, were active for 30 minutes each session and convinced one friend to be active for 3 minutes of MVPA each day for 1 year following Fierce & Fit, the program reduced direct medical costs by $358,755 ($348,194-$369,316); when Girl Scouts convinced two and three friends, direct medical costs were lowered by $534,752 ($519,140-$550,364) and $718,640 ($701,777-$735,503), respectively (Supporting Information Table S11).
Varying proportion of participants who maintain postprogram BMI percentile until age 18
During the 35-week program meeting twice a week and with 30 minutes of activity each session, when 75% of girls maintained their BMI percentile following the program until age 18 and 25% reverted to preprogram BMI, we saw a reduction in direct medical costs of $140,406 ($134,086-$146,727). When 50% of girls maintained postprogram BMI percentile, we observed a reduction of $87,344 ($82,200-$92,488) in direct medical costs, with a reduction of $48,895 ($44,663-$53,127) when 25% of girls maintained their postprogram BMI. Results demonstrated that the program can still result in cost savings even if some participants do not maintain their end-of-program BMI (Supporting Information Table S11).
Compensating by reducing physical activity outside of program or increasing caloric consumption outside of program
When girls compensated for physical activity during the Fierce & Fit program by reducing their physical activity outside of the program, such that they expended only 75% of calories from the program, direct medical costs were $158,387 ($151,029-$165,746); when they compensated such that they expended only 50% of calories from the program, direct medical costs decreased by $112,467 ($105,752-$119,183); and when participants compensated such that they expended only 25% of calories from the program, direct medical costs were reduced by $48,996 ($44,108-$53,884). Thus, the program may still have benefits even when compensation occurs (Supporting Information Table S11).
Changes made to Fierce & Fit program as a result of our simulation experiments
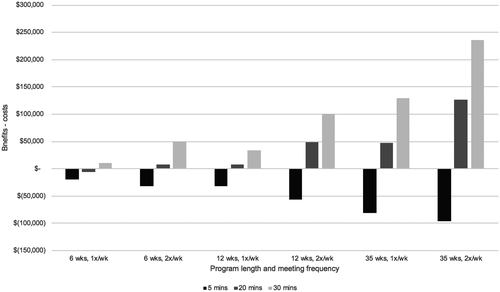
The main change as a result of our simulation programs was the GSCM deciding to restructure the Fierce & Fit program. They decided to change their original program format from a 6-week program meeting once per week with approximately 5 minutes of MVPA each session to a 12-week program with sessions meeting twice per week with 30 minutes of MVPA per session. GSCM made this decision after considering a wide range of model simulations results, including a cost-benefit comparison that found that none of the programs that offered 5 minutes of activity was cost-effective; however, all besides one (6 weeks, once a week) of the programs bringing activity levels to 20 or 30 minutes per session showed a positive benefit (Figure 3). GSCM combined this analysis with what was feasible for their team both financially and capacity-wise. They are currently piloting this new model. Additionally, the modeling has informed additional data collection for the program. GSCM has now developed pre- and postsurveys of the program, including questions on each participant’s level of physical activity outside of the program. Furthermore, they have developed a monitoring tool based on System for Observing Play and Leisure Activity in Youth (SOPLAY) ((20)), which is a more detailed way of tracking the amount of physical activity that occurs during the program sessions. This information can be used to update future iterations of the model.
Discussion
This is an example of using computational modeling to help refine the design of a physical activity program. As indicated in our results, the GSCM made changes in their Fierce & Fit program based on the simulation experiments. This included expanding the structure of their program to last for twice as long (from 6 weeks to 12 weeks), to meet twice as often (from once per week to twice per week), and to increase the amount of time girls are actually active during the program sixfold (from 5 minutes to 30 minutes).
Other professions and industries routinely use mathematical and computational modeling to guide decision-making and program design. For example, weather planning relies on the use of meteorological simulation models that produce the weather maps frequently seen on television. These simulation models combine and integrate information from many different types of data from sources such as air, land, and water temperature; barometric pressure; wind speed and direction; and cloud patterns. Such models can help communities plan evacuations when hurricanes are forming and approaching, event planners determine when rain delays may occur, air traffic controllers and pilots alter flight patterns, and farmers establish crop planning.
By contrast, modeling has historically not played as prominent a role in helping health and health-related decision-making. In the past, there have been some examples of computational modeling guiding policy, intervention, and program design for the control of infectious diseases. For example, during the 2009 H1N1 influenza pandemic, computational simulation models helped national, state, and local decision-makers answer questions about whether to close schools, how antiviral medications should be used, and who should get vaccines first when vaccines were in short supply ((21-25)). Computational models have also helped decision-makers plan new vaccine introductions ((26, 27)), determine how best to design vaccine-carrying devices ((28, 29)), and determine how to redesign health product supply chains ((30, 31)). The use of computational models to directly guide program design in other health areas is relatively new. There are some examples of modeling studies published in the tobacco control and urban planning areas ((32, 33)). However, there remain significant opportunities for computational modeling to more directly guide the design of strategies and programs to address a wider variety of health issues.
Without simulation modeling, it can be difficult to understand the impact of different aspects of a physical activity program. Testing each program aspect separately to determine the drivers requires significant time and resources and may not fully account for other contextual factors affecting the changes. The degree to which a specific program component impacts health and associated costs takes a lifetime to manifest, and decision-makers cannot afford to wait that long to see the impacts, not to mention the logistical challenges of tracking cohorts of individuals into and throughout adulthood.
All models simplify reality ((34, 35)) and cannot include all possible factors impacting girls’ participation in Fierce & Fit or their behavior outside of the program. The health and economic impacts that we modeled and presented include effects that accrue over time, as our goal was to elucidate the relationship between the program and long-term impacts that may not otherwise be understood. While we conducted a range of sensitivity analyses to account for various circumstances, we cannot account for all possibilities and changes that may occur between the time of the program and the time of various outcomes. Because we focused on the obesity-related benefits of Fierce & Fit, the simulations do not account for impacts of the program that cannot be tied directly to decreases in costs or BMI. GSCM teaches girls about self-esteem, mindfulness, and developing healthy lifestyle habits, all of which are salutary in ways that the model does not capture.
Conclusion
This is an example of using computational modeling to help evaluate and revise the design of a program aimed at increasing physical activity among girls. Our simulation model showed that increasing duration, frequency, and time active during the program can result in significant cost savings. GSCM then utilized these results to alter the design of the Fierce & Fit program.
Funding agencies
The project described was supported by the Global Obesity Prevention Center (GOPC) and Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Office of the Director, National Institutes of Health (OD) under award number U54HD070725. This project is also funded by NICHD via grant U01HD086861 and 5R01HD086013-02 as well as the Agency for Healthcare Research and Quality (AHRQ) via grant R01HS023317. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD or AHRQ. This study was supported, in part, by a grant from the Lerner Center for Public Health Promotion at Johns Hopkins Bloomberg School of Public Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Lerner Center for Public Health Promotion. The study sponsors did not have any role in the study design, collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Disclosure
The authors declared no conflicts of interest.
Author contributions
Conceived and designed experiments: MCF, MJM, KJO, VM, AW, and SSS. Parameterized experiments: MCF, MJM, VM, TC, and AW. Programmed the model and experiments: LW, MSG, and DLH. Performed experiments: LW, MSG, and DLH. Analyzed data: MCF, MJM, KJO, SR, and SSS. Wrote the paper: MCF, MJM, KJO, VM, TC, AW, SSS, and BYL. Helped guide data collection for model parameters: MCF, MJM, KJO, VM, TC, AW, SSS, and BYL. Helped guide technical methodology: MCF and BYL.





