Obesity Risk Among Young Australian Women: A Prospective Latent Class Analysis
Abstract
Objective
Prospective studies on obesity incidence specifically among young adults have not been reported. This study examined risks of obesity incidence over 19 years among young women without obesity at baseline.
Methods
Women aged 18 to 23 years at baseline (N = 8,177) were followed up every 2 to 3 years to ages 37 to 42 using the Australian Longitudinal Study on Women’s Health. A latent class analysis identified obesity-risk classes based on time-dependent measures of income, education, physical activity, sleep quality, dietary behavior, depression, stressful events, and social functioning. Cox proportional hazards regression models examined associations between incident obesity and latent classes, controlling for covariates.
Results
Four latent classes were identified, including a lower-risk referent class and classes characterized by poor exercise and diet, stress and low income, and multiple intermediate-level risks. Compared with the referent, all three risk classes had significantly higher obesity risk, with the highest risk in the stress and low-income group (hazard ratio = 2.22; 95% CI: 1.92-2.56). Individual risks associated with obesity included lower education, stressful life events, and lower vigorous physical activity.
Conclusions
Young women without baseline obesity were at risk of developing obesity when they experienced co-occurring behavioral, socioeconomic, and psychosocial risks. Both latent classes and individual risk indicators offer insights into prevention strategies.
Study Importance
What is already known?
- Obesity rates are increasing among children and adults worldwide.
- Individual risk variables have been studied as main effects.
What does this study add?
- A prospective analysis of obesity risk among young adult women has not before been undertaken.
- Latent class analysis in Australia adds new information about risk variables as coexposures.
Introduction
Obesity is a global public health epidemic (1, 2). Estimates are that the prevalence of obesity among adults worldwide was approximately 37.5% in 2013; rates specifically among women were 38.0% (3). The overweight and obesity prevalence is approximately 67% among adults in Australia as of 2015, with the obesity rate itself at 31% (4). Currently, there are 1.9 billion adults and 340 million children globally with overweight or obesity (5). These figures are concerning because obesity is a well-established risk factor for serious chronic health problems, including type 2 diabetes, cardiovascular disease, some forms of cancer (including breast and endometrial cancer), and early mortality (2, 6-8).
The problem of obesity, however, is not restricted to adults, and of great concern has been the observation that obesity is occurring with increasing prevalence among children and adolescents (3). Overweight or obesity in children and adolescents stands at about 23% in developed countries globally and has been increasing in both developed and developing nations (3). Overweight and obesity among children in Australia stands at about 25% (4). These trends indicate that the obesity epidemic has been expanding to impact populations at younger ages.
Studies of obesity risk have usually been focused on children, adolescents, or adults of all ages. The development of obesity specifically among younger adults has not been well investigated. An important study by Zheng et al. (9) revealed that women who, at age 55, recalled greater weight gain over the adult years beginning at age 18 had greater risk for diabetes, hypertension, cardiovascular disease, and obesity-related cancer. Weight gain from early adulthood was based on retrospective self-report. Alati et al. (10) documented a generational increase in young adult obesity rates from mothers to daughters and from fathers to sons. Neither of these studies investigated obesity incidence prospectively in young adults. Dietz (11) argued for the need for research focused on young adult obesity prevention. To better target prevention efforts to this population, targeted research into risks is necessary.
Factors contributing to obesity risk have generally been focused on lifestyle behaviors, including poor diets and lack of physical activity (12-14). Other risks include low socioeconomic status (SES) (15), poor access to healthy food sources (16, 17), and psychological issues such as depression or stress (18-20). These risks do not operate in isolation of one another (21). Low SES, for example, influences diet, food access, and psychological health (15, 22). The Chronic Care Model stipulates that multiple individual behaviors and environmental conditions interact to promote healthy or unhealthy weight conditions (23), but attempts to model multiple influences have rarely been undertaken. Although multiple obesity risks are recognized, most research on the predictors or correlates of obesity has been focused on independent effects of single variables.
Analyzing multiple co-occurring influences on a health outcome of interest has been challenging, in part, because of limitations of traditional statistical approaches. Statistical power for investigation of co-exposures is often lacking. In addition, collinearity among important predictors may mask combined influences. Latent class analysis (LCA) offers an approach to address these limitations (24). LCA uses observed items to divide a heterogeneous population into unobserved, discrete, mutually exclusive, and exhaustive subgroups or classes in which members share common features. An advantage of LCA is that it provides for the identification and interpretation of simultaneous co-exposures among multiple variables.
LCA studies of obesity risk in children have been undertaken (25-28). Huh et al. (25), for example, used items assessing eating, physical activity, and weight perception variables to identify five latent classes in children that were related to obesity risk. Magee et al. (29) conducted a cross-sectional LCA of sleep quality in Australian adults; poor sleepers had higher BMI. Another sleep study (30) followed up children in Australia over 2 years; three latent weight-trajectory classes were identified, and children with short sleep duration were at higher risk for increased BMI. However, no prospective LCA studies have been undertaken to examine the transition to having obesity among young adults without obesity at baseline.
The purpose of the current study was to conduct an LCA to identify whether there are co-occurring exposure variables that increase obesity risk among young adult women. Young adults have rarely been the focus of studies of obesity risk, despite the fact that obesity is increasingly a problem among younger people. It appears that prospective studies examining obesity incidence over time among young adults have not been done. Our study included women without obesity aged 18 to 23 years at baseline who were followed up for almost 20 years for the development of obesity. Variables that might predict the development of obesity were measured at baseline, updated over time, and used as items in an LCA. We then used Cox hazards regression models to examine associations between latent-class membership and subsequent obesity outcomes. Results from the study are expected to contribute to knowledge about risks for the emergence of obesity among an understudied population of young adult women, with implications for prevention efforts tailored to risk profiles.
Methods
Design
We analyzed data from a prospective cohort study, the Australian Longitudinal Study on Women’s Health (ALSWH). Details of the ALSWH objectives, design, participants, and survey methods are described elsewhere (31). Briefly, three cohorts of women (born during the years 1973-1978, 1946-1951, or 1921-1926) were recruited to participate in a long-term prospective study of women’s health in Australia. The current study is limited to women in the younger cohort, born in 1973-978. About 41.5% of women in this cohort who were initially contacted agreed to participate.
Women were initially selected from the national Medicare database, which contains the names and addresses of all Australian citizens and permanent residents. Selection was random, with over-selection for rural and remote areas. Respondents were demographically similar to the general age-specific population in Australia but overrepresented women who were married or employed or had higher education and underestimated immigrant women (32). Surveys were conducted by mail, with additional efforts to contact participants by telephone to encourage participation. The baseline survey was conducted in 1996, and surveys were repeated every 3 years for 7 total administrations.
Participants
The 1973-1978 cohort numbered 14,247 at baseline. Women were excluded from the present study if they reported obesity at baseline (based on reported weight and height converted to BMI ≥ 30 kg/m2; n = 772), if follow-up data on BMI were missing (n = 1,559), if the only follow-up BMI data were collected while the participant was pregnant (n = 1,570), or if the participant provided no data over the follow-up surveys (n = 2,169). The sample for the current study, therefore, included 8,177 women without baseline obesity with follow-up data. Women began participation in 1996 when they were 18 to 23 years old and were followed up approximately every 3 years over 7 total survey administrations to ages 37 to 42 years. Response rates to surveys 2 through 7 for this cohort varied from 68% to 57%.
Measures
We selected nine variables from the baseline survey for inclusion in the LCA. These items were reassessed as time-dependent risks as the survey administrations proceeded. The items were measured at baseline and were updated for each survey administration for participants who did not report obesity, such that the items assessed risk status before the subsequent outcome measure closest in time rather than only at baseline. The nine items measured included income, education, vigorous and moderate physical activity, sleep quality, dietary behavior, depression, stressful events, and social functioning. These were selected to represent recognized obesity-risk variables, as described in the Introduction. We converted each of the items into dichotomous measures for analysis using SAS software version 9.4 PROC LCA (24), which requires categorical variables. Rather than asking for income directly, which generally increases nonresponse rates, income was measured from the item “How do you manage on the income you have available?” Responses were on a five-point scale from “it is easy” to “impossible.” Income was scored as responses 1 to 3 versus 4 to 5. Education was measured on a seven-point scale from “no formal” to “higher degree” and was scored as 1 to 5 versus 6 to 7, dividing participants into those who had or had not completed at least a university education. Physical activity was measured by two items assessing whether the participant engaged in either vigorous or moderate exercise at least once a week for 20 minutes or more. Sleep quality was measured from one item used to rate difficulty sleeping in the last 12 months on a four-point scale that included “never,” “rarely,” “sometimes,” or “often” and was scored as 1 to 2 versus 3 to 4. Poor dietary behavior was estimated from the frequency of eating at fast food restaurants, which was measured on a six-point scale from “never” to “almost every day” and was scored as 1 to 4 versus 5 to 6 or once a week or less versus more than once a week. Stress was measured from survey items assessing the proportion of stressful life events experienced and was converted to scores above and below the median. Social functioning was taken from the Short Form-36 social functioning scale and was dichotomized at the median split. Depression was not assessed in the baseline survey and was included beginning only in the second survey; depression was measured from an item on the second survey that asked, “Have you even been told by a doctor that you have depression (not postnatal) in the last four years?”
We considered additional possible variables for the LCA, including current and former smoking and alcohol consumption, but found in exploratory analyses that they were nonsignificantly related to reduced obesity risk over time. Therefore, these were not included in the LCA models. The outcome measure was obesity during the follow-up period, as measured by self-reported weight and height converted to BMI ≥ 30.
Covariates included baseline BMI, age in years, marital status, parity status, and change in relationship status. Marital status at baseline was dichotomized into married or in a de facto relationship versus other (separated, divorced, widowed, or never married). Change in relationship status identified women who were not married or in a de facto relationship at baseline but who entered such a relationship by the first follow-up; this was a common occurrence among the young women in the sample, and there has been previous ALSWH data suggesting that entering a new relationship can increase obesity risk. Marital status and entering a new relationship were also updated for each survey to assess time-dependent covariates. We identified women who had one or more live births by the end of the follow-up period; women with one or more children are at greater risk for obesity than nonparous women.
Analysis
Descriptive statistics for study variables were found using frequency counts and percentages for categorical variables and means and SDs for continuous variables.
The LCA was performed using SAS software version 9.4 PROC LCA (24). Items for the LCA included the nine dichotomous time-dependent risk indicators described in the Measures section. LCA data were weighted using the area-weighting variable to balance participation from rural and remote regions of Australia. Items with missing data were retained in the model and were imputed within the PROC LCA procedure using full information maximum likelihood estimation under a missing at random assumption (24). Model fit was examined for solutions with two to five classes; model-fit indicators included the Akaike information criterion, Bayes information criterion (BIC), and consistent Akaike information criterion (CAIC). The BIC is often considered as a key indicator of model fit (33). We also considered entropy, the percentage of participants assigned to each class, subjective interpretability, and posterior probabilities. Supporting Information Table S1 provides an example of the SAS code used for the LCA. Once a class solution was selected, each person was assigned to the class of their highest posterior probability, and this categorical variable was used in a subsequent Cox proportional hazards regression model to test for significant associations between each class (with one relatively low-risk class selected as the referent) and risk of obesity over the follow-up. Participants were followed up to the first occurrence of obesity, loss to follow-up, or the end of the follow-up period, whichever occurred first. Finally, to contrast findings from the LCA to what results might indicate using a more traditional analysis, we conducted a Cox model with obesity as the outcome and each of the five covariates (baseline BMI, age, marital status, entering a new relationship, and parity status) and nine risk items as separate independent variables. Missing data on the depression indicator were retained as a categorical level in this analysis because of the common occurrence of missing data on this item.
Results
Table 1 provides a descriptive summary of study variables. We can see, for example, that 21.2% of respondents reported frequent fast food consumption, and 34.5% reported poor sleep. Over the follow-up, 31.5% (n = 2,575) of respondents reported incident obesity. Missing observations were infrequent except for the depression scale; we accounted for missing data on this variable as described in the Methods.
| Frequency | % | |
|---|---|---|
| Low income | ||
| No | 4,110 | 50.4 |
| Yes | 4,045 | 49.6 |
| Missing | 22 | … |
| Low education | ||
| No | 1,586 | 19.5 |
| Yes | 6,561 | 80.5 |
| Missing | 42 | … |
| Low vigorous physical activity | ||
| No | 1,377 | 16.8 |
| Yes | 6,800 | 83.2 |
| Missing | 0 | … |
| Low moderate physical activity | ||
| No | 2,484 | 30.5 |
| Yes | 5,674 | 65.5 |
| Missing | 19 | … |
| Fast food | ||
| No | 6,429 | 78.8 |
| Yes | 1,728 | 21.2 |
| Missing | 20 | … |
| Poor sleep | ||
| No | 5,331 | 65.5 |
| Yes | 2,806 | 34.5 |
| Missing | 40 | … |
| High stressful events | ||
| No | 5,464 | 66.9 |
| Yes | 2,700 | 33.1 |
| Missing | 13 | … |
| Depression | ||
| No | 6,159 | 86.4 |
| Yes | 969 | 13.6 |
| Missing | 1,049 | … |
| Low social functioning | ||
| No | 5,796 | 70.9 |
| Yes | 2,378 | 29.1 |
| Missing | 3 | … |
| Married or in a de facto relationship | ||
| No | 5,508 | 67.5 |
| Yes | 2,652 | 32.5 |
| Missing | 17 | … |
| New relationship | ||
| No | 6,549 | 80.1 |
| Yes | 1,628 | 19.9 |
| Missing | 0 | … |
| Had children | ||
| No | 2,733 | 33.5 |
| Yes | 5,424 | 66.5 |
| Missing | 20 | … |
| Had obesity over follow-up | ||
| No | 5,602 | 68.5 |
| Yes | 2,575 | 31.5 |
| Missing | 0 | … |
| Mean | SD | |
| Age at baseline (missing = 0), y | 20.7 | 1.5 |
| BMI at baseline (missing = 0) | 22.2 | 3.1 |
Model-fit indices are summarized in Table 2. LCA models with two to five classes were examined for model fit and interpretability. We selected a four-class solution, which offered the best fit as measured by a lower BIC and CAIC. The four classes contained between 14% and 30% of participants and had posterior probabilities ranging from 61% to 80%. A five-class solution was considered but contained one class with only 4% of the sample and a poorer BIC and CAIC and offered no simpler or clearer interpretation.
| Class | AIC | BIC | CAIC | Entropy | |
|---|---|---|---|---|---|
| 2 | 1,239.5 | 1,372.6 | 1,391.6 | 0.46 | |
| 3 | 998.1 | 1,201.3 | 1,230.3 | 0.60 | |
| 4 | 826.4 | 1,099.8 | 1,138.8 | 0.50 | |
| 5 | 758.6 | 1,102.0 | 1,151.0 | 0.63 | |
| Class membership, % | |||||
| Class 1 | Class 2 | Class 3 | Class 4 | Class 5 | |
| 2 | 59.9 | 40.1 | … | … | … |
| 3 | 55.4 | 30.3 | 14.3 | … | … |
| 4 | 29.6 | 28.4 | 13.6 | 28.4 | … |
| 5 | 4.3 | 13.5 | 41.5 | 17.5 | 23.2 |
| Posterior probabilities, % | |||||
| Class 1 | Class 2 | Class 3 | Class 4 | Class 5 | |
| 2 | 84.5 | 81.0 | … | … | … |
| 3 | 83.8 | 79.2 | 79.2 | … | … |
| 4 | 69.3 | 80.3 | 80.0 | 61.2 | … |
| 5 | 71.1 | 58.8 | 81.2 | 87.2 | 74.0 |
- AIC, Akaike information criterion; BIC, Bayes information criterion; CAIC, consistent Akaike information criterion.
Figure 1 shows the item probabilities across the four classes. Class 1 (29.6% of the total sample) was labeled the “lower-risk referent” group, with relatively low risk probabilities across most items. Class 2 (28.4%) was labeled “poor diet and exercise” because members of this class had the highest probabilities of low moderate physical exercise and the highest probability of frequent fast food consumption. This group also had the highest probabilities of poor sleep, depression, and low social functioning, although these probabilities were similar to those in class 3. Class 3 (13.6%) was labeled the “stress and psychosocial risk” group. Members of this class had the highest probability of reporting high stressful life events. They were also relatively high on poor sleep, depression, and low social functioning, although not quite as high as class 2. Classes 2 and 3 were similar across many items, but class 3 was characterized by greater life stress and slightly greater socioeconomic disadvantage (low income and education). Class 4 (28.4%) was labeled “multiple intermediate risks.” Members of this group had the highest probability of low education and intermediate probabilities across most other items.
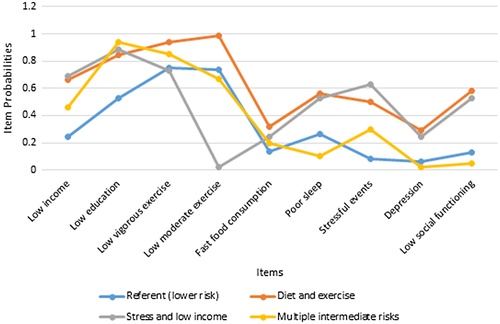
Item probabilities for the two-, three-, and five-class solutions are provided in Supporting Information Figure S1. The two-class solution suggested a split between low- and high-risk profiles. The three- and five-class solutions suggested a lower-risk class and less clear combinations of moderate- and higher-risk classes.
Cox proportional hazards modeling was used to examine associations between class membership for the final four-class solution and obesity over the follow-up. Results are summarized in Table 3. Development of obesity was associated with higher baseline BMI, younger age at baseline, having children, and entering a new relationship. Being married was protective against obesity. Compared with the low-risk referent class, all three of the other classes were associated with a significantly higher obesity risk, including the poor diet and exercise class (hazard ratio [HR] = 1.82; 95% CI: 1.60-2.06), the stress and low-income class (HR = 2.22; 95% CI: 1.92-2.56), and the multiple intermediate risks class (HR = 1.81; 95% CI: 1.60-2.06).
| Variable | HR | 95% CI |
|---|---|---|
| Baseline BMI | 1.38 | 1.37-1.41 |
| Baseline age | 0.93 | 0.90-096 |
| Married | 0.65 | 0.59-0.71 |
| New relationship | 1.39 | 1.26-1.53 |
| Had children | 1.59 | 1.54-1.74 |
| Lower-risk class (referent) | 1.00 | — |
| Poor diet and exercise | 1.82 | 1.60-2.06 |
| Stress and low income | 2.22 | 1.92-2.56 |
| Multiple intermediate risks | 1.81 | 1.60-2.05 |
The Cox model with individual predictors showed that obesity was associated with younger age, entering a new relationship, having children, not being married, and greater baseline BMI, similar to the covariates in the LCA. Obesity was significantly associated with four of the nine items on an individual basis, including low education, lack of vigorous exercise, and stressful life events. Opposite of vigorous exercise, lack of moderate exercise was associated with lower obesity risk (Table 4).
| Variable | HR | 95% CI |
|---|---|---|
| Baseline BMI | 1.38 | 1.36-1.40 |
| Baseline age | 0.96 | 0.93-0.99 |
| Married | 0.71 | 0.64-0.79 |
| New relationship | 1.44 | 1.30-1.59 |
| Had children | 1.43 | 1.30-1.57 |
| Low income | 1.00 | 0.92-1.09 |
| Low education | 2.29 | 2.00-2.62 |
| Low vigorous physical activity | 1.58 | 1.39-1.80 |
| Low moderate physical activity | 0.80 | 0.73-0.87 |
| Fast food consumption | 1.08 | 0.98-1.19 |
| Poor sleep | 1.03 | 0.95-1.13 |
| Stressful events | 1.66 | 1.53-1.81 |
| Depression | 0.99 | 0.87-1.13 |
| Low social functioning | 0.99 | 0.90-1.08 |
Discussion
Women aged 18 to 23 years without obesity at baseline were at higher risk of obesity over approximately 19 years of follow-up in association with three latent classes characterized by different risk profiles. The latent class with the highest point estimate of obesity risk was one characterized by the highest probability of stressful life events and low income and by relatively high risks for low education, poor sleep, depression, and low social functioning. Interestingly, this class was characterized by lowest probabilities of low exercise.
Two other classes were associated with higher obesity risks at almost the same HRs as each other but were characterized by different profiles. The class we labeled “poor diet and exercise,” but that was also characterized by relatively higher probabilities of poor sleep, depression, and low social functioning, had higher obesity risk compared with the referent group, as did the class we labeled “multiple intermediate risks.” This latter group had the highest probability of low education and intermediate probabilities of low income, low exercise, fast food consumption, and stressful events.
Latent classes 2 and 3 had similar profiles, with comparable probabilities on many of the risk items, but one of these classes (class 3, labeled “stress and low income”) had an HR appreciably higher than that of the other classes. What distinguished this class most clearly was a higher probability of greater stressful life events. The stressful life events variable was also strongly associated with obesity in the traditional independent variable analysis. What distinguished higher risk most clearly in class 2 relative to class 3 was lack of exercise. Furthermore, class 3 had the lowest probability of not engaging in moderate exercise, and the lack of moderate exercise in the traditional analysis was actually protective against obesity. We interpret this to indicate that the independent effect of moderate exercise, controlling for vigorous exercise and other risks, identifies people who actually engage in very little physical activity because this measure was based on those reporting as little as one episode per week of moderate activity.
Studies have not previously been reported on prospective obesity risk among young adults, despite the fact that obesity is increasingly a problem among this population. Results of the current study confirmed risk variables that have been identified for other populations, such as low SES, stress, depression, lack of vigorous exercise, and poor eating habits (15, 16, 18, 19). For this young adult population, as well as for others, it remains an important objective to reduce obesity risks and help young adults achieve and maintain healthy weights through behavioral and policy means, as described further below.
In addition to confirming some expected relationships, the LCA provides new insights into possibilities for obesity prevention. Comparison of the latent classes with results from the traditional independent variable analysis revealed both commonalities and contrasts. Stressful life events, lack of vigorous exercise, and low education were identified from the traditional analysis, but other indicators, including poor sleep, low income, and fast food consumption, that helped to contribute to the interpretation of high-risk latent classes were not significantly associated as main effects with obesity risk. Rather than viewing the LCA and the traditional analysis as competitors, it may be useful to examine both approaches to gain deeper insight into how obesity is related to risk variables. We may determine, for example, that depression and stress are important risks. But we also recognize that exposures do not occur in isolation, that women who develop obesity are likely to experience multiple co-occurring exposures, and that there are multiple routes or risk profiles by which obesity may emerge over time.
Consistent with this multiple-exposure perspective, Dietz et al. (34) and Swinburn et al. (35) have called for policy change in efforts to prevent obesity. They argue that the current focus on individual behavioral-change efforts will have limited success and that we must address underlying causes that lead to poor diet and sedentary behavior. These underlying causes address fundamental educational and economic opportunities as well as environmental conditions in which people live that make engaging in healthy behaviors more challenging. As an example, there is easy access to inexpensive “junk food” in most environments that likely contributes to obesity, whereas easy and inexpensive access to lean protein, healthy fats, and complex carbohydrates is not as common. Based on results of the current study, policy changes could include attention to improved educational and economic conditions, both at the individual and neighborhood level, and to improved quality of food options. Better economic conditions, in turn, would help to promote improved psychological health, which could also reduce obesity risk. Tax policies to subsidize fruits and vegetables and make nutritionally poor foods more expensive may also be implemented (36). Health service systems can contribute to dissemination of health promotion messages. Mental health promotion and prevention of depression also remain important goals. Obesity levels continue to pose serious threats to public health despite tremendous efforts from the scientific and public health communities focused on individual behavioral change. The multiple risks that contribute to obesity require responses at multiple points.
Strengths of the study include the large sample, the long-term follow-up period, and the attention paid through the ALSWH to maintain response rates over time. However, a number of study limitations should be recognized. The latent classes were not as well discriminated as we would like, as evidenced by moderate entropy and by partially overlapping risk profiles. The classes sometimes shared common features such as similar class probabilities for depression or low education. There were limitations in available items used to assess exposures. We used only one measure of fast food consumption to estimate poor diet, and alternative measures could be useful. The study was limited to women in Australia and may not by generalizable to men or to other locations. The items were based largely on self-report and may contain reporting bias. Women with overweight or obesity may underreport weight, but the degree of underreporting is usually less than 10%, and self-reported weight is considered to be reasonably reliable and accurate (37). Depression based on self-reported doctor diagnosis may be underestimated as well, although previous research has indicated that self-reported depression is valid compared with a structured clinical interview (38, 39). If reporting biases change over time (e.g., younger women underreport weight more than older women), the associations between baseline risks and follow-up obesity status could be misspecified.
In conclusion, young women without baseline obesity were at risk of developing obesity when they experienced a set of co-occurring risk profiles characterized by combinations of poor behaviors, socioeconomic conditions, or psychosocial risks. Prevention of obesity may benefit from attention to co-occurring risks both with respect to improving efforts at individual behavior change and to larger health policy interventions addressing underlying risks.
Acknowledgments
The research on which this article is based was conducted as part of the ALSWH by the University of Queensland and the University of Newcastle. We are grateful to the Australian Government Department of Health for funding and to the women who provided the survey data.





