Impact of Changes in the Food, Built, and Socioeconomic Environment on BMI in US Counties, BRFSS 2003-2012
Abstract
Objective
Researchers have linked geographic disparities in obesity to community-level characteristics, yet many prior observational studies have ignored temporality and potential for bias.
Methods
Repeated cross-sectional data were used from the Behavioral Risk Factor Surveillance System (BRFSS) (2003-2012) to examine the influence of county-level characteristics (active commuting, unemployment, percentage of limited-service restaurants and convenience stores) on BMI. Each exposure was calculated using mean values over the 5-year period prior to BMI measurement; values were standardized; and then variables were decomposed into (1) county means from 2003 to 2012 and (2) county-mean-centered values for each year. Cross-sectional (between-county) and longitudinal (within-county) associations were estimated using a random-effects within-between model, adjusting for individual characteristics, survey method, and year, with nested random intercepts for county-years within counties within states.
Results
A negative between-county association for active commuting (β = −0.19; 95% CI: −0.23 to −0.16) and positive associations for unemployment (β = 0.17; 95% CI: 0.14 to 0.19) and limited-service restaurants (β = 0.13; 95% CI: 0.11 to 0.14) were observed. An SD increase in active commuting within counties was associated with a 0.51-kg/m2 (95% CI: −0.72 to −0.31) decrease in BMI over time.
Conclusions
These results suggest that community-level characteristics play an important role in shaping geographic disparities in BMI between and within communities over time.
Study Importance
What is already known?
- Previous research using cross-sectional data from the Behavioral Risk Factor Surveillance System (BRFSS) survey has linked obesity to a range of community-level characteristics.
What does this study add?
- Using a random-effects within-between (REWB) model, which is designed to estimate both cross-sectional associations and longitudinal associations, we integrate temporality into the estimation of repeated cross-sectional data, reducing unobserved, time-invariant confounding.
- Our results suggest that a lower percentage of active commuting and a higher percentage of unemployment rates and unhealthy food outlets are linked to higher BMI levels, both between and within communities over time.
Introduction
The prevalence of obesity in the United States has increased rapidly since the 1960s, when approximately 10% of US adults had obesity. An estimated 39.8% of US adults had obesity according to data from the National Health and Nutrition Examination Survey 2015-2016 (1). Until recently, prevention efforts have focused predominantly on addressing individual-level behavioral risk factors. However, studies have shown considerable geographic variation in obesity prevalence across US states and counties (2-7), suggesting variation beyond traditional individual determinants. Estimates from the Behavioral Risk Factor Surveillance System (BRFSS) survey showed that clusters of counties with a high prevalence of obesity (34.6%-47.9%) were found in the South and Midwest, while clusters of counties with a low prevalence of obesity (≤27.3%) were located mostly in the West and Northeast (8). A growing body of research exploring these geographic patterns has linked obesity and its risk factors to a range of neighborhood-level health determinants, including economic context, built environment features, and the community food environment (9-11).
Identifying and measuring the influence of these community-level characteristics has become increasingly important, as they provide potentially impactful targets for policy reform or intervention. To date, a variety of community-level economic indicators (e.g., unemployment) have been linked to higher obesity prevalence at the national level in several cross-sectional studies (8, 12, 13). Economic conditions at state and county levels may influence changes in adult BMI levels through losses in earned income and constraints on household food budgets (12), though some evidence has suggested that extreme forms of economic hardship (e.g., foreclosures) may contribute to food insecurity and decrease obesity risk (14, 15). Furthermore, prior research has suggested that low-income individuals are often exposed to the poorest-quality environments (e.g., poor neighborhood and housing conditions, low street connectivity, lack of safety and social cohesion) (16, 18), which may contribute to socioeconomic disparities in BMI levels.
Other studies have shown that the physical environment influences individual BMI levels, including characteristics related to the built and food environment that shape physical activity and dietary intake (3, 8). For example, individuals living in communities with a higher availability of public transportation options and infrastructure for walking and cycling are more likely to actively commute to work (19) and thus increase caloric expenditure and decrease BMI levels by increasing daily physical activity levels. Previous research has also suggested that inequities in the food environment are linked to poorer diet and higher obesity risk, such as living in a community with an overabundance of inexpensive, less healthy options and limited access to affordable and healthy food items (e.g., food swamps) (9-11).
The evidence linking the physical and social environment to individual BMI levels is based on both experimental research (20) and observational research (21, 22), including ecologic study designs using repeated cross-sectional survey data (8). However, most prior studies using cross-sectional surveys (e.g., BRFFS data) to characterize geographic disparities in weight status have ignored temporality and potential bias from county-level unmeasured confounding and have modeled obesity as opposed to continuous BMI values (8, 12, 17). The present study addressed these gaps by using a random-effects within-between (REWB) model to examine how geographic variability and temporal change in county-level exposures predict variability and change in individual-level BMI values. The REWB model is designed to estimate both cross-sectional associations and longitudinal associations, thereby integrating temporality into the estimation of repeated cross-sectional data (23-25).
The goal of our study was to use an REWB model to examine geographic and temporal trends in individual-level BMI values across US counties between 2003 and 2012, the years for which geographically linked BRFSS data are publicly available. We focused on identifying modifiable community-level determinants to help inform policies that aim to mitigate geographic disparities in obesity prevalence, such as changes to commuting infrastructure or economic incentives to promote the establishment and expansion of grocery stores in underserved communities. To that end, we (1) investigated associations between food, built, and economic contextual factors and geographic differences in BMI levels between US counties as well as their relationship to longitudinal changes in BMI levels within US counties and (2) explored whether these relationships differed by gender and income level.
Methods
Data
The BRFSS is an ongoing, nationally representative, cross-sectional telephone survey of health risk behaviors and preventive health practices of noninstitutionalized civilians aged ≥ 18 years in all 50 US states, the District of Columbia, and participating US territories and other geographic areas (26). The survey is administered by states, and data are aggregated by the Centers for Disease Control and Prevention; participants are selected via random-digit dial. We used data from 2003 to 2012, which included identifiers indicating respondents’ counties of residence for counties with ≥ 50 respondents in a given year.
Outcome
To minimize measurement error and maximize statistical power, we modeled continuous individual-level BMI (vs. categories of obesity) (27, 28). Previous work has also indicated that bias from using self-reported height and weight data is greater when discrete categories of obesity (vs. continuous BMI) are used (29). We calculated BMI (weight in kilograms divided by height in meters squared) using self-reported height and weight data from the BRFSS survey for each survey year from 2003 to 2012.
Exposures
Our selection of modifiable community determinants to examine was shaped by findings from published literature and our participation in The Diabetes LEAD (Location, Environmental Attributes, and Disparities) Network (8, 15, 18, 30). The Diabetes LEAD Network is a Centers for Disease Control and Prevention-funded collaboration between Drexel University, Geisinger-Johns Hopkins University, New York University School of Medicine, and University of Alabama at Birmingham. The primary goal of the network is to examine geographic disparities in diabetes incidence and obesity prevalence across the United States and across demographic groups. The network has identified several potentially modifiable community domains to prioritize, including the social environment, the food environment, and the physical activity environment. Our exposure variables included (1) active commuting, (2) unemployment rate, and (3) the relative availability of limited-service restaurants and convenience stores (separately).
To characterize active commuting, we used decennial census data (1990 and 2000; https://www.census.gov/programs-surveys/decennial-census/data.html) and the American Community Survey (ACS) 2009 to 2013 5-year estimates (https://www.census.gov/data/developers/data-sets/acs-5year.2009.html) to calculate the proportion of total workers aged ≥ 16 years who commute by walking, biking, or using public transportation. We used linear interpolation to estimate active commuting for intercensal years. To characterize the county-level economic environment during our study period, we used the mean annual unemployment rate from the US Bureau of Labor Statistics, which is the annual average estimate of monthly estimates of unemployment for the United States (31). We also used County Business Patterns data from the US Census Bureau (https://www.census.gov/programs-surveys/cbp.html) to characterize the retail food environment at each year. To capture the relative availability of less healthy food options, we calculated the percentage of limited-service restaurants per total restaurants and the percentage of convenience stores per total food stores in each county. Total restaurants included limited-service restaurants (e.g., restaurants providing food services where patrons generally order or select items and pay before eating) and full-service restaurants (e.g., restaurants providing food services to patrons who order and are served while seated), categorized using North American Industry Classification System codes 722211 and 722110, respectively. Total food stores included convenience stores and supermarkets/grocery stores, categorized using North American Industry Classification System codes 445120 and 445110, respectively.
To capture the cumulative exposure of community-level risk factors on individual-level BMI levels (32), we used a moving average lag to characterize our exposure variables. Specifically, we used the mean value over the 5-year period preceding BMI measurement (e.g., we assigned the mean values of exposure variables from 1998 to 2002 to adults with BMI measured in 2003). We assigned the midpoint of the 5-year ACS variables to exposure variables, including variables corresponding to 2007 to 2011 (e.g., 2005-2009 ACS 5-year estimates were used to characterize active commuting in 2007), and we assigned decennial census data and interpolated values to exposure variables in previous years.
Covariates
Additional individual-level variables from BRFSS included age (years), gender (female or male, with no data available about whether respondents were transgender or other), race/ethnicity (Hispanic, non-Hispanic Asian/Pacific Islander, American Indian, or Alaskan Native, black, white, or multiracial), annual household income (continuous in 2012 dollars, using the midpoint of the income categories and $90,000 for the top category), region (Midwest, Northeast, South, West), marital status (currently married, not married), method of survey administration (landline, cell phone), health insurance coverage (yes, no), education (less than high school, high school graduate, some college or technical school, college graduate), number of adults in household, and smoking status (current smoker, former smoker, never smoked). We also used ACS data to calculate county-level population density (quintiles).
Statistical analysis
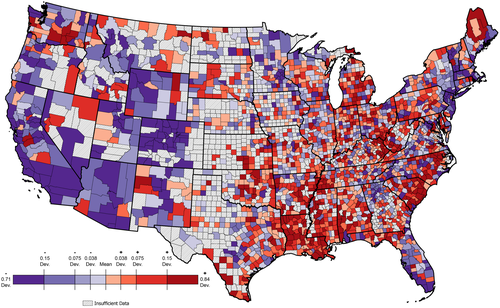
To describe the mean BMI of our study population at the county level independent of secular changes and population aging, we used a hierarchical linear regression model with predictors for age and year and random intercepts for county; we also controlled for method of survey administration to account for changes in data collection format. We plotted the random-effect values to visualize the average deviation of counties from the national expected BMI. To visualize the average deviation of counties from the national expected change in BMI, we added random intercepts for year to an identical model.
To examine both cross-sectional and longitudinal associations between our county-level exposure variables and individual-level BMI, we used a REWB linear model, including nested random intercepts for county-years within counties within states. REWB models, to date more typically employed in political science research, allow for simultaneous estimation of cross-sectional (between-group) and longitudinal (within-group) associations for group-level predictors (23, 33). To estimate a REWB model, we standardized the values for each county-level exposure and then decomposed each variable into the following two new variables: (1) the mean for each county from 2003 to 2012 and (2) the group-mean-centered value for each survey year (county-year value minus county mean). The latter is equivalent to the coefficients estimated by econometric fixed-effects models (i.e., the association between a change in exposure and a change in individual-level BMI within a county), which account for county-level time-invariant confounding (34). We estimated the model using Laplace approximation with the lmer function of the lme4 package in R version 3.5.1 (The R Foundation, Vienna, Austria), which is equivalent to a hierarchical linear regression model (35).
where X1itjk represents an individual-level covariate for person i in county-year t in county j in state k; x is a county-level predictor decomposed into a within-county coefficient,  , and a between-county coefficient,
, and a between-county coefficient,  ; Year represents the BRFSS survey year; and the error terms u, v, w, and ϵ represent the residuals for state, county, county-year, and individual, respectively. The model assumes a normal distribution of the residuals at individual level and the residuals of the outcome.
; Year represents the BRFSS survey year; and the error terms u, v, w, and ϵ represent the residuals for state, county, county-year, and individual, respectively. The model assumes a normal distribution of the residuals at individual level and the residuals of the outcome.
Based on prior literature, we hypothesized that our predictors might have a stronger association with BMI among females and low-income households (3, 30). Therefore, we stratified our models by gender and income (dichotomized by splitting the continuous income variable at the median) in secondary analyses.
Results
The total number of adults in our analytic sample ranged from 196,822 in 2003 to 420,929 in 2011 (n = 3,258,577 in total over the study period), representing 76% of all US counties from 2003 to 2012. Across the study period, the average BMI for the full analytic sample was 27.6 (SD = 5.9) (Table 1). The average BMI of women and men in the sample was 27.3 (SD = 6.4) and 28.0 (SD = 5.1), respectively, and the average BMI of low-income and high-income participants was 28.1 (SD = 6.5) and 27.2 (SD = 5.4), respectively. Controlling for individual-level age, year, and method of survey administration, the counties located in the South and Midwest had the highest average deviation from the national expected BMI (Figure 1), as well as the greatest deviation from the national expected change in BMI (Figure 2).
| Adult participants | BMI | |||
|---|---|---|---|---|
| n or mean | % | Mean | SD | |
| Total sample | 3,258,577 | - | 27.6 | 5.9 |
| Demographic characteristics | ||||
| Age | ||||
| 18-24 | 141,003 | 4.2 | 25.2 | 5.6 |
| 25-34 | 349,428 | 10.3 | 27.0 | 6.1 |
| 35-44 | 521,997 | 15.4 | 27.6 | 6.2 |
| 45-54 | 680,452 | 20.0 | 28.0 | 6.2 |
| 55-64 | 708,820 | 20.9 | 28.3 | 6.1 |
| 65-74 | 543,535 | 16.0 | 27.8 | 5.5 |
| 75-84 | 351,725 | 10.4 | 26.4 | 4.8 |
| ≥ 85 | 100,161 | 3.0 | 24.8 | 4.3 |
| (missing) | 3 | <0.1 | 26.7 | 7.6 |
| Gender | ||||
| Female | 2,079,996 | 61.2 | 27.2 | 6.4 |
| Male | 1,317,128 | 38.8 | 27.9 | 5.2 |
| (missing) | - | - | - | - |
| Race/ethnicity | ||||
| Non-Hispanic white | 2,689,777 | 79.2 | 27.2 | 5.7 |
| Non-Hispanic black | 278,516 | 8.2 | 29.7 | 6.9 |
| Hispanic | 213,049 | 6.3 | 28.1 | 6.1 |
| Non-Hispanic Asian | 65,299 | 1.9 | 24.9 | 4.7 |
| Non-Hispanic Alaskan or Native/Pacific Islander | 38,666 | 1.1 | 28.8 | 6.5 |
| Multiracial | 78,709 | 2.3 | 28.0 | 6.5 |
| (missing) | 33,108 | 1.0 | 27.5 | 6.0 |
| Socioeconomic characteristics | ||||
| Education | ||||
| Less than high school | 315,978 | 9.3 | 28.4 | 6.7 |
| High school | 1,000,571 | 29.5 | 27.9 | 6.1 |
| Some college | 907,480 | 26.7 | 27.8 | 6.1 |
| College/graduate school | 1,166,940 | 34.4 | 26.7 | 5.3 |
| (missing) | 6,155 | 0.2 | 26.7 | 5.7 |
| Income | ||||
| Annual household income (SD) | $52,982 ($31,825) | 87.8 | 26.7 | 5.8 |
| (missing) | - | 12.2 | 27.6 | 5.9 |
| Marital status | ||||
| Married | 1,853,621 | 54.6 | 27.5 | 5.5 |
| Not married | 1,533,361 | 45.1 | 27.5 | 6.4 |
| (missing) | 10,142 | 0.3 | 26.7 | 6.0 |
| Health and health behaviors | ||||
| Smoking | ||||
| Current | 599,045 | 17.6 | 26.9 | 5.9 |
| Ever | 993,990 | 29.3 | 28.0 | 5.8 |
| Never | 1,784,057 | 52.5 | 27.4 | 6.0 |
| (missing) | 20,032 | 0.6 | 27.1 | 5.9 |
| Health insurance | ||||
| Insured | 3,011,713 | 88.7 | 27.4 | 5.9 |
| Uninsured | 377,290 | 11.1 | 27.8 | 6.5 |
| (missing) | 8,121 | 0.2 | 26.5 | 6.3 |
| Weight status | ||||
| Under or normal weight | 1,199,249 | 35.3 | 22.2 | 2.0 |
| Overweight | 1,185,243 | 34.9 | 27.2 | 1.4 |
| Obesity | 874,085 | 25.7 | 35.1 | 5.3 |
| (missing) | 138,547 | 4.1 | - | - |
| Survey design | ||||
| Number of adults in household | ||||
| 1-2 | 2,842,245 | 83.7 | 27.4 | 5.9 |
| 3+ | 418,064 | 12.3 | 27.8 | 6.3 |
| (missing) | 136,815 | 4.0 | 27.5 | 6.2 |
| Sample selection | ||||
| Landline | 3,119,599 | 91.8 | 27.5 | 5.9 |
| Cell phone | 272,565 | 8.0 | 27.7 | 6.1 |
| (missing) | 4,960 | 0.2 | 27.2 | 5.7 |

From 1998-2002 to 2007-2011, the average unemployment rate across all US counties was 6.5% (SD = 2.2%), and the mean percentage of adults actively commuting to work was 4.7% (SD = 4.9%) (Table 2), though only 1.3% of counties had active commuting rates above 10%. The average percentage of convenience stores (per total food stores) and limited-service restaurants (per total restaurants) across all US counties was 43.6% (SD = 13.8%) and 22.9% (SD = 14.7%), respectively, and 9.1% and 1.2% of counties had no convenience stores and no limited-service restaurants, respectively. Based on the REWB model, we observed a negative between-county association for active commuting and BMI (β = −0.19; 95% CI: −0.23 to −0.16) (Table 3). Furthermore, we observed positive between-county associations with BMI for both unemployment (β = 0.17; 95% CI: 0.14 to 0.19) and the percentage of limited-service restaurants (β = 0.13; 95% CI: 0.11 to 0.14). However, the percentage of convenience stores between counties was not statistically significantly associated with BMI (β = 0.02; 95% CI: 0.0004 to 0.05).
| Between-county means (2003-2012) | Mean change (2007-2011 vs. 1998-2002) | |||
|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | |
| Unemployment | ||||
| Unemployed, % | 6.5 (2.2) | 6.3 (5.0 to 7.6) | 2.5 (1.8) | 2.5 (1.3 to 3.7) |
| Food environment | ||||
| Limited-service restaurants, % | 43.6 (13.8) | 45.8 (36.5 to 52.3) | 0.5 (12.1) | 0.7 (−4.3 to 5.6) |
| Convenience stores, % | 22.9 (14.7) | 22.3 (11.7 to 33.2) | −1.7 (15.6) | −0.5 (−10.4 to 6.7) |
| Transportation means | ||||
| Walk, bike, or use public transportation to travel to work, % | 4.7 (4.9) | 3.4 (2.2 to 5.6) | −0.1 (1.5) | −0.1 (−0.6 to 0.4) |
| Primary exposure | β | 95% CI | P |
|---|---|---|---|
| Food environment | |||
| % Limited-service restaurants per total restaurants, mean | 0.13 | 0.11 to 0.14 | <0.001 |
| % Limited-service restaurants per total restaurants, mean difference | 0.03 | −0.004 to 0.06 | 0.09 |
| % Convenience stores per total food stores, mean | 0.02 | 0.0004 to 0.05 | 0.05 |
| % Convenience stores per total food stores, mean difference | 0.03 | 0.01 to 0.06 | 0.01 |
| Active commuting | |||
| Walking, biking, or public transportation, mean | −0.19 | −0.23 to −0.16 | <0.001 |
| Walking, biking, or public transportation, mean difference | −0.51 | −0.72 to −0.31 | <0.001 |
| Unemployment | |||
| Annual unemployment rate, mean | 0.17 | 0.14 to 0.19 | <0.001 |
| Annual unemployment rate, mean difference | - | - | - |
- a Random-effects within-between (REWB) linear model, including nested random intercepts for county-years within counties within states.
- b Model controlled for individual-level age, gender, race/ethnicity, income, region, marital status, method of survey administration, health insurance coverage, education, number of adults in household, smoking status, county-level population density, and survey year (linear). Two-way interaction terms between age, race/ethnicity, gender, and region included.
- c Exposure variables characterized using mean value over 5-year period prior to BMI measurement. Values standardized for each county-level exposure and then variables decomposed into two new variables: (1) mean for each county from 2003 to 2012 and (2) group-mean-centered value for each survey year (county-year value minus county mean).
Between 1998-2002 and 2007-2011, the average percent of participants actively commuting was relatively stable over time (−0.1 percentage points, SD = 1.5) (Table 2). Results from the REWB model indicated that an SD increase in active commuting within counties was associated with a 0.51-kg/m2 (95% CI: −0.72 to −0.31) decrease in BMI over time (Table 3). The average percentage of convenience stores decreased over time (−1.7 percentage points, SD = 15.6), whereas the average percentage of limited-service restaurants increased slightly (0.5 percentage points, SD = 12.1). Model results showed that an SD increase in the percentage of convenience stores within counties was associated with a small increase in BMI (β = 0.03; 95% CI: 0.01 to 0.06). In contrast, the within-county association for an increase in the percentage of limited-service restaurants was not statistically significant (β = 0.03; 95% CI: −0.004 to 0.06).
The average county-level unemployment rate increased by 2.5 percentage points (SD = 1.8) between 1998-2002 and 2007-2011 (Table 2) and increased in 93.6% of counties in general. However, it was not possible to estimate within-county associations for unemployment because of collinearity between the within-county unemployment variable and the linear term for survey year (r = 0.65) and variance inflation factor > 10. The same was true for alternative measures of economic deprivation (e.g., poverty status); thus, we excluded within-county associations for unemployment a posteriori.
Between-county and within-county associations for active commuting were consistent across gender and income strata (Tables 4 and 5). The point estimates for between-county and within-county associations for the effect of convenience stores were relatively larger for low- (vs. high-) income participants, whereas within-county increases in the percentage of limited-service restaurants were positively associated with increases in BMI among high-income participants only. The between-county associations for unemployment did not differ meaningfully by gender or income level. Supporting Information Tables S1 to S3 provide full model estimates, including information regarding random effects.
| Primary exposure | Male | Female | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | P | β | 95% CI | P | |
| Food environment | ||||||
| % Limited-service restaurants per total restaurants, mean | 0.10 | (0.08 to 0.12) | <0.001 | 0.15 | (0.13 to 0.17) | <0.001 |
| % Limited-service restaurants per total restaurants, mean difference | 0.02 | (−0.02 to 0.07) | 0.29 | 0.04 | (−0.01 to 0.08) | 0.11 |
| % Convenience stores per total food stores, mean | −0.002 | (−0.03 to 0.02) | 0.89 | 0.05 | (0.02 to 0.08) | 0.002 |
| % Convenience stores per total food stores, mean difference | 0.03 | (−0.001 to 0.06) | 0.05 | 0.03 | (−0.003 to 0.07) | 0.07 |
| Active commuting | ||||||
| Walking, biking, or public transportation, mean | −0.19 | (−0.23 to −0.16) | <0.001 | −0.18 | (−0.22 to −0.14) | <0.001 |
| Walking, biking, or public transportation, mean difference | −0.18 | (−0.43 to 0.08) | 0.17 | −0.74 | (−1.02 to −0.46) | <0.001 |
| Unemployment | ||||||
| Annual unemployment rate, mean | 0.15 | (0.12 to 0.18) | <0.001 | 0.18 | (0.15 to 0.21) | <0.001 |
| Annual unemployment rate, mean difference | - | - | - | - | - | - |
- a Random-effects within-between (REWB) linear model, including nested random intercepts for county-years within counties within states and stratified by gender.
- b Model controlled for individual-level age, race/ethnicity, income, region, marital status, method of survey administration, health insurance coverage, education, number of adults in household, smoking status, county-level population density, and survey year (linear). Two-way interaction terms between age, race/ethnicity, gender, and region included.
- c Exposure variables characterized using mean value over 5-year period prior to BMI measurement. Values standardized for each county-level exposure and then each variable decomposed into two new variables: (1) mean for each county from 2003 to 2012 and (2) group-mean-centered value for each survey year (county-year value minus county mean).
| Primary exposure | Low income | High income | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | P | β | 95% CI | P | |
| Food environment | ||||||
| % Limited-service restaurants per total restaurants, mean | 0.11 | (0.09 to 0.13) | <0.001 | 0.18 | (0.15 to 0.20) | <0.001 |
| % Limited-service restaurants per total restaurants, mean difference | 0.01 | (−0.03 to 0.05) | 0.69 | 0.06 | (0.01 to 0.10) | 0.01 |
| % Convenience stores per total food stores, mean | 0.04 | (0.01 to 0.07) | 0.004 | 0.01 | (−0.02 to 0.04) | 0.59 |
| % Convenience stores per total food stores, mean difference | 0.04 | (0.01 to 0.07) | 0.02 | 0.02 | (−0.02 to 0.05) | 0.32 |
| Active commuting | ||||||
| Walking, biking, or public transportation, mean | −0.17 | (−0.21 to −0.13) | <0.001 | −0.20 | (−0.24 to −0.17) | <0.001 |
| Walking, biking, or public transportation, mean difference | −0.51 | (−0.79 to −0.22) | <0.001 | −0.35 | (−0.60 to −0.09) | 0.01 |
| Unemployment | ||||||
| Annual unemployment rate, mean | 0.15 | (0.12 to 0.18) | <0.001 | 0.20 | (0.17 to 0.24) | <0.001 |
| Annual unemployment rate, mean difference | - | - | - | - | - | - |
- a Random-effects within-between (REWB) linear model, including nested random intercepts for county-years within counties within states and stratified by income (dichotomized by splitting the continuous income variable at median).
- b Model controlled for individual-level age, gender, race/ethnicity, region, marital status, method of survey administration, health insurance coverage, education, number of adults in household, smoking status, county-level population density, and survey year (linear). Two-way interaction terms between age, race/ethnicity, gender, and region included.
- c Exposure variables characterized using mean value over 5-year period prior to BMI measurement. Values standardized for each county-level exposure and then each variable decomposed into two new variables: (1) mean for each county from 2003 to 2012 and (2) group-mean-centered value for each survey year (county-year value minus county mean).
Discussion
In this study, we employed an innovative multilevel model using 10 years of individual-level BRFSS data and publicly available county-level contextual data to assess relationships between a select group of county-level determinants and BMI using both between-county (cross-sectional) and within-county (temporal change) estimates. Similar to econometric fixed-effects models, our modeling strategy provides stronger support for causal inference by reducing unobserved, time-invariant confounding. Though our findings were substantively similar to previous works, most prior studies have used standard multilevel regression models that ignore potential confounding by using a single cross section of data (3, 12, 36) or ignore temporality by pooling multiple years of cross-sectional data (37, 38); however, we integrated temporality into the estimation of repeated cross-sectional data, which allowed us to capture longitudinal associations within counties over time.
Substantively, our results showed that increases in active commuting (i.e., walking, biking, or using public transportation) within US counties were associated with meaningful decreases in BMI levels over time. This finding provides more robust evidence for an effect of active commuting than traditional cross-sectional multilevel models (12). The direction and magnitude of our findings are corroborated by previous studies showing that higher levels of active travel and physical activity are associated with lower BMI levels and obesity prevalence across US counties (8, 12). Higher rates of active travel to work are associated with higher rates of physical activity (39), which mitigate obesity risk, potentially via increases in caloric expenditure. Prior research also indicates that individuals who reside in areas with higher walkability and cycling infrastructure are more likely to engage in active commuting (39). Thus, our findings support expansion and improvement in walking and cycling infrastructure (e.g., bike paths), as well as land use policies that increase active travel (e.g., mixed-use development).
Based on between-county estimates, we also found that higher rates of unemployment were associated with higher BMI levels, consistent with previous multilevel modeling studies showing links between obesity and county-level unemployment rates and other measures of economic deprivation (e.g., county poverty rates) (8, 12, 15). Two hypothesized mechanisms by which unemployment influences weight status are economic deprivation and social deprivation. Higher levels of unemployment and poverty at the community level may be linked to constrained household food budgets and may encourage excess intake of energy-dense, nutrient-poor foods, which are relatively less expensive than healthy food items (40). Furthermore, area-level deprivation may be linked to differences in social norms regarding obesity as well as fewer opportunities for physical activity and recreation (41). This highlights the importance of promoting and funding efforts to increase the affordability of healthy foods for low-income individuals (e.g., the Supplemental Nutrition Assistance Program) and mitigating social deprivation (e.g., increasing the adequacy of infrastructure).
Our results also suggest that the county-level food environment profile plays a role in shaping obesity risk. Notably, among low-income participants, the increases in the relative availability of convenience stores were associated with increases in BMI within counties over time, whereas increases in the relative availability of limited-service restaurants were associated with increases in BMI among high-income participants. Findings across previous studies of the food environment, most of which used ecologic analyses, have not been consistent, with contradictory or null findings, regardless of whether the food environment was characterized using absolute measures (e.g., density) (8, 12) or relative measures (e.g., ratio, index) (3, 8, 12, 36). For example, a study by Myers et al. (8) used BRFSS weight data from 2004 and 2009 to estimate associations between a suite of community exposures and change in age-adjusted adult obesity prevalence across US counties. Their results suggest that increases in both grocery store/supercenter density and food restaurant density are associated with decreases in obesity prevalence, the latter of which is contrary to expectations. However, the authors used model-based estimates of BMI, which may not reflect variation caused by county-level factors (42), and the mismatch between baseline exposure values (2000) and baseline obesity prevalence (2004) may have resulted in a misrepresentation of the etiologic period. These issues are common to the majority of studies using ecologic data, including ignoring temporal variation from year to year (3, 8, 12, 36).
Though the effect size of estimates varied, most were similar or larger than most obesity intervention studies focused on individuals (43). For example, the observed effect size of 0.5 kg/m2 for the county-level proportion of total workers who actively commute is equivalent to approximately 3.5 lb and 2.9 lb for the average male participant (70.1 in, 195.1 lb) and the average female participant (64.3 in, 159.5 lb), respectively, in the BRFSS sample. Furthermore, even small decreases in BMI confer health benefits, especially in the context of a multipronged approach to changing environmental determinants of obesity. Policies and programs that target multiple population-level risk factors at once may contribute to even greater weight loss, such as funding for improving cycling infrastructure, which may provide employment opportunities as well as increase physical activity at the population level.
Our study has several limitations. Most notably, our individual-level BRFSS data were not longitudinal, so we are prone to bias from selection into residential settings; however, our use of lagged exposures minimizes this bias. Though we are also prone to bias because of missing data, we did not observe a substantial difference in the average BMI for participants with complete data (27.6) versus missing data (27.0). Our BMI outcome data were self-reported, making them vulnerable to measurement error, and nonresponse and noncoverage in the BRFSS survey may bias results and reduce generalizability. We were also not able to estimate within-county associations for unemployment because of near-universal increases in county-level unemployment over time, which resulted in collinearity between unemployment and survey year. In addition, the scale of our exposures may have been too large to appropriately capture the impact of area-level contextual factors on weight status, and county boundaries may change over time. Indeed, findings from the United States Department of Agriculture’s National Household Food Acquisition and Purchase Survey indicate that the average distance to an individual’s primary food store (3.4 miles) is smaller than the average size of a US county (44). Regardless, our approach to estimating between- and within-county associations represents a significant improvement on the majority of national studies of geographic disparities in BMI and obesity prevalence.
Conclusion
The results of this study show that a lower percentage of active commuting and a higher percentage of unemployment and unhealthy food outlets are linked to higher BMI levels, suggesting that these community-level characteristics play an important role in shaping geographic disparities in weight status. Overall, our study design offers certain advantages over previous studies, including maximizing temporal information and accounting for potential bias from time-invariant confounding. In future studies, it is critical to identify the extent to which policy changes to modifiable county-level risk factors, in combination or isolation, are linked to differences in weight status over time.
Acknowledgments
We would like to acknowledge Andrew Vinson for his support in creating maps to visualize the data and Samrachana Adhikari for her critical review of the manuscript.





