Healthcare Professionals' Job Satisfaction and Its Determinants in Ethiopia: A Systematic Review and Meta-Analysis
Funding: The authors received no specific funding for this work.
ABSTRACT
Aim
This study targeted to determine the aggregated prevalence and determinants of job satisfaction of healthcare professionals in Ethiopia.
Design
A systematic review and meta-analysis.
Methods
Literature has been systematically searched from databases like PubMed, Hinari, Science Direct, Google Scholar, Scopus and Web of Science. Data were collected using Microsoft Excel and STATA 16 version was used for analysis. The I2 statistic was used to determine the significance of homogeneity. A 95% confidence interval with adjusted odds ratios (AOR) was used to show association.
Results
The aggregated prevalence of job satisfaction of healthcare professionals in Ethiopia was found to be 43.42%. Being married, having good recognition, having good remuneration, having adequate supervision and having good work security were positively associated with job satisfaction.
Patient or Public Contribution
No patient or public contribution.
Conclusion
This study showed poor job satisfaction among healthcare professionals in Ethiopia. Therefore, strategies have to be designed to increase the level of satisfaction by all stakeholders.
1 Introduction
Healthcare professionals are paramount important in the healthcare system as they have great roles and responsibilities in ensuring the well-being of the patients and community at large (Engum and Jeffries 2012; Pillay 2009). Globally, the well-being of healthcare providers and their feelings about their job are important in securing quality healthcare for mankind (Bridgeman et al. 2018; Güler et al. 2019; Kang et al. 2020). As Ethiopia is among the developing countries, it is not deniable that its healthcare system is subjected to challenges (Kitaw et al. 2020; Woldemariam et al. n.d.).
The job satisfaction of healthcare professionals is indicating the feeling and beliefs that healthcare professionals have about their job (Goetz et al. 2015). A favourable attitude toward the job indicates job pleasure, while an opposed attitude toward the job indicates job disappointment. It is among the important variables that could be used to measure the quality of healthcare systems (Okoli et al. 2020; Ruiz-Fernández et al. 2020).
Job satisfaction could be measured by different components such as monthly payments like salary, working situation, prospects for personal and professional development, a manageable amount of work, presence of positive regulation, relationships and recognition, patient care outcomes, autonomy and contingent rewards (Okoli et al. 2020; Ramasodi 2012). If an individual is not satisfied with his/her job, he/she will be subjected to stress, absenteeism and intention to leave (Hooker et al. 2015).
Having highly satisfied healthcare professionals will contribute positively to the healthcare system of a country as it will lead to better performance and better patient outcomes (Thiagaraj and Thangaswamy 2017). Unsatisfied healthcare professionals will not work properly and will not stay in their profession (Kols et al. 2018). Addressing such a problem might be very difficult in a country like Ethiopia where there is no adequate work task force due to many factors (Debela et al. 2017).
Studies show the prevalence of health professionals' job satisfaction varies from 32% (Temesgen et al. 2018) to 61% (Ayalew et al. 2019). It is about 50% in Sudan (Suliman et al. 2017), and 18% in Pakistan (Tasneem et al. 2018). Varied reports from previous studies on prevalence and especially predicting factors of healthcare professionals' job satisfaction were the main reasons to trigger this study (Abate and Mekonnen 2021; Girma et al. 2021). This systematic review and meta-analysis aimed to estimate the pooled prevalence and associated factors of job satisfaction in Ethiopia.
2 Methods
2.1 Study Setting and Search Strategies
The current study was conducted to determine the aggregated prevalence and determinants of job satisfaction of healthcare professionals in Ethiopia. It is reported as per the established standard which is Preferred Reporting Items for Systematic and Meta-analysis (Page et al. 2021). CoCoPop (Condition: job satisfaction; Context: Ethiopia; and Population: healthcare professionals) was used to find eligible studies. It is a recommended tool for systematic review of prevalence studies (Munn et al. 2014). Potential studies were identified through a search in PubMed, Hinari, Science Direct, Google Scholar, Scopus and Web of Science databases. Cross-references and links were used to additionally search potential studies. English language restriction was employed to include studies. The clerking of databases was done from 23 to 26 February 2022. Medical subject heading (MeSH) terms of Healthcare professionals AND Job satisfaction AND Ethiopia were used in different combinations. Free full text, human species and studies conducted from 2010 to 26 February 2022 were used to narrow potential studies to be included. The research registry registration was done with registry identification of reviewregistry1648 and it can be accessed by the following link: https://www.researchregistry.com/browse-the-registry#registryofsystematicreviewsmeta-analyses/registryofsystematicreviewsmeta-analysesdetails/648060ea133ae2002803a021/.
2.2 Inclusion Criteria
The inclusion criteria were original studies reported the prevalence of job satisfaction and/or studies reported determinants of job satisfaction, studies published in English from Ethiopia from 1 January 2010 to 26 February 2022.
2.3 Exclusion Criteria
Studies that failed to report outcome variables were excluded. Studies whose full texts were not available and were unable to receive full text from the authors within 2 weeks were excluded.
2.4 Study Selection and Data Collection
Database search results were combined, and duplicate articles were removed using Endnote (Version 8) and manually. The eligibility assessment was performed independently by four reviewers (D.T., D.Z., S.H. and E.F). Discrepancies between the four reviewers in this process were discussed with the review team until a consensus was reached. Articles identified through electronic literature searches and from other sources were comprehensively reviewed based on the eligibility criteria for inclusion.
2.5 Outcome Measurement
The aggregated prevalence and determinants of job satisfaction of healthcare professionals in Ethiopia were our variables of interest.
2.6 Quality Assessment and Data Extraction
The modified Newcastle–Ottawa appraisal assessment tool (Peterson et al. 2011) was used to evaluate the quality of the studies. Three authors (D.T., B.C. and E.F.) evaluated the quality of included studies independently. The disagreements arising were resolved by evaluating and discussing with the three authors together. Accordingly, all included studies in this study were graded as high quality, which means they scored ≥ six out of nine (Table 1).
| First author, publication year | Study area | Study design | Study population | Sample size | Satisfaction (%) | Quality status |
|---|---|---|---|---|---|---|
| Ayalew et al. (2019) | Bahir Dar | Cross-sectional | Nurses | 220 | 43.6 | High quality |
| Ayalew et al. (2019) | In all public health facilities of Ethiopia | Cross-sectional | Nurses | 424 | 60.8 | High quality |
| Ayele et al. (2020) | In public hospitals located in eastern Ethiopia | Cross-sectional | Pharmacists | 220 | 32.7 | High quality |
| Bekru et al. (2017) | In health facilities in Addis Ababa city | Cross-sectional | Midwives | 221 | 52.9 | High quality |
| Deriba et al. 2017 (32) | At public health centers in West Ethiopia | Cross-sectional | All Healthcare professionals | 308 | 41.46 | High quality |
| Gedif et al. (2018) | At the University of Gondar Referral Hospital, Northwest Ethiopia | Cross-sectional | All Healthcare professionals | 383 | 54 | High quality |
| Geleto et al. 2015 (34) | At public health institutions in Harari region, eastern Ethiopia | Cross-sectional | All Healthcare professionals | 405 | 44.2 | High quality |
| Merga and Fufa (2019) | In Bale Zone Public Health Facilities, eastern Ethiopia | Cross-sectional | All Healthcare professionals | 422 | 38.5 | High quality |
| Semachew et al. (2017) | In Ethiopian public hospitals | Cross-sectional | Nurses | 316 | 68.4 | High quality |
| Temesgen et al. 2018 (18) | At Western Amhara Region of Ethiopia | Cross-sectional | All Healthcare professionals | 575 | 31.7 | High quality |
| Yami et al. (2011) | In Jimma university specialised hospital, southwest Ethiopia | Cross-sectional | All Healthcare professionals | 145 | 41.4 | High quality |
| Yilkal Fentie et al. (2018) | In Amhara National Regional State, Northwest Ethiopia | Cross-sectional | Anaesthetists | 98 | 46.9 | High quality |
Year of publication along with author's name, study (quality, area, design and sample size) and main findings of the studies like the magnitude of job satisfaction and its determinants were extracted. Searching results and their references are reviewed by seven authors (D.T., M.C., M.H., W.A., D.M., B.G. and E.F.) independently. The disagreements arising to include studies were resolved by evaluating and discussing with all authors.
2.7 Statistical Analysis
The Microsoft Excel spreadsheet and STATA version 16.0 software were used for data management. The aggregated prevalence of job satisfaction and its determinants were analysed by the ‘Der Simonian and Laird random-effects meta-analysis (random-effects model)’ (Kelley and Kelley 2012). The aggregated adjusted odds ratios with a 95% confidence interval for associated factors of included studies were computed. Forest plots and tables were used to depict the findings.
2.8 Heterogeneity and Publication Bias
The I2 statistic test was done to determine the heterogeneity of included studies (Deeks et al. 2019). The finding was highly heterogeneous (heterogeneity I2 > 75%). To minimise heterogeneity and identify its source, subgroup analyses were done. Again, to differentiate the outlier articles, sensitivity analysis was done. The funnel plot, Egger test and p-value < 0.05 were employed to declare publication bias (Peters et al. 2006).
3 Results
3.1 Search Strategy
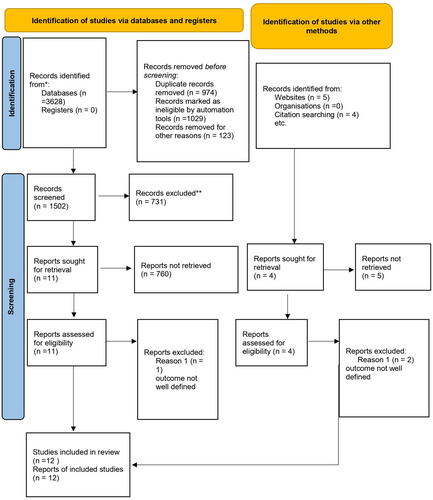
In the current study, published articles on the prevalence and associated factors of job satisfaction in Ethiopia were included. An overall of 3628 articles were found as a search result. In total, 1502 articles after similar studies were removed were further screened and 1487 articles were excluded. Only 15 articles were left and three research studies were excluded for reasons. Finally, 12 were used for qualitative and quantitative synthesis (Moher et al. 2009) (Figure 1).
3.2 Characteristics of Included Studies
This study used 12 studies with a total number of 3736 healthcare professionals. The job satisfaction among the included studies varied from 31.7% (Temesgen et al. 2018) to 68.4% (Semachew et al. 2017). Regarding study design, only cross-sectional design was employed. Furthermore, concerning the study population, six studies were conducted on all healthcare professionals, while the remaining three studies were conducted on nurses. A single study focused on pharmacists, midwives and anaesthetists (Table 1).
3.3 Meta-Analysis
3.3.1 Publication Bias
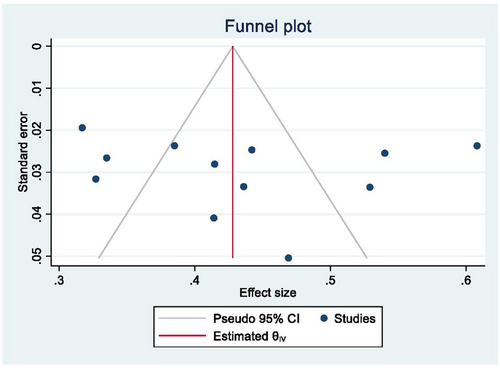
A funnel plot (Figure 2) and Egger's regression test (Peters et al. 2006; Sterne et al. 2005) depicted that there was no publication bias seen between the studies (egger's regression test p-value =0.7497).
3.3.2 The Aggregated Prevalence of Job Satisfaction Among Healthcare Professionals
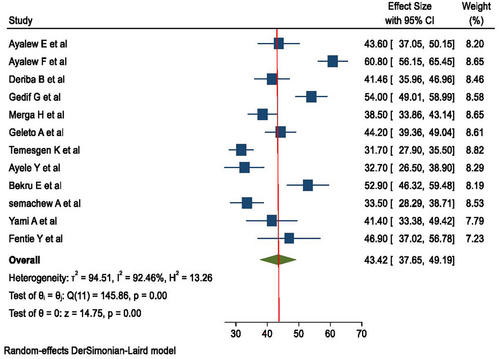
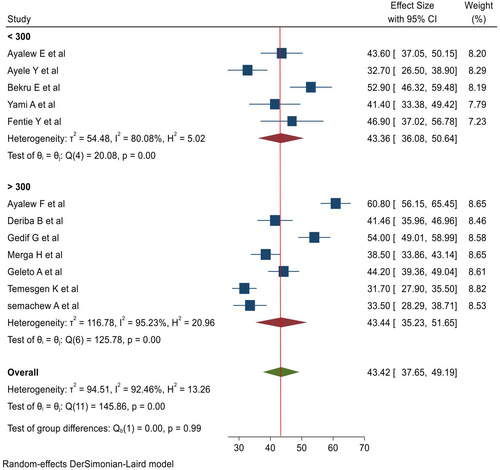
The pooled prevalence of satisfaction in this study was found to be 43.42% with 95% CI (37.65, 49.19). Heterogeneity was significant across the included studies (I2 = 92.46%, p = 0.00) (Figure 3).
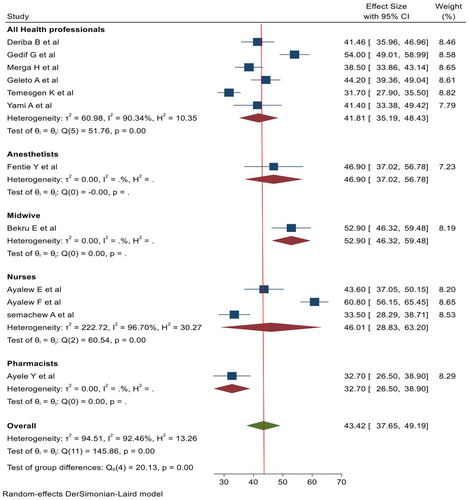
3.3.3 Subgroup Analysis
Subgroup analysis was done by using the type of healthcare professionals (nurses, midwives, pharmacists, anaesthetists, and all healthcare professionals) and sample size. The highest proportion of job satisfaction was observed in studies that had a sample size of > 300, with 44.44% and a CI of (35.23, 51.65) (Figure 4). Based on the type of profession, the highest proportion of job satisfaction was seen in midwives, with a proportion of 52.90% (46.32, 59.48), and the lowest proportion of job satisfaction was seen in pharmacists, 32.70% (26.50, 38.90) (Ayele et al. 2020). The pooled prevalence of job satisfaction in studies that include all healthcare professionals was 41.81% (35.19, 48.43), and the pooled prevalence of job satisfaction in studies that include only nurses was 46.01% (28.83, 63.20) (Figure 5).
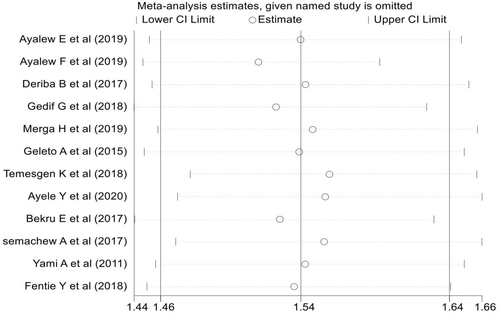
3.4 Sensitivity Analysis
There was no single study that significantly affected the overall estimate (Figure 6).
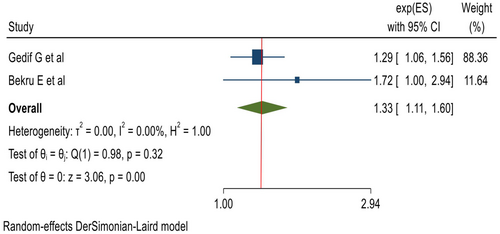
3.4.1 The Effect of Marital Status on the Pooled Estimate of Job Satisfaction of Healthcare Professionals
Two of the overall 12 studies reported the significance of marital status on the satisfaction of healthcare professionals. Further, the combined effect sizes of these two different studies (Bekru et al. 2017; Gedif et al. 2018) showed that married healthcare professionals were 1.3 times more likely to be gratified compared to those who were not married (AOR: 1.33; 95% CI: 1.11, 1.60), (I2 = 0.0%, p = 0.322) (Figure 7).
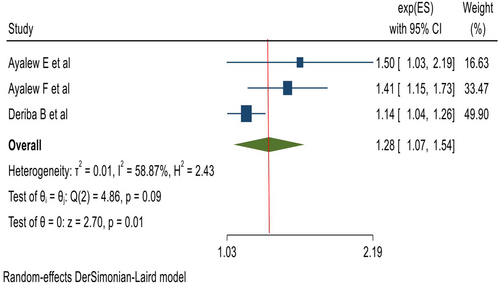
3.4.2 The Effect of Recognition on the Pooled Estimate of Job Satisfaction of Healthcare Professionals
Three (Ayalew and Workineh 2019; Ayalew et al. 2019; Deriba et al. 2017) studies reported the significance of recognition on the job satisfaction of healthcare professionals. Having good recognition was positively associated with job satisfaction in healthcare professions as compared with its counterpart (AOR: 1.28; 95% CI: 1.07, 1.54), (I2 = 58.9%, p = 0.088) (Figure 8).
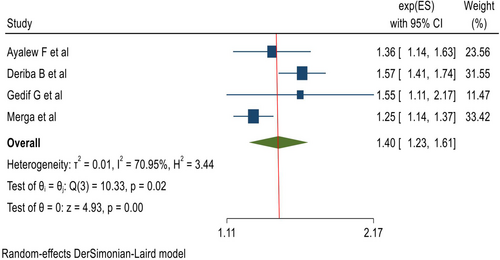
3.4.3 The Effect of Remuneration on the Pooled Estimate of Job Satisfaction of Healthcare Professionals
Four studies reported the significance of recognition on the job satisfaction of healthcare professionals. The pooled effect sizes of these four different studies (Ayalew et al. 2019; Deriba et al. 2017; Gedif et al. 2018; Merga and Fufa 2019) showed that having good remuneration is significantly associated with job satisfaction (AOR: 1.40; 95% CI: 1.23, 1.61), (Figure 9).
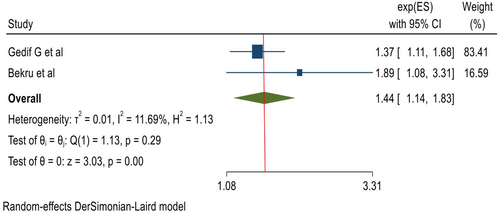
3.4.4 The Effect of Supervision on the Pooled Estimate of Job Satisfaction of Healthcare Professionals
From random-effects model estimates, the pooled odds of having adequate supervision among healthcare professionals were 1.4 times more likely to be satisfied compared to their counterparts (AOR: 1.44, 95% CI, 1.14, 1.83), (Figure 10).
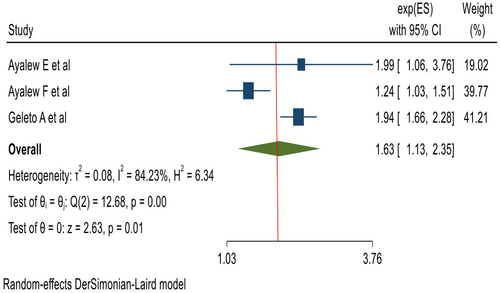
3.4.5 The Effect of Work Security on the Pooled Estimate of Job Satisfaction of Healthcare Professionals
Having good work security of the participant has a significant effect on healthcare professionals' satisfaction. Those participants having good work security were 1.6 times more likely to be satisfied as compared to those who did not have good work security (AOR: 1.63 95% CI, 1.13, 2.35) (Figure 11).
3.4.6 The Effect of Work Experience on the Pooled Estimate of Job Satisfaction of Healthcare Professionals
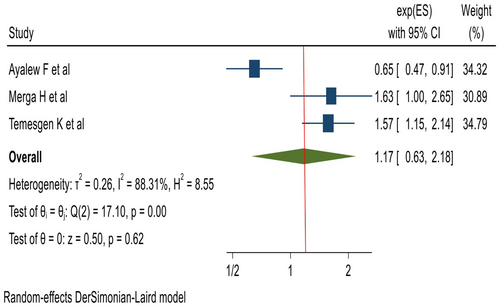
From random-effects model estimates, the work experience was not associated with job satisfaction of healthcare professionals (AOR: 1.17 95% CI, 0.63, 2.18) (Figure 12).
3.4.7 The Effect of Workload on the Pooled Estimate of Job Satisfaction of Healthcare Professionals
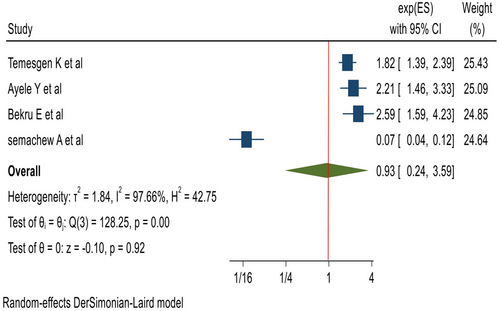
From random-effects model estimates, the workload was not associated with the job satisfaction of healthcare professionals (AOR: 0.93 95% CI, 0.24, 3.59), (Figure 13).
3.4.8 The Effect of Working Unit on the Pooled Estimate of Job Satisfaction of Healthcare Professionals
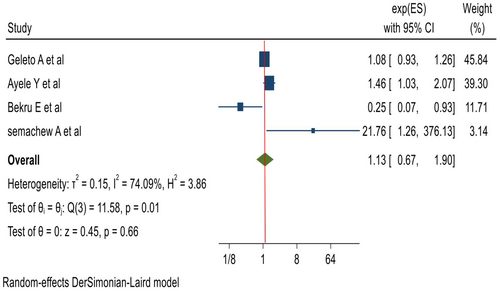
From random-effects model estimates, the working unit was not associated with the job satisfaction of healthcare professionals (AOR: 1.13 95% CI, 0.67, 1.90) (Figure 14).
4 Discussion
This study was conducted to estimate the aggregated prevalence of job satisfaction of healthcare professionals and associated factors in Ethiopia. The aggregated prevalence of job satisfaction was 43.42% (95% CI: 37.65, 49.19). The pooled prevalence of job satisfaction among healthcare professionals in this study was in line with the studies done in Iran 43.6% (Amiresmaili and Moosazadeh 2013) and in Sudan 41% (Suliman et al. 2017). This low level of job satisfaction might be due to workload, poor leadership quality, poor work–life balance, poor relationship with colleagues or supervisors and poor motivational factors including incentives.
The finding of this study was higher than studies done in Korea 28.1% (Park and Lee 2018) and Pakistan 18% (Tasneem et al. 2018). This might be due to differences in the study population (nurses only) and a small sample size of only 256 in Korea and Pakistan as compared to the current study. While the findings of this study are lower than the study done in Nepal 76% (Chaulagain and Khadka 2012), the discrepancy might be due to the variation in health policy and economic status; as Nepal has a better economy, they may invest more in the health sector and health professionals.
The pooled prevalence of job satisfaction among healthcare professionals in Ethiopia by professions was 53% in midwives (Bekru et al. 2017), 42% in studies that include all healthcare professionals (Deriba et al. 2017; Gedif et al. 2018; Geleto et al. 2015; Merga and Fufa 2019; Temesgen et al. 2018; Yami et al. 2011), 47% in anaesthetists (Yilkal Fentie et al. 2018), 46% in nurses (Ayalew and Workineh 2019; Ayalew et al. 2019; Semachew et al. 2017) and 33% in pharmacists (Ayele et al. 2020). The higher pooled prevalence of job satisfaction among healthcare professionals in Ethiopia by sample size category was observed in studies that had a sample size greater than 300 (Ayalew and Workineh 2019; Deriba et al. 2017; Gedif et al. 2018; Geleto et al. 2015; Merga and Fufa 2019; Semachew et al. 2017; Temesgen et al. 2018) was 43% with a CI of (35, 52).
This meta-analysis showed that being married, healthcare professionals, having good recognition, good remuneration, adequate supervision and good work security were positively associated with job satisfaction of healthcare professionals as compared to their counterparts, while working unit and workload failed to associate with job satisfaction. This result is in line with studies done in Pakistan, Nepal and Australia (Chaulagain and Khadka 2012; Kluger et al. 2003; Tasneem et al. 2018). This similarity might be due to having good recognition, good remuneration, adequate supervision and good work security creating good motivation for staff that leads to good working conditions and satisfaction. This result is not similar to studies done in Serbia and South Africa (Kuburović et al. 2016; Ramasodi 2012). The dissimilarity might be due to differences in equipping health sectors, as these countries have better socio-economic status than Ethiopia.
4.1 Limitation
The limitation of this study is that all included studies employed a cross-sectional study design, and there is also significant heterogeneity among included studies, which might cause difficulty in establishing a temporal relationship between the healthcare professionals' job satisfaction and its determinants.
5 Conclusion
Poor healthcare professional job satisfaction has to be strategically halted by all stakeholders as the finding of this systematic review and meta-analysis showed a low level of job satisfaction which is less than 50%. It would be very difficult to have a productive health professional without maintaining their satisfaction with their job.
Author Contributions
All authors substantially performed the literature search, assessment of articles, data extraction, statistical analysis and manuscript preparation. All authors reviewed the manuscript and agreed to publication.
Acknowledgements
Debre Tabor University for providing internet service.
Ethics Statement
The authors have nothing to report.
Consent
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.