Roles and challenges encountered by midwives in the management of postpartum haemorrhage following normal vaginal delivery: A scoping review
Abstract
Aims
To establish a comprehensive understanding of the roles of midwives and the challenges they encounter in the prevention, diagnosis and management of postpartum haemorrhage (PPH) following normal vaginal delivery.
Design
We conducted a scoping review following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis for Scoping Reviews (PRISMA-ScR) recommendations.
Methods
We considered studies related to the roles of midwives and the challenges they encounter in the prevention, diagnosis and management of PPH during vaginal delivery. We excluded guidelines, consensuses, abstracts of meetings and non-English language studies. Databases, including the Cochrane Library, PubMed, Web of Science, Ovid, Medline, Embase, JBI EBP and BIOSIS Previews, were searched on January 1, 2023, with no time limitations.
Results
We included 28 publications. Midwives play important roles in the prevention, diagnosis and management of postpartum haemorrhage during vaginal delivery. In the prevention of PPH, midwives' roles include identifying and managing high-risk factors, managing labour and implementing skin-to-skin contact. In the diagnosis of PPH, midwives' roles include early recognition and blood loss estimation. In the management of PPH, midwives are involved in mobilizing other professional team members, emergency management, investigating causes, enhancing uterine contractions, the repair of perineal tears, arranging transfers and preparation for surgical intervention. However, midwives face substantial challenges, including insufficient knowledge and skills, poor teamwork skills, insufficient resources and the need to deal with their negative emotions. Midwives must improve their knowledge, skills and teamwork abilities. Health care system managers and the government should give full support to midwives. Future research should focus on developing clinical practice guidelines for midwives for preventing, diagnosing and managing postpartum haemorrhage.
1 INTRODUCTION
Postpartum haemorrhage (PPH) accounts for the highest number of maternal deaths globally, comprising 27% of total maternal deaths (World Health Organization [WHO], 2023). PPH refers to blood loss greater than 500 mL after vaginal delivery within the first 24 h. Eighty percent of PPH cases occur within 2 h of delivery and are accompanied by signs or symptoms of hypovolemia (Wormer et al., 2023). The incidence of PPH after vaginal delivery is 3.2% in the United States (Reale et al., 2020), 16% in Nepal (Sharma & Dhakal, 2018) and 10.4% in China (Wei et al., 2020). PPH can result in complications such as hypovolemic shock, disseminated intravascular coagulation, acute respiratory distress syndrome, acute renal failure and decreased fertility; it can also cause long-term psychological effects such as fear, depression and post-traumatic stress disorder, resulting in serious challenges and economic burdens in the global public health sector (American College of Obstetricians and Gynecologists [ACOG], 2017; WHO, 2023). However, most cases of PPH are avoidable or potentially preventable, with the key lying in scientific management. The WHO has recommended a midwife-led continuity of care model (Tuncalp et al., 2017), and studies show that the midwife-led care model can reduce the incidence of PPH (Kalu & Chukwurah, 2022; Zhang et al., 2021).
The International Confederation of Midwives (ICM) issued a joint statement stressing that midwifery plays important roles in promoting reproductive health and ensuring the safety of mothers and infants (Nove et al., 2018). The Lancet Series on Midwifery concluded that midwives could avert about 70% of maternal or infant deaths (Renfrew et al., 2014). Midwives are often the first-line professionals in quantifying blood loss, initiating the early diagnosis of PPH and mobilizing a team response if necessary (Natrella et al., 2018). Multiple government agencies have released guidelines for preventing, treating and managing PPH, but these are applicable to all health care personnel and do not explicitly address the role of midwives (ACOG, 2017; Queensland Health, 2023; WHO, 2023). Renfrew et al. (2014) developed a framework for quality maternal and newborn care and examined effective and ineffective practices in midwifery, from pre-pregnancy and pregnancy to birth and postpartum. However, effective PPH practices only included the use of medications (Renfrew et al., 2014). Another study indicated that in the management of PPH, midwives must assess and intervene as early as possible or during the haemorrhage, initiating emergency treatment or calling for help; however, that study lacked specific descriptions (Mamakou, 2020). Emergency personnel in PPH include obstetricians, anaesthesiologists, midwives, nurses and laboratory personnel. However, in many countries, no clear professional distinction exists between midwives and nurses (Nove et al., 2021). This leads to midwives lacking a clear understanding of the role they play in different settings, hindering the quality of interprofessional communication and collaboration in daily clinical practice (Maier & Aiken, 2016). This situation further affects the success rate of treating PPH and poses challenges to the management of PPH. In addition, midwives' professional qualifications, clinical experience, knowledge level, age, working years and education level are closely related to the prevention and management of PPH (Muthoni et al., 2021; Ramadhani et al., 2020; Voillequin et al., 2022; Wake & Wogie, 2020). Although some studies have investigated the challenges related to PPH, there are no systematic reviews on this topic in particular.
Thus, we conducted a review of the roles of midwives and the challenges faced by them in preventing, diagnosing and managing PPH based on scope to provide a basis for clinical midwifery management, reduce the incidence of PPH and put forward prospects and suggestions for the development of midwives in their professional field.
2 AIM
In this study, we aimed to acquire a comprehensive understanding of the roles of midwives and the challenges faced by them in the prevention, diagnosis and management of PPH following normal vaginal delivery.
3 METHODS
A scoping review was conducted following PRISMA-ScR recommendations (Tricco et al., 2018). The chosen methodological framework was the model designed by Arksey and O'Malley and extended by Levac (Levac et al., 2010). This involved a six-step process: (i) identifying the research questions; (ii) identifying relevant studies; (iii) selecting studies; (iv) charting the data; (v) collating, summarizing and communicating the results and (vi) holding consultations.
3.1 Research questions
The research questions used in exploring the literature were as follows: (a) What are the roles of midwives in the prevention, diagnosis and management of PPH? (b) What challenges do midwives face regarding PPH?
3.2 Inclusion and exclusion criteria
The inclusion criteria for papers in this scoping review were as follows: (a) there were no restrictions on the type of study design, including qualitative studies, quantitative studies, mixed studies and reviews; (b) the research topics involved the roles of midwives and the challenges faced by them in managing PPH and (c) the delivery mode was vaginal delivery. The exclusion criteria were as follows: (a) the document was a set of guidelines, a meeting abstract, or a consensus; (b) the articles were repeated publications or had incomplete information or data; (c) the full text was unavailable or (d) the article was not published in English.
3.3 Information sources and search procedures
The databases searched were the Cochrane Library, PubMed, Web of Science, Ovid, Medline (Ovid, 1946 to present), Embase (Ovid, 1974 to present), JBIEBP (Ovid, current to present) and BIOSIS Previews (Ovid, 1994 to present). To identify the greatest possible number of articles, the search was conducted by combining Medical Subject Headings (MeSH terms), keywords and truncation. The final search strategy for PubMed can be found in Table 1.
| Search | Query | Records retrieved |
|---|---|---|
| #1 | (((((((((Postpartum Haemorrhage [MeSH Terms]) OR (postpartum haemorrhage [Title/Abstract])) OR (post partum haemorrhage [Title/Abstract])) OR (post partum haemorrhage [Title/Abstract])) OR (postpartum bleeding [Title/Abstract])) OR (maternal bleeding [Title/Abstract])) OR (obstetric haemorrhage [Title/Abstract])) OR (obstetric bleeding [Title/Abstract])) OR (PPH [Title/Abstract])) | 16,235 |
| #2 | ((((Nurse Midwives [MeSH Terms]) OR (Nurse Midwives [Title/Abstract])) OR (Accoucheur [Title/Abstract])) OR (midwi* [Title/Abstract])) | 32,557 |
| #3 | #1 AND #2 | 386 |
- Note: PubMed: Searched on 31 December 2022. No limitations.
3.4 Selection process
In this study, the bibliographies were imported into EndNote X9 for removal. The titles and abstracts of all bibliographies were read by two trained researchers (XY and LJD). Screening is based on inclusion/exclusion criteria. If there was any disagreement, two researchers (XY and LJD) held discussions to resolve the issue.
3.5 Charting the data
To guarantee a general description of the included articles, the following information was extracted from the resulting articles: author, year, country, participants, design, main findings and conclusions. Two researchers (XY and LJD) independently performed complete data extraction for the included studies. Discrepancies were resolved with a third researcher (RH) to ensure quality.
3.6 Analysis
The authors conducted a content analysis to identify subject areas from the extracted data. For the mapping process, all systematically selected studies were reviewed narratively and summarized, and the results were finally grouped together.
4 FINDINGS
4.1 Search and selection process
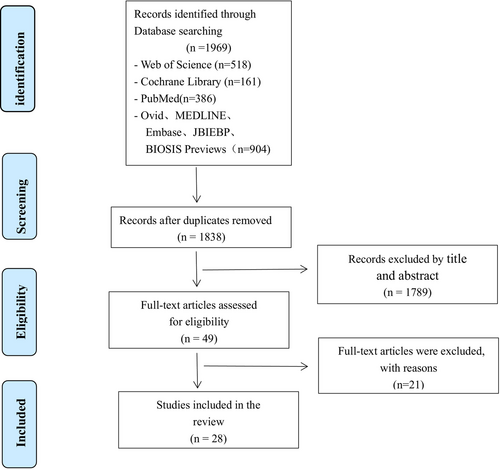
The initial database search yielded 1969 articles. We removed a total of 131 duplicates and screened 1789 reports according to the title and abstract. Subsequently, the full texts of the remaining 49 references were analysed to determine their eligibility. This led to the exclusion of 21 full texts that were deemed irrelevant to the study objectives for various reasons: 2 articles were in a non-English language, 10 articles were not available in full, and 9 articles did not match the topic. Ultimately, 1810 papers were excluded, and 28 papers were included. The search and selection processes are summarized in Figure 1.
4.2 Study characteristics
The research team conducted a summary analysis of the general characteristics of the included studies. Table 2 presents an overview of the study's characteristics. We found that the publication year of related studies spanned from 2012 to 2022, showing a gradual increasing trend, with the most publications in 2022. The included studies were conducted in 21 countries. Of these, 11 studies were from developed countries, and 17 studies were from developing countries. The country with the highest number of published articles was Australia. Regarding research methods, 21 articles were original studies, and seven articles were secondary analyses of original documents. Concerning the topic of the review, two publications involved the topic ‘third-stage management’, two articles evaluated ‘the effects of hands on and hands off/poised technique’, one article discussed ‘blood loss estimation’, one article focused on ‘Pronurturance Plus’ and one article discussed ‘experience in preventing PPH’. However, there were no reviews specifically on the roles of midwives and the challenges faced by them in managing PPH.
| Author, year, (country) | Funding | Design | Participants | Main findings | Conclusions |
|---|---|---|---|---|---|
| Zhang et al. (2021) (China) | No | Randomized controlled trial | Primiparous women (n = 340) | The postpartum haemorrhage amounts in the continuous midwifery group were lower than they were in the traditional midwifery group (p < 0.01). | Continuous delivery services for primiparas during natural delivery can significantly increase the natural delivery rate, reduce postpartum haemorrhage. |
| Loewenberg Weisband et al. (2018) (USA) | No | Cross-sectional study | Pregnant women (n = 8779) | The risks of caesarean and preterm birth were significantly lower among women who initiated prenatal care with a midwife compared with those who initiated prenatal care with a physician. | Our study provides further evidence that midwives provide a safe alternative to physician prenatal care. |
| Kalu and Chukwurah (2022) (Nigeria) | No | Qualitative study | Midwives (n = 15) | Four themes were identified: (1) interventions for preventing PPH; (2) approaches to managing PPH; (3) challenges of preventing and managing PPH; (4) ways of supporting midwives to overcome these challenges in rural health care settings. | Midwives in Nigerian rural health care settings engaged in preventive practices and active management of PPH, but there still were barriers, such as inadequate resources. |
| Petrocnik and Marshall (2015) (UK) | No | Systematic review | Five studies | The hands-poised technique appeared to cause less perineal trauma and reduced rates of episiotomy. The hands-on technique resulted in increased perineal pain after birth and higher rates of postpartum haemorrhage. | The hands-poised technique is a safe and recommended technique for perineal management and discussions of such a technique should be included in all midwifery education and training programs. |
| Huang et al. (2020) (China) | No | Systematic review | Nine RCTs | This study did not find a difference between hands-on and hands-off/poised techniques regarding the risk of postpartum haemorrhage. | Hands-off/poised is safe to use because it does not increase the risk of severe perineal trauma and postpartum haemorrhage. |
| Begley et al. (2019) (Ireland, UK) | No | Systematic review | Eight studies | Active management of the third stage of labour can reduce the risk of severe primary PPH greater than 1000 mL. | Active management of the third stage of labour can reduce mean maternal blood loss at birth and probably reduce the rate of primary blood loss. |
| de Castro Parreira and Gomes (2013) (Portuguese) | No | Integrative review | / | Most studies support the effectiveness of active management in reducing the risk of haemorrhage during the immediate postpartum period. | The results of this review of management practices supported active management of the third stage of labour can prevent postpartum haemorrhage. |
| Cohain (2022) (Israeli) | No | Cross-sectional study | Pregnant women (n = 2159) | Expedient delivery of the placenta in squatting within 3–5 min postpartum resulted in an average blood loss of 100 mL in the first 2 h after birth and no cases of PPH ≥500 mL in the first 24 h after birth. | The 1–3 min Expedient Squatting Protocol appears to be an effective third stage protocol that uses gravity, diaphragmatic and abdominal muscles and expedience to prevent postpartum haemorrhage. |
| Aydin Kartal et al. (2022) (Turkey) | Yes | Randomized controlled trial | Primiparous women (n = 68) | The 30th min oxytocin level was significantly higher in the control group (skin-to-skin contact interventions) than in the observation group (routine care). | Skin-to-skin contact intervention may have beneficial effects on postpartum pain and postpartum haemorrhage in the early postpartum period. |
| Saxton et al. (2016) (Australia) | No | Review | / | / | This article built upon previous theory and evidence of the effectiveness of simple pro-nurturance in reducing PPH rates to produces a new theory called Pro-nurturance Plus. |
| Liu et al. (2021) (China) | Yes | Cross-sectional study | Midwives and nurses (n = 361) | The accuracy and intra-rater agreement of visual estimation of blood loss (VEBL) were low with the help of visual aid. | The accuracy of VEBL was low even with a visual aid, especially when the volume exceeds 500 mL. To improve accuracy, institutions should make standard advised assessment guidance and provide regular training for blood loss quantification. |
| Wiklund et al. (2022) (Sweden) | No | Cross-sectional study | Pregnant women (n = 192) | The number of overestimates of blood loss was 45.3% (n = 87) with an average of 72.9 mL; the number of underestimates was 49.4% (n = 95) with an average of 73.8 mL. Exact correct estimations of blood loss were done in 5.2% of the cases (n = 10). | It is reasonable to start weighing blood loss when it exceeds 300 mL. |
| Natrella et al. (2018) (Italy) | No | Systematic review | Thirty-five studies | Accurate estimation of postpartum blood loss is identified as a major contributor to the improvement of maternal safety and the reduction of PPH-related morbidities. Visual estimation of postpartum blood loss is under debate. | The centrality of the role of nurses and midwives in quantifying blood loss, improving communication, initiating early diagnosis of obstetric haemorrhage and mobilizing a team response may worth the effort of discussing. |
| Golmakani et al. (2015) (Iran) | No | Cross-sectional study | Females (n = 112) | A significant difference was found between the estimated blood loss based on the weighting methods and using the National Guideline (p = 0.000). | Usage of symptoms and the weighing method is recommended in cases of postpartum bleeding. |
| Rosmaria et al. (2019) (Indonesia) | No | Qualitative study | Midwives (n = 23) | There were four methods of blood loss assessment (BLA) theoretically known to midwives, but there was only one applicable method. | The BLA was not undertaken in most labours. Physiological parameters were the most applicable method for the Indonesian midwives. |
| Smit et al. (2014) (Netherland) | No | Cross-sectional study | Cases of PPH (n = 98) | Eleven indicators were found to be applicable and feasible. Five of these indicators showed improvement potential. | Eleven out of 25 indicators were found to be suitable as an assessment tool for midwifery care of PPH |
| Moudi et al. (2019) (Iran) | No | Quasi-experimental design | Midwives (n = 47) | Midwives used more than one method to estimate blood loss and higher doses of oxytocin to control haemorrhage. They showed improvements in the use of intravenous fluid therapy, pulse and blood pressure checks, external uterine massage and uterotonic drugs. | Midwives' management of PPH improved after the interventions. Training programs should be based on study of the local situation to identify shortcomings. Regular monitoring of outcomes is needed to detect and resolve failures. |
| Esan et al. (2022) (Nigeria) | No | Qualitative study | Midwives (n = 15) | Two themes emerged from the analysis, including: (1) management practices adopted against PPH, (2) hospital protocol for the management of PPH. | The midwives are somewhat satisfied with PPH management in their facilities However barriers in PPH management still exist. |
| Wake and Wogie (2020) (Ethiopia) | No | Cross-sectional study | Midwives (n = 285) | The knowledge, practice level, and educational level of Midwives were significantly associated with active management of the third stage of labour. | Midwives should update their academic level and knowledge. Health institutions, in collaboration with the Tigray Regional Health Bureau, should arrange training for all midwives to bring about change. |
| Voillequin et al. (2022) (France) | Yes | Cross-sectional study | Midwives (n = 450) | The risk of delay was lower among midwives working in university maternity hospitals (OR 0.47, 95% 0.21, 0.97), in units with 1500–2500 births per year (OR 0.49, 95% CI 0.26, 0.90). and delay increased with the midwives' years of experience (OR 1.30, 95% CI 1.01, 1.69) years of experience. | Delays in oxytocin administration for first-line treatment of PPH suggest that continuing training of midwives should be considered, especially in small maternity units. |
| Ramavhoya et al. (2021) (Africa) | Yes | Qualitative study | Midwives (n = 18) | One theme emerged ‘challenges by midwives managing women with PPH’ with five subthemes, including: ‘difficulty experienced resulting in feelings of frustration and confusion and lack of time and shortage of human resource inhibits guidelines consultation’. | Midwives experienced difficulty managing women with postpartum haemorrhage. |
| Ramadhani et al. (2020) (China) | No | Cross-sectional study | Nurse-midwives (n = 160) | Knowledge was significantly contributed by multiple factors (p = 0.009). Correct AMTSL use was 46.8%, which was significantly affected by AMTSL training (X2 = 6.732, p = 0.009) and prioritizing attending an asphyxiated baby (X2 = 5.647, p = 0.017). | Regardless of high nurse-midwives' AMTSL knowledge. It is imperative that responsible authorities plan appropriate strategies to solve reported barriers affecting correct AMTSL use. |
| Prapawichar et al. (2020) (Thailand) | Yes | Case–control study | Women (N = 1833) | Inadequate nurse midwife to patient ratio, lacking nurse midwives with working experience of 6–10 years, inadequate equipment and supplies for emergency obstetric care had significantly higher incidences of having PPH, respectively. | Improving health care services by allocating sufficient human and physical resources would significantly reduce this complication. |
| Muthoni et al. (2021) (Kenya) | No | Cross-sectional study | Midwives (n = 156) | Midwives' factors that influenced the management of PPH were: professional qualification, labour ward experience, training on emergencies, midwife's knowledge and skills factors. | Indicate a statistical association between midwives' factors and the management of PPH. |
| Bewket et al. (2022) (Australia) | Yes | Qualitative study | Midwives, managers and obstetricians (N = 41) | Five themes were identified: (1) workforce, (2) communication issues between healthcare providers, (3) systemic issues, (4) education, training and resourcing issues, (5) lack of identification and referral. | Maternal healthcare providers in these hospitals require training in managing a birthing emergency. In addition, the birth units need adequate supplies and continuous essential services. |
| Beltman et al. (2013) (Malawi) | No | Qualitative study | Clinical officers, nurse-midwives medical assistants (N = 29) | Factors contributing to facility-based obstetric haemorrhage mentioned by participants were categorized into four major areas:(1) limited availability of basic supplies; (2) lack of human resources; (3) inadequate clinical skills of available health workers; (4) substandard referrals by traditional birth attendants and lack of timely self-referrals of patients. | Health workers in this district mentioned important community, system and provider related factors that need to be addressed in order to reduce the impact of obstetric haemorrhage. |
| Akter et al. (2022) (Australia) | Yes | Qualitative study | Midwives, nurses, doctors, managers (N = 45) | Four key themes were identified: (1) in-service training on emergency obstetric care; (2) limited knowledge about PPH; (3) current approaches to PPH detection, (4) current PPH management and associated challenges. | There are critical needs to address context-specific barriers to early and timely detection and management of PPH in hospital settings. |
| Finlayson et al. (2019) (Italy) | Yes | Systematic review | Thirty-five studies | Four key themes were identified: (1) What PPH means to stakeholders: belief, knowledge and understanding, (2) Organizational issues affect PPH prevention. (3) The value of competent caring, (4) Influence of uterotonics in PPH prevention. | PPH prevention strategies are more likely to be successful, especially in the context of sufficient resources and effective implementation by competent, suitably trained providers. |
4.3 Role of midwives in managing PPH
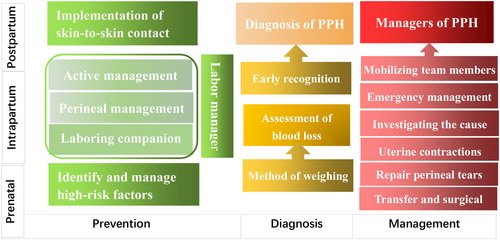
According to the reviewed studies, midwives have roles in the prevention, diagnosis and management of PPH, covering prenatal, intrapartum and postpartum care (Figure 2).
4.3.1 Prevention of PPH
In the prevention of PPH, midwives play roles such as identifying and managing high-risk factors, managing labour and implementing skin-to-skin contact (SSC).
Identification and management of high-risk factors
Five studies described the role of midwives in identifying and managing high-risk factors (Akter et al., 2022; Beltman et al., 2013; Kalu & Chukwurah, 2022; Loewenberg Weisband et al., 2018; Zhang et al., 2021). In the prenatal period, midwives can establish personalized health cards for pregnant women, conduct health education and provide psychological counselling for pregnant women and their families. This approach aims to improve the mother's physical fitness, reduce anxiety in pregnant women, recognize high-risk factors and decrease the occurrence of PPH (Zhang et al., 2021). The high-risk factors for PPH include a previous history of PPH, a large baby, multigravida, placental problems, anaemia, or a history of coagulopathy (Akter et al., 2022; Kalu & Chukwurah, 2022). The early identification of high-risk factors for PPH and optimizing pregnancy can effectively prevent its occurrence (Escobar et al., 2022). Midwives can guide pregnant women with anaemia to consume folic acid and iron supplements, provide prophylactic malaria treatment and conduct regular blood monitoring, aiming to maintain optimal haemoglobin levels during the antenatal period, thereby enhancing women's ability to cope with PPH if it occurs (Kalu & Chukwurah, 2022). When high-risk factors are severe or uncontrollable, timely referral to a higher level medical facility should be initiated (Beltman et al., 2013).
Management of labour
Midwives can manage labour according to established evidence-based practice. Labour is the process through which a foetus and placenta are delivered from the uterus through the vagina. There are three stages of labour in humans. The roles and functions of midwives during labour are described below.
Labour companion
Continuous one-to-one midwife support throughout the first stage of labour is an essential measure to reduce the risk of complications (Cederfeldt et al., 2016). Two studies have described the midwives' role as a labour companion (Kalu & Chukwurah, 2022; Zhang et al., 2021). The authors noted that during labour and delivery, having the same midwife continuously present at a women's bedside can slightly alleviate the pain through methods like massage, storytelling, reassurance and scientific guidance, thereby reducing the incidence of PPH.
Perineal management
In the second stage of labour, appropriate perineal management techniques are believed to reduce perineal trauma and subsequently reduce the occurrence of PPH. Two studies have explored the techniques of perineal management (Huang et al., 2020; Petrocnik & Marshall, 2015). Petrocnik conducted a systematic review comparing the hands-on and hands-poised techniques of perineal management during the second stage of labour. The review showed that the hands-on technique resulted in higher rates of PPH (Petrocnik & Marshall, 2015). Another study indicated that there was no difference between the hands-on and hands-off/poised techniques regarding the risk of PPH incidence (Huang et al., 2020).
Active management
Three studies described the roles of midwives in the third stage of labour (Begley et al., 2019; Cohain, 2022; de Castro Parreira & Gomes, 2013). Two studies focused on active management in the third stage of labour (AMTSL); the results from both studies showed that AMTSL reduced the risk of PPH (Begley et al., 2019; de Castro Parreira & Gomes, 2013). AMTSL comprises three components: (1) administration of uterotonic agents within 1 min of childbirth and delayed cord clamping; (2) active removal of the placenta by controlled cord traction following signs of placental separation; and (3) uterine massage immediately after removal of the placenta (WHO, 2014). Another study described a novel third-stage protocol. This protocol entails cutting the umbilical cord 1 min after delivery, encouraging the mother to squat 2 min after delivery and having the mother push out the placenta while in the squatting position, followed by a 10-s abdominal massage to promote uterine contractions once the mother is in bed, if consent was obtained before birth. The study found that the protocol resulted in an average blood loss of 100 mL in the first 2 h after birth and no cases of PPH ≥500 mL (Cohain, 2022).
Implementation of skin-to-skin contact
SSC is defined as immediate and uninterrupted contact between the woman and her newborn (Moore et al., 2016). Contact, heat and olfactory receptors with strong vagus nerve stimulants during SSC may lead to the release of maternal oxytocin. Oxytocin is one of the most important uterine contraction factors, capable of promoting rhythmic contractions of the uterine muscles, aiding in uterine contraction and detachment of the placenta and playing a crucial role in controlling PPH (Aydin Kartal et al., 2022). Two studies have demonstrated that SSC after delivery can reduce the incidence of PPH (Aydin Kartal et al., 2022; Saxton et al., 2016). Saxtonproposed a new theory based on SSC (Saxton et al., 2016). The theory, named ‘Pronurturance Plus’, posits that by establishing a trusting relationship between the midwife and pregnant woman, providing the pregnant woman with a warm environment, facilitating SSC and enhancing midwife supervision, the secretion of oxytocin is boosted.
4.3.2 Diagnosis of PPH
Midwives are often the first to diagnose PPH via early recognition and blood loss estimation. Midwives recognize PPH through clinical manifestations in women (decreased blood pressure, increased pulse rate, tachypnoea and altered physical and mental state) (Akter et al., 2022). Five studies focused on the assessment of postpartum blood loss (Golmakani et al., 2015; Liu et al., 2021; Natrella et al., 2018; Rosmaria et al., 2019; Wiklund et al., 2022). In Indonesia, midwives have not paid sufficient attention to the evaluation of postpartum blood loss, and physiological parameters are the most applicable method for doing so (Rosmaria et al., 2019). In China, a study that aimed to evaluate the accuracy of visually estimated blood loss in PPH by midwives and nurses showed that the overall accuracy was 30.52% (1763/5776), with 25.3% and 18.0% for PPH (500 mL) and severe PPH (1000 mL), respectively (Liu et al., 2021). The visual assessment was not credible, with both overestimates and underestimates of blood loss noted. Instead, the blood lost should be weighed, especially for bleeding greater than 300 mL (Golmakani et al., 2015; Natrella et al., 2018; Wiklund et al., 2022).
4.3.3 Management of PPH
Midwives' actions in first aid are crucial in determining maternal outcomes in PPH (Natrella et al., 2018). Midwives' roles mainly include mobilizing other professional team members (obstetricians, anaesthetists, laboratory staff and nurses) (Akter et al., 2022), emergency management (intravenous infusion therapy, oxygen inhalation, monitoring vital signs), investigating the cause, enhancing uterine contractions (extrinsic massage, administration of oxytocin and other drugs) and repair of perineal tears (Esan et al., 2022; Moudi et al., 2019; Smit et al., 2014). Transfer to the hospital and referral to a physician are essential when midwives are unable to control PPH, prepare for surgical intervention for those not responding to medical management, or provide support (Kalu & Chukwurah, 2022).
4.4 Challenges faced by midwives in PPH
The challenges faced by midwives with respect to PPH include insufficient knowledge and skills, poor teamwork skills, insufficient resources and dealing with their own negative emotions.
4.4.1 Insufficient knowledge and skills
Midwives' professional qualifications, clinical experience, knowledge level, age, working years and education level are closely related to the prevention and management of PPH (Muthoni et al., 2021; Ramadhani et al., 2020; Voillequin et al., 2022; Wake & Wogie, 2020). The knowledge factor includes knowledge on the prevention of PPH, correct use of prophylactic uterotonics, uterine massage during the third stage of labour, examination of the placenta and management of PPH (Muthoni et al., 2021). Due to knowledge deficiencies, midwives often feel confused and frustrated with PPH management (Ramavhoya et al., 2021).
4.4.2 Poor teamwork skills
The successful management of PPH requires a rapid and coordinated response by obstetricians, midwives and other staff members working under high-risk, time-critical and stressful conditions (Fleischer & Meirowitz, 2016). Miscommunication or a lack of communication among midwives, nurses, first responders and doctors has been identified as a key barrier to teamwork (Akter et al., 2022). This miscommunication leads to low efficiency among doctors with different roles in clinical practice. Miscommunication also results in multiple medical staff performing the same tasks, wasting rescue time and leading to delays, especially across different departments. Examples of these delays include blood reporting and waiting for an anaesthesiologist (Bewket et al., 2022).
4.4.3 Insufficient resources
Insufficient resources, such as infrastructure, labour ward equipment, laboratory facilities, medication and staff, act as inhibitory factors in the provision of timely and adequate care (Kalu & Chukwurah, 2022). Hospitals with an inadequate midwife patient ratio, a shortage of midwives with 6–10 years working experience and insufficient equipment and supplies for emergency obstetric care experience a significantly higher incidence of PPH (Prapawichar et al., 2020). In primary care settings, a single midwife is often responsible for all patients, which can result in the poor implementation of guidelines. Staff shortages are especially severe in certain low- and middle-income countries and are believed to contribute to maternal deaths (Beltman et al., 2013; Finlayson et al., 2019; Ramavhoya et al., 2021). Essential drugs, equipment and resources are frequently lacking or compromised across many countries. For instance, there is a shortage of uterine contraction-promoting drugs such as oxytocin, which requires cold chain preservation and transport. Emergency blood products, such as fresh frozen plasma and platelets, are often not readily available. Additionally, there is a lack of access to oxygen in emergency situations, which can exacerbate PPH, delay effective management and result in avoidable adverse outcomes (Beltman et al., 2013; Bewket et al., 2022; Esan et al., 2022; Kalu & Chukwurah, 2022).
4.4.4 Negative emotions experienced by midwives
Midwives who are able to maintain a positive attitude during PPH emergencies can enhance efficiency and provide care and comfort to birthing women by alleviating their anxiety and psychological distress, thereby promoting patient safety (Elfors et al., 2024; Kalu & Chukwurah, 2022). It has been reported that only 18.3% of midwives are able to provide positive emotional support (Muthoni et al., 2021). Some midwives encounter difficulties, experience a lack of confidence and grapple with negative emotions such as fear, depression, confusion and frustration when dealing with PPH, which can be attributed to factors such as midwives' insufficient knowledge, delayed ambulance services, the inadequate provision of a medical history by pregnant women and an unclear delineation of roles within the rescue team (Bewket et al., 2022; Ramavhoya et al., 2021).
5 DISCUSSION
In the present scoping review, we included 20 studies describing the roles of midwives in managing PPH. Most publications (12 of 20, 60%) reported the roles of midwives in preventing PPH. This result is consistent with the International Federation of Gynecology and Obstetrics (FIGO) guidelines, which state that all attempts should be made to reduce PPH with effective resources and appropriate interventions (Escobar et al., 2022). Fewer studies (5 of 20, 25%) reported midwives' role in diagnosing PPH. Consistent with a previous study, accurate estimation of postpartum blood loss was identified as a major contributor to the improvement of maternal safety and the reduction of PPH-related morbidities (Natrella et al., 2018). The best measure of PPH volume is the weighting method. Only a few studies (3 of 20, 15%) reported midwives' role in the management of PPH. This may be due to the inevitable overlap between the roles and responsibilities of different health care professionals (Wake & Wogie, 2020), resulting in few studies involving only midwives. Future research should focus on the roles of midwives in postpartum on-site management.
In this scoping review, studies on the roles of midwives in PPH covered a total of 16 countries, with five conducted in developing countries and 11 in developed countries. In developing countries, midwives' roles are focused on identification of high-risk factors, acting as a labour companion and assessment of postpartum blood loss; in developed countries, midwives are focused on active management of the third stage of labour and diagnosis and management of PPH. This difference is because, in some countries, the roles of midwives are limited by the health care system and cultural barriers. In Canada and the Netherlands, the midwife's scope of practice is limited to the care of women experiencing uncomplicated pregnancies. In the United Kingdom, New Zealand and Australia, midwives provide care to women who are experiencing medical and obstetric complications in collaboration with medical colleagues (Sandall et al., 2016). For countries in economic transition, like Iran and China, care is primarily led by obstetricians, with midwives mainly responsible for providing care during labour, collaborating with other healthcare professionals and being supervised by an obstetrician (Renfrew et al., 2014). Based on data from 37 countries around the world, most countries (31 of 37, 84%) report that midwives are authorized to perform AMTSL. Fewer studies (29 of 37, 78%) reported that midwives were authorized to administer magnesium sulphate to treat PPH, and still fewer (26 of 37, 70%) reported that midwives were authorized to perform manual removal of the placenta (Smith et al., 2014). In France, midwives provide the initial management of nearly all cases of PPH and can prescribe some drugs, including oxytocin (Voillequin et al., 2022). This shows that the broader the scope of practice for midwives, the more central their role in PPH.
As a single occupational group, midwives have great potential to contribute to the reduction of maternal and neonatal mortality as part of a multidisciplinary team operating within an enabling environment (Nove et al., 2021). The WHO has recommended a midwife-led continuity of care model in which a known midwife or a small group of known midwives supports a woman throughout the antenatal, intrapartum and postnatal continuum (Tuncalp et al., 2017). However, midwives face challenges in the management of PPH, which mainly include insufficient knowledge and skills, poor teamwork skills, insufficient resources and experiencing negative emotions.
Improvements can be made at the level of midwives, health care system managers and the government. Midwives must improve their knowledge, skills and teamwork abilities. Studies have shown that mentorship in the management of PPH increases the knowledge and self-efficacy of midwives in managing PPH (Musabwasoni et al., 2020). Therefore, a one-to-one tutorial system can be used to improve midwives' clinical skills. Simulation can be thought of as an educational modality and can encompass approaches such as mental rehearsal, verbal simulation, computer or screen-based simulation, task trainers, or team training experiences using equipment that ranges from low to high fidelity. Such simulations can improve team performance and reduce the incidence of PPH (Brazil et al., 2022; Gerard et al., 2024). For health care system managers, to increase AMTSL coverage in facilities with limited staff, task shifting for uterine massage and postpartum assessment to unskilled attendants or delivered women could be considered (Raams et al., 2018). Furthermore, improving the hospital supply chain of specialized first-aid consumables and drugs requires strengthening cooperation between the equipment department, pharmacy and obstetrics department. It is important to distinguish between general and first-aid modes, achieve differentiated management of consumables and drugs, set up a list of first-aid supplies and establish production and storage management mechanisms. Governments should provide adequate support to midwives and health care system managers to overcome challenges, including those related to inadequate resources such as human resources. For example, expanding the range of roles for midwives will enable them to provide needed services, thereby addressing the primary causes of maternal mortality (Smith et al., 2014). Finally, optimizing the ambulance management model ensures that ambulances can respond rapidly in emergency situations (Ramavhoya et al., 2021).
6 LIMITATIONS
This scoping review has some limitations. First, eight databases were searched in this study, and only full-text English published articles were included; unpublished guidelines, grey literature and non-full-text publications were not included. In terms of literature type, the included studies were mainly cross-sectional studies, qualitative interviews and secondary analyses; few randomized controlled studies were included.
7 CONCLUSION
Overall, the findings of this scoping review suggest that midwives play crucial roles in preventing, diagnosing and managing PPH during vaginal delivery, covering prenatal, intrapartum and postpartum care. In the prevention of PPH, midwives' roles involve identifying and managing high-risk factors, managing labour and implementing SSC. In the diagnosis of PPH, midwives have roles such as early recognition of PPH and blood loss estimation. In the management of PPH, midwives participate in mobilizing other professional team members, emergency management, investigating the cause, enhancing uterine contractions, repairing perineal tears, arranging transfers and preparing for surgical intervention. However, midwives face some challenges, including insufficient knowledge and skills, poor teamwork skills, insufficient resources and experiencing negative emotions. Midwives must improve their knowledge, skills and teamwork abilities. To this end, health care system managers and the government should give full support to midwives. Future research should focus on developing clinical practice guidelines for midwives for managing PPH and providing standardized guidance and best practices for midwives to ensure safer and more effective care for patients.
AUTHOR CONTRIBUTIONS
Xiao Yao contributed to the research design, data analysis and original draft. Shan-Shan Shan and Yue-Hong Li conducted a literature review and extracted data from studies. Yin-Yi Zhao and Rong Huang participated in supervision and review, project administration. All authors approved the final version for submission.
ACKNOWLEDGEMENTS
None declared.
FUNDING INFORMATION
2022–2023 Nursing Research Project of Chinese Medical Association Publishing House (CMAPH-NRG2022047). ‘Reservoir’ Talent Development Program of Shanghai First Maternity and Infant Hospital.“The Yuying”Talent Development Program of Shanghai First Maternity and Infant Hospital.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
All relevant data are within the paper.