The U-shaped association between hospitalization time and fall incidence in inpatients using publicly available data: A cross-sectional study in Japan
Abstract
Aim
To examine the association between the hospitalization time and fall incidence.
Design
A secondary analysis using the Dryad Digital Repository public database.
Methods
Data were extracted from the Fukushima Medical University Hospital cohort study between August 2008 and September 2009. The final analytic sample included 8,598 participants, 156 of who fell. The risk of fall incidents according to hospitalization time was estimated using logistic proportional hazards models, and restricted cubic splines with four knots model were developed.
Results
The median hospitalization time was 9.00 (4.00, 17.00) days. The incidence of falls was 1.81% (N = 156). A U-shaped association between the hospitalization time and fall incidence, with an inflextion point of 8 days. We found a decreasing fall incidence as the hospitalization time increased from 0 to 8 days (OR 0.72 [0.62 ~ 0.83], p < .001); beyond 8 days, the fall incidence increased as the hospitalization time increased (OR 1.06 [1.04 ~ 1.09]).
1 INTRODUCTION
A fall is defined as an unexpected event in which an individual comes to inadvertently rest on the ground, floor or lower level (Delbaere et al., 2021). Falls are common yet complex events and are caused by a variety of factors, such as disabilities and the nursing care environment (Hayakawa et al., 2014a, 2014b). They can lead to moderate to severe injuries, hospitalization, loss of independence and an increased risk of death (Lee et al., 2021; Lu et al., 2020). Patient falls and related injuries are considered nursing-sensitive indicators because fall prevention depends on the quantity and quality of nursing care (Dykes et al., 2020; Kutney-Lee et al., 2015). Most falls in hospitals are preventable (Choi et al., 2021; Hou et al., 2017). A previous study (Dykes et al., 2009) theorized that fall prevention in hospitals is a three-step process: (1) assessing the fall risk, (2) developing a personalized prevention plan and (3) executing the plan consistently. It is important to identify high-risk patients for falls, so preventive measures can be instituted in the hospital setting (Guerard et al., 2015).
However, existing fall risk prediction methods (for example, the Morse Fall Scale [MFS]) do not fully capture all the risk factors associated with inpatient falls (Cameron et al., 2018; Cho et al., 2019; Noh et al., 2021; Yang et al., 2021). Najafpour et al. (2019) found that longer length of stay increased the risk of patient falls, but Toye et al. (2019) and Chabot et al. (2019) found that the risk of falling was not associated with the length of stay, there have been few studies on the association between the hospitalization time and fall incidence, and the association between the hospitalization time and fall incidence remains unclear. Thus, this study aimed to elucidate whether the hospitalization time is associated with fall incidence.
2 BACKGROUND
The common risk factors for falls in inpatients were age, sex, history of falls, postural hypotension, mobility and cognitive status, and medications and so on (Hayakawa et al., 2014a, 2014b; Hou et al., 2017; Omer et al., 2018). In the past decades, fall risk assessment tools have been developed. Numerous risk factors for fall risk have been identified (Cho et al., 2019). The ideal modality for screening should have high sensitivity and high specificity, however, several fall risk assessment tools, such as St. Thomas' Risk Assessment Tool and the MFS, have reported inconclusive results (Hou et al., 2017).
Falls remain an important problem for the elderly in hospitals, particularly those with high fall risk (Toye et al., 2019), and thus, identifying predictive factors may help prevent inpatients from falls (Curcio et al., 2020). The top three departments ranked in the incidence of falls were oncology (35.6%), rehabilitation (20.3%) and neurology (18.6%) departments (Koç et al., 2020). Most falls occurred within a few weeks of admission (Lee & Stokic, 2008; Vlahov, et al., 1990; Wilson et al., 2020). Toye et al. (2019), who found that the risk of falling was not associated with the length of stay (OR 1.04; 95% CI 0.99–1.09; p = .076). The association between the hospitalization time and fall incidence remains unclear. Thus, this study aimed to elucidate whether the hospitalization time is associated with fall incidence.
3 MATERIAL AND METHODS
3.1 Study source
Data was extracted from the Dryad Digital Repository (https://datadryad.org/), which allowed users to freely download the raw data. We cited the Dryad data package ((Hayakawa et al., 2014a, 2014b), “Data from: Risk factors of falls in inpatients and their practical use in identifying high-risk persons at admission: Fukushima Medical University Hospital cohort study,” Dryad, Dataset, 10.1136/bmjopen-2014-005385) in the present study.
3.2 Study design and participants
This cross-sectional study was conducted between August 2008 and September 2009 among 8,598 inpatients (aged ≥ 18 years) included in the Fukushima Medical University Hospital (FMUH) database. This was a study at FMUH (Fukushima, Japan), designed to (1) identify the risk factors for falls in a hospital setting and (2) use such factors to identify the risk of falls in high-risk persons.
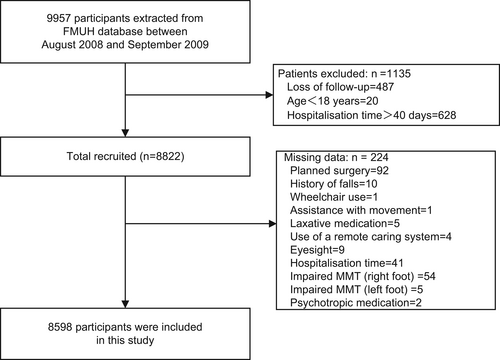
The details of the FMUH study were described previously (Hayakawa et al., 2014a, 2014b). Briefly, 9,957 participants who participated in the program between August 2008 and September 2009 were recruited at FMUH and were followed up until discharge. We excluded participants who were lost to follow-up (N = 487), with age <18 years (N = 20), and with a hospitalization time >40 days (N = 628). Participants with missing covariate information were excluded from the analyses (N = 224). A total of 8,598 participants were included in the final analysis (Figure 1). Our study was exempt from institutional review board oversight, because the Dryad database is accessible to the public, and the patients in the database are de-identified.
3.3 Variables
The primary outcome measured was a fall event, which was treated as a classified variable (no or yes). The primary exposure of interest was the hospitalization time, which was a continuous variable.
The covariates included in the analysis were age, sex, history of falls, cognitive dysfunction, planned surgery, wheelchair use, assistance in movement, eye sight, use of a remote caring system, impaired manual muscle test (MMT, defined as MMT <4) (Bohannon, 2005), assistance with activities of daily living (ADL), medication use (for example, laxative, sedative, hypnotic, and psychotropic medications).
Information was collected using a structured questionnaire through face-to-face interviews and clinical records at admission, conducted by nurses and doctors. A low level of ADL was defined as the need for help with any one of the seven activities (standing, sitting, dressing, eating, toileting, evacuation and washing of face).
3.4 Statistical analysis
The continuous variable, hospitalization time, was defined as a categorical variable. All the normally distributed and skewed continuous variables were described as mean (standard deviation) or median (interquartile range), and categorical variables were described as frequencies (%). The baseline characteristics of the different hospitalization time groups were analysed using one-way analysis of variance (normal distribution), the Kruskal–Wallis H (skewed distribution), and chi-square test (categorical variables).
Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for falls associated with the hospitalization time using four logistics proportional hazards models as follows: (1) unadjusted; (2) adjusted for age and sex; (3) adjusted for history of falls, MMT (left foot), MMT (right foot), cognitive dysfunction, eyesight, assistance with ADLs based on Adjust I; and (4) adjusted for planned surgery, wheelchair use, assistance with movement, laxative use, use of a remote caring system, sedative use, hypnotic medication use and psychotropic medication use based on Adjust II.
We determined whether each potential confounding variable was associated with falls. A confounder was defined as a variable with a clinically meaningful relationship with a risk factor and outcome (regardless of statistical significance). Besides, we also used restricted cubic splines with four knots at the 5th, 35th, 65th and 95th centiles to flexibly model the association between hospitalization time and fall incidence. Subgroup analyses were conducted by age, sex, history of falls, cognitive dysfunction, and laxative, hypnotic and psychotropic medications use using stratified logistic regression models. All analyses were performed using the statistical software packages R 3.3.2 (http://www.R-project.org; The R Foundation) and Free Statistics software version 1.2. p-Values <.05 (two-sided) were considered statistically significant.
4 RESULTS
4.1 Baseline characteristics of study participants by categories of hospitalization time
Figure 1 shows the number of eligible participants and participants analysed in this study. Participants who were lost to follow-up, with age <18 years, with a hospitalization time >40 days, and those who lacked clear records on covariants were excluded. Therefore, 8,598 participants were included in the final analysis. Inpatients who met the study criteria were identified in the FMUH database from August 2008 to September 2009.
Table 1 Of the 9,957 participants, 1,359 were excluded, and thus the data from 8,598 inpatients (mean age 59.30 ± 17.39 years; 4,294 male, 4,304 female) were analysed in the current study. The Incidence rate of falls was 1.81% (N = 156) in the present study, then the participants were divided into tertiles based on the hospitalization time. The participants with the longest hospitalization time were likely to fall, compared with those who had the shortest hospitalization time (p < .001). The mean age, sex, number of falls, history of falls, wheelchair use, assistance with movement, MMT right or left, laxative medication use, hypnotic and psychotropic medication use, cognitive dysfunction, eyesight and assistance with ADLs, among others, varied significantly between groups. Meanwhile, the proportion of participants who fell was higher in the participants using hypnotic and psychotropic medications.
| Variables | All participants | Hospitalization time tertile | p-Value | ||
|---|---|---|---|---|---|
| Q1 (≤5 days) | Q2 (6–12 days) | Q3 (≥13 days) | |||
| Participants (N) | 8,598 | 2,824 | 2,634 | 3,140 | |
| Age (years) | 59.30 ± 17.39 | 59.07 ± 17.86 | 56.65 ± 18.11 | 61.75 ± 15.96 | <0.001 |
| Sex (%) | |||||
| Male | 4,294 (49.94) | 1,380 (48.87) | 1,244 (47.23) | 1,670 (53.18) | <0.001 |
| Female | 4,304 (50.06) | 1,444 (51.13) | 1,390 (52.77) | 1,470 (46.82) | |
| History of falls (%) | |||||
| No | 7,866 (91.49) | 2,606 (92.28) | 2,436 (92.48) | 2,824 (89.94) | <0.001 |
| Yes | 732 (8.51) | 218 (7.72) | 198 (7.52) | 316 (10.06) | |
| Cognitive dysfunction (%) | |||||
| No | 8,403 (97.73) | 2,760 (97.73) | 2,591 (98.37) | 3,052 (97.20) | 0.012 |
| Yes | 195 (2.27) | 64 (2.27) | 43 (1.63) | 88 (2.80) | |
| Planned surgery (%) | |||||
| No | 4,971 (57.82) | 1,829 (64.77) | 1,515 (57.52) | 1,627 (51.82) | <0.001 |
| Yes | 3,627 (42.18) | 995 (35.23) | 1,119 (42.48) | 1,513 (48.18) | |
| Wheelchair use (%) | |||||
| No | 6,962 (80.97) | 2,383 (84.38) | 2,219 (84.24) | 2,360 (75.16) | <0.001 |
| Yes | 1,636 (19.03) | 441 (15.62) | 415 (15.76) | 780 (24.84) | |
| Assistance with movement (%) | |||||
| No | 7,436 (86.49) | 2,475 (87.64) | 2,347 (89.10) | 2,614 (83.25) | <0.001 |
| Yes | 1,162 (13.51) | 349 (12.36) | 287 (10.90) | 526 (16.75) | |
| Eye sight (%) | |||||
| Normal | 4,480 (52.11) | 1,494 (52.90) | 1,419 (53.87) | 1,567 (49.90) | <0.001 |
| Use spectacles | 3,349 (38.95) | 1,025 (36.30) | 979 (37.17) | 1,345 (42.83) | |
| Need help 1 | 468 (5.44) | 191 (6.76) | 148 (5.62) | 129 (4.11) | |
| Need help 2 | 274 (3.19) | 104 (3.68) | 77 (2.92) | 93 (2.96) | |
| Trance | 23 (0.27) | 9 (0.32) | 9 (0.34) | 5 (0.16) | |
| Zero | 4 (0.05) | 1 (0.04) | 2 (0.08) | 1 (0.03) | |
| Use of a remote caring system (%) | |||||
| No | 8,532 (99.23) | 2,804 (99.29) | 2,622 (99.54) | 3,106 (98.92) | 0.055 |
| Yes | 2 (0.02) | 0 (0.00) | 0 (0.00) | 2 (0.06) | |
| Crip censor | 29 (0.34) | 10 (0.35) | 3 (0.11) | 16 (0.51) | |
| Other censor | 35 (0.41) | 10 (0.35) | 9 (0.34) | 16 (0.51) | |
| Impaired MMT (right foot) (%) | |||||
| Zero | 75 (0.87) | 34 (1.20) | 16 (0.61) | 25 (0.80) | <0.001 |
| Trance | 52 (0.60) | 16 (0.57) | 11 (0.42) | 25 (0.80) | |
| Poor | 65 (0.76) | 20 (0.71) | 10 (0.38) | 35 (1.11) | |
| Fair | 88 (1.02) | 27 (0.96) | 22 (0.84) | 39 (1.24) | |
| Good | 400 (4.65) | 123 (4.36) | 96 (3.64) | 181 (5.76) | |
| Normal | 7,918 (92.09) | 2,604 (92.21) | 2,479 (94.12) | 2,835 (90.29) | |
| Impaired MMT (left foot) (%) | |||||
| Zero | 75 (0.87) | 39 (1.38) | 15 (0.57) | 21 (0.67) | <0.001 |
| Trance | 63 (0.73) | 21 (0.74) | 18 (0.68) | 24 (0.76) | |
| Poor | 78 (0.91) | 27 (0.96) | 14 (0.53) | 37 (1.18) | |
| Fair | 104 (1.21) | 28 (0.99) | 26 (0.99) | 50 (1.59) | |
| Good | 380 (4.42) | 100 (3.54) | 100 (3.8) | 180 (5.73) | |
| Normal | 7,898 (91.86) | 2,609 (92.39) | 2,461 (93.43) | 2,828 (90.06) | |
| Assistance with ADLs (%) | |||||
| No | 6,713 (78.08) | 2,246 (79.53) | 2,188 (83.07) | 2,279 (72.58) | <0.001 |
| Yes | 1,885 (21.92) | 578 (20.47) | 446 (16.93) | 861 (27.42) | |
| Laxative medication (%) | |||||
| No | 7,091 (82.47) | 2,330 (82.51) | 2,254 (85.57) | 2,507 (79.84) | <0.001 |
| Yes | 1,507 (17.53) | 494 (17.49) | 380 (14.43) | 633 (20.16) | |
| Sedative medication (%) | |||||
| No | 8,458 (98.37) | 2,776 (98.3) | 2,598 (98.63) | 3,084 (98.22) | 0.43 |
| Yes | 140 (1.63) | 48 (1.7) | 36 (1.37) | 56 (1.78) | |
| Hypnotic medication (%) | |||||
| No | 7,285 (84.73) | 2,440 (86.4) | 2,246 (85.27) | 2,599 (82.77) | <0.001 |
| Yes | 1,313 (15.27) | 384 (13.6) | 388 (14.73) | 541 (17.23) | |
| Psychotropic medication (%) | |||||
| No | 8,068 (93.84) | 2,649 (93.8) | 2,495 (94.72) | 2,924 (93.12) | 0.042 |
| Yes | 530 (6.16) | 175 (6.2) | 139 (5.28) | 216 (6.88) | |
| Hospitalization time (days) | 9.00 (4.00, 17.00) | 3.00 (2.00, 4.00) | 8.00 (7.00, 10.00) | 20.00 (16.00, 26.00) | <0.001 |
| Falls (%) | |||||
| No | 8,442 (98.19) | 2,781 (98.48) | 2,613 (99.20) | 3,048 (97.07) | <0.001 |
| Yes | 156 (1.81) | 43 (1.52) | 21 (0.80) | 92 (2.93) | |
- Note: Data presented are mean ± standard deviation, median (Q1%–Q3%), or N (%).
- Abbreviations: ADL, activities of daily living; FMUH, Fukushima Medical University Hospital, Fukushima, Japan; MMT, manual muscle test.
4.2 Association of the hospitalization time with fall incidence
Table 2 shows the association between the hospitalization time and falls using the multiple logistic regression models. In the non-adjusted model, there was an initial decrease followed by an increasing risk for developing falls as the tertile of hospitalization time increased; participants who had a hospitalization time in the highest tertile versus the lowest tertile had an approximately twofold increased risk of falls (OR, 1.95; 95% CI, 1.35, 2.81), p for trend <.0001. Similar results were obtained in the model adjusted for all covariates, including age, sex, history of falls, MMT left, MMT right, cognitive dysfunction, eyesight, assistance with ADL, planned surgery, wheelchair use, assistance with movement, laxative medication use, remote caring system, and sedative, hypnotic and psychotropic medications use (OR 1.57, 95% CI 1.07 to 2.30, p = .021), p for trend = .006.
| Item | Non-adjusted | Adjust I | Adjust II | Adjust III | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Hospitalization time (day) | 1.05 (1.03, 1.06) | <.001 | 1.04 (1.03 ~ 1.06) | <.001 | 1.04 (1.02 ~ 1.05) | <.001 | 1.03 (1.02 ~ 1.05) | <.001 |
| Hospitalization time tertile | ||||||||
| Q1 (≤5 days) | 1 | 1 | 1 | 1 | ||||
| Q2 (6–12 days) | 0.52 (0.31 ~ 0.88) | .014 | 0.56 (0.33 ~ 0.95) | .031 | 0.55 (0.32 ~ 0.93) | .027 | 0.54 (0.32 ~ 0.93) | .025 |
| Q3 (≥13 days) | 1.95 (1.35 ~ 2.81) | <.001 | 1.87 (1.30 ~ 2.70) | .001 | 1.64 (1.13 ~ 2.38) | .010 | 1.57 (1.07 ~ 2.30) | .021 |
| p For trend | 1.53 (1.25 ~ 1.87) | <.001 | 1.48 (1.21 ~ 1.80) | <.001 | 1.37 (1.12 ~ 1.68) | .002 | 1.34 (1.09 ~ 1.64) | .006 |
- Note: Data presented are odds ratios (ORs) and 95% confidence intervals (CIs). Adjust I model adjusts for age and sex. Adjust II model adjusts for adjust I + history of falls + MMT (left foot) + MMT (right foot) + cognitive dysfunction + eyesight + assistance with ADLs.Adjust III model adjusts for adjust II + planned surgery + wheelchair use + assistance with movement + laxative medication use + use of a remote caring system + sedative medication use + hypnotic medication use + psychotropic medication use.
- Abbreviations: ADL, activities of daily living; FMUH, Fukushima Medical University Hospital, Fukushima, Japan; MMT, manual muscle test.
4.3 Inflection point analysis of the hospitalization time on fall incidence
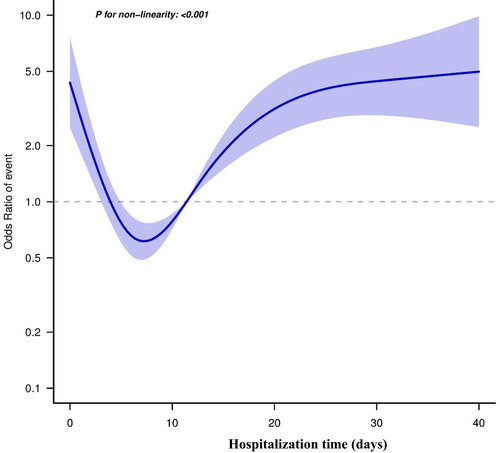
The relationship between falls and the hospitalization time was non-linear (p value, non-linear <.001), and a model using restricted cubic splines with three knots revealed a U-shaped association, with a decreasing fall incidence as the hospitalization time increased from 0 to 8 days (OR 0.72 [0.62 ~ 0.83], p < .001); beyond 8 days, the fall incidence increased as the hospitalization time increased (OR 1.06 [1.04 ~ 1.09]) (Figure 2, Table 3). In the figure, the blue solid line indicates the estimated risk of fall incidence, and the light blue shadow represents point-wise 95% CI adjusted for age, sex, history of falls, MMT (left foot), MMT (right foot), cognitive dysfunction, eyesight, assistance with ADLs, planned surgery, wheelchair use, assistance with movement, laxative medication use, remote care system use, and sedative, hypnotic and psychotropic medications use.
| Outcome: | OR (95% CI) | p Value |
|---|---|---|
| Two-piecewise linear regression model | ||
| Hospitalization time <8 days | 0.72 (0.62 ~ 0.83) | <.001 |
| Hospitalization time ≥8 days | 1.06 (1.04 ~ 1.09) | <.001 |
| Likelihood ratio test | — | <.001 |
- Note: Adjusted for age, sex, history of falls, MMT (left foot), MMT (right foot), cognitive dysfunction, eyesight, ADL, planned surgery, wheelchair use, assistance with movement, laxative medication use, use of a remote care system, and sedative, hypnotic, and psychotropic medications use.
- Abbreviations: ADL, activities of daily living; CI, confidence interval; FMUH, Fukushima Medical University Hospital, Fukushima, Japan; MMT, manual muscle test; OR, odds ratio.
4.4 Subgroup analysis
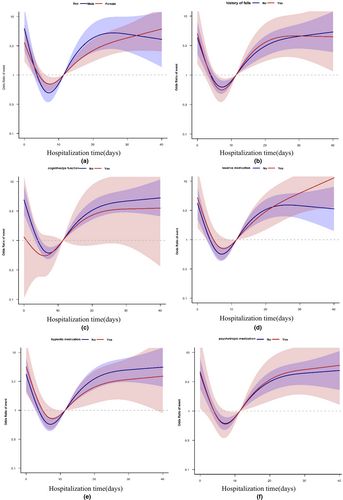
Sex, history of falls, cognitive dysfunction, and laxative, hypnotic and psychotropic medications use are known confounders of hospitalization time–fall association (Hayakawa et al., 2014a, 2014b). In order to investigate whether different layers affected the hospitalization time and falls, stratification analysis in subgroups was performed (Figure 3). We found a stable correlation between the hospitalization time and falls.
5 DISCUSSION
The present study investigated the association between the hospitalization time and the incidence of falls. The hospitalization time was independently associated with fall incidence with U-shaped association curves among inpatients. The findings show that the fall incidence first decreased and then increased as hospitalization time increased. The association between the hospitalization time and fall incidence was stable between layers.
Falls remain an important problem for the elderly in hospitals, particularly those with high fall risk (Toye et al., 2019), and thus, identifying predictive factors may help prevent inpatients from falls (Curcio et al., 2020). A systematic review reported that fall rates ranged from 1.52% to 3.41% in inpatients (Sattar et al., 2021) and 30.23% in oncology inpatients (Li et al., 2018). Meanwhile, a lower incidence (1.8%) was observed in this study, which is in line with previous studies (Li et al., 2018; Sattar et al., 2021).
Most falls occurred within a few weeks of admission (Lee & Stokic, 2008; Wilson et al., 2020). Compared with 6–12 days, the risk of falling in 0–5 days and more than 13 days was significantly increased in our study. This finding was consistent with that of Najafpour et al. (2019), which found that the risk of falling was associated with a longer length of stay (odds ratio [OR] = 1.01; CI = 1.01 to 1.02, p < .001). However, there are also some other studies that are inconsistent with our findings. Toye et al. (2019) and Chabot et al. (2019) reported that the risk of falling was not associated with the length of stay. We analysed these studies that are inconsistent with our results, and we speculate that the reasons for the different results may be caused by the following factors: (1) fall risk assesment is different. Falls event was collected from clinical records in our study, but the risk of falls was measured using the MFS in the study of Chabot et al. (2019); (2) the research population is different. The study of Toye et al. (2019) was targeted at acute hospital inpatients. The association between the hospitalization time and falls was U-shaped, and the inflection point was eight days in our study, we found that beyond 8 days, falls increased as hospitalization time increased; but the median hospitalization time was 5 (1–48) days, and in the study by Toye et al. (2019), different hospitalization times led to different results. The top three department ranked in the incidence of falls were oncology (35.6%), rehabilitation (20.3%), and neurology (18.6%) departments (Koç et al., 2020; Lovallo et al., 2010). This may be attributed to the following: ① the high fall rate in the inpatient setting may be related to the increased frailty in patients with advanced disease settings (Sattar et al., 2021). Many cancer- and treatment-related factors and toxicities (Guerard et al., 2015) can increase the risk of falls (Kolb et al., 2016; Li et al., 2018). ② Nutritional status is associated with function, physical performance, and falls in older adults admitted to geriatric rehabilitation (Urquiza et al., 2020). ③ Inpatients may sometimes limit their participation in activities due to fear of falls, which may cause a real decline in physical capacity and increase the fall incidence (Denkinger et al., 2015; Filiatrault et al., 2013).
5.1 Strengths and limitations
The strengths of our study include the fact that our sample size was relatively large compared to that of previous similar studies performed on inpatients (≥18 years). Nevertheless, there are some limitations to our study. First, our research participants were restricted to inpatients (≥18 years); therefore, there was a certain deficiency in the universality and extrapolation of the research. Second, there was a selection bias in the present study. The hospitalization time of our participants was ≤40 days, which might have led to an underestimation of the incidence of falls. Third, the data lacks disease type, patients' clinical conditions and worsening or improvement during the hospital stay, treatments received, and characteristics of the care team, but it is important to evaluate preventive factors against falls. In the future, we need a large sample of forward-looking fall data to improve the research in this area.
6 CONCLUSIONS
In this study, the hospitalization time was found to be significantly associated with fall incidence. The association was U-shaped, with an inflection point at eight days of hospitalization.
Further studies are needed to determine whether a causal association exists between the hospitalization time and falls. Our findings highlight that the hospitalization time should be included in the fall risk assessment or prediction model, such that inpatients may benefit from fall prevention interventions.
7 RELEVANCE TO CLINICAL PRACTICE
It is important to identify high-risk patients for falls. Understanding the risk factors associated with inpatient falls is the first step in preventing falls. However, existing fall risk prediction methods (for example, the Morse Fall Scale) do not fully capture all the risk factors associated with inpatient falls. In this study, the hospitalization time was found to be significantly associated with fall incidence. Therefore, the hospitalization time should also be considered when falls risk factors are assessed in hospital settings. Our findings highlight that the hospitalization time should be included in the fall risk assessment or prediction model, such that inpatients may benefit from fall prevention interventions.
AUTHOR CONTRIBUTIONS
All the authors designed the study. Data analyses and interpretation were performed by Yonghong Chen and Zihong Chen. Qiang Zhong and Zihong Chen drafted and revised the manuscript. Critical revision of the article: Lihua Chen, Huanhuan Peng. All the authors read and approved the final manuscript.
- substantial contributions to conception and design, acquisition of data or analysis and interpretation of data;
- drafting the article or revising it critically for important intellectual content.
ACKNOWLEDGEMENTS
We thank Dr. Liu Jie (People's Liberation Army of China General Hospital, Beijing, China) and Dr. Yang Qilin (The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China) for helping in this revision.
FUNDING INFORMATION
This study was supported by the Guangxi Health and Family Planning Commission (Z2019380), Wuzhou Science and Technology Plan Project of Guang Xi (201902169).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Extra data can be accessed via the Dryad data repository at http://datadryad.org/ with the doi: 10.5061/dryad.16h8j