An evidence-based general anaesthesia and prone position nursing checklist: Development and testing
Abstract
Aim
Prone positioning during general anaesthesia is one of the most difficult practices for the perioperative nurse. Patients in this position are vulnerable to many preventable complications. However, no studies have developed an evidence-based tool to improve nursing practice during general anaesthesia and prone positioning. This study aimed to develop and test a general anaesthesia and prone position nursing checklist for use by the circulating nurse.
Design
A prospective pre-post study was performed between October 2020 and March 2021.
Methods
The WHO checklist development model and evidence-based methods guided the checklist development process. We prospectively observed circulating nurses that attended to prone general anaesthesia during posterior lumbar spine surgery for 3 months before and after the introduction of the general anaesthesia and prone position nursing risk checklist. The main outcomes were successful delivery of essential prone positional nursing practices during each surgery and the nurse's opinion of the checklist's efficacy and utility.
Results
A general anaesthesia and prone position nursing checklist comprised of 4 pause points and 22 necessary nursing practices was developed. Seventy-two nurses participated in this study. Use of the checklist significantly increased the average performance of essential practices during each surgery from 72.72%–95.45%. Three measures had a compliance rate of 100%. The delivery rate of 14 measures was significantly improved, 91.7% of nurses considered the checklist easy to use, and 94.4% nurses would want the checklist to be used if they underwent a prone position and general anaesthesia operation.
1 INTRODUCTION
General anaesthesia with patients in the prone position is one of the most common used and difficult surgical positions and is required during many types of surgeries, including spine, neurosurgery and urinary (Spruce, 2021). The patient under general anaesthesia in the prone position is vulnerable to multiple injuries, including pressure injuries (PI), postoperative vision loss (POVL), perioperative peripheral nerve injuries (PPNI), tongue swelling resulting in airway compromise and even permanent disability (Association of periOperative Registered Nurses, 2020). Existing literature reports that intraoperatively induced PI occur in 5% to 66% of this position (Association of periOperative Registered Nurses, 2020). POVL after spine surgery in the prone position is a rare but devastating complication with an incidence of about 0.017% to 1%(Xiong et al., 2020). Most of these types of injuries are well-understood and largely avoidable by following clinical practice guidelines (CPG). However, prior work showed that 73% of the operating room (OR) nurses did not have adequate knowledge about how to prevent perioperative PI, and their ability to identify risks for PI was also limited (Khong et al., 2020). Besides, they also lack evidence-based tools and methods to help them provide optimal prone position nursing practices (Woodfin et al., 2018).
Checklists had been used for many decades in aviation, construction and other non-medical areas to guide users when completing tasks during which errors or omissions can be fatal (Oliveira et al., 2017). The WHO defined medical checklists as useful tools for bridging the gap between evidence and safe daily practices (World Health Organization, 2009). Two studies designed checklists for anaesthesia practitioners and intensive care unit (ICU) practitioners to provide proper prone positioning techniques (Oliveira et al., 2017; Salkind, 2013). These two checklists can effectively improve prone positioning care safety and set up a standard prone positioning procedure. However, both checklists were based on unevaluated evidence, and their target users were not circulating nurses.
The circulating nurse in particular plays a critical role in surgical patient positioning. The circulating nurse must balance surgical comfort with optimal exposure of the surgical site, airway management, ventilation and monitoring access for the anaesthesia care provider while minimizing the risk of injury to the patient (Kwee et al., 2015; Spector et al., 2013). It is critical for the circulating nurse to deliver standardized and scientific interventions when the patient is in the prone position. This study aimed to design and implement an evidence-based general anaesthesia and prone position nursing checklist (GAPPNC) to improve the circulating nurse's delivery of standard prone positional nursing practices and investigated the nurse's evaluation of the checklist. The checklist development process was based on the WHO checklist development model and evidence-based methods.
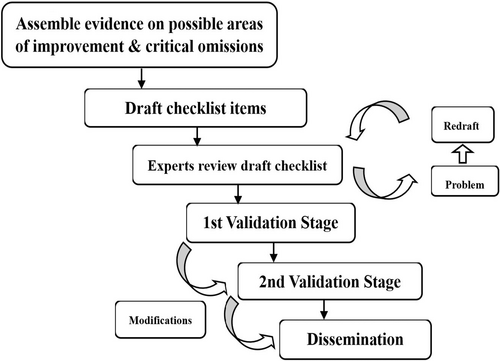
1.1 Theoretical framework
The study followed the WHO-recommended checklist development model (Figure 1) and the WHO Safe Childbirth Checklist development study (Spector et al., 2013). A checklist is a set list used to identify, schedule or verify a group of elements or key points, and used as a visual or oral aid to supplement the user's memory. A medical checklist improves the provision of care and guides the medical staff towards consistently following a core set of safety practices to minimize the most common and avoidable medical errors that can endanger the patient's life and well-being (World Health Organization, 2009). WHO-designed checklists and its checklist development model have received global recognition (Haynes et al., 2009). Weiser and Spector described the WHO methodology as the basis for content and critical implementation components of a checklist development program in order to help inform health workers in the design of different medical checklists (Weiser et al., 2010).
2 MATERIALS AND METHODS
2.1 Study design
We conducted a single-centre prospective pre-post intervention study in Sir Run Run Shaw Hospital of Zhejiang University School of Medicine. The hospital is a large, tertiary, research-oriented general university hospital in Hangzhou, Zhejiang province, China. The study consisted of two phases: (1) development of a GAPPNC, (2) testing the feasibility of using the GAPPNC.
2.2 GAPPNC development
2.2.1 Establishment of a multidisciplinary development team
A multidisciplinary development team was established, including the OR nursing manager, director of orthopaedics, director of anaesthesiology and hospital administrative coordinator from the Sir Run Run Shaw Hospital of Zhejiang University School of Medicine. The responsibilities of the team members include reviewing the guidelines for general anaesthesia in the prone position, drafting the first edition of the checklist, assembling expert consultation, iterative refinement through consultation, evaluating checklist feasibility.
2.2.2 Literature review and quality evaluation
A comprehensive literature review of the major causes of general anaesthesia-prone position complications and existing CPGs that targeted these major complications were combined to a background document. This document was critical for not only establishing goals for improvement but also for highlighting the specific practices necessary to achieve these goals. The background document also suggested additional topics for consideration as part of the checklist (Spector et al., 2013; Weiser et al., 2010). The document was circulated to all confirmed participants in the Delphi consultation. The following electronic databases were systematically searched for CPGs: Chinese Biomedical Literature Database, the VIP Database, Wanfang Database, Google Scholar, Joanna Briggs Institutions, PubMed, National Guideline Clearinghouse, and WHO. Search terms included general anaesthesia, positioning, surgical position, patient positioning, prone, prone position, positioning injury, pressure injury, POVL, perioperative neuropathy injury, circulating nurse, operative nurse, perioperative nurse, perioperative nursing, CPG, practice guidelines, and advisory. The inclusion criteria were that the guidelines needed to be published in either the English or Chinese language before June 2020 and deal with general anaesthesia and prone positioning interventions in the OR. Articles with an AGREE II overall score less than 70% were excluded so that guidelines with the highest possible quality could be chosen. The AGREE II instrument was developed to assess the quality of guidelines. It is an effective and reliable tool that consists of 23 items organized into six domains, including scope and purpose, stakeholder involvement, rigour of development, clarity of presentation, applicability and editorial independence (Spector et al., 2013). Two researchers independently used the AGREE II instrument to appraise the identified guidelines.
2.2.3 Identify critical omissions and draw up the checklist
According to Weiser's study, the overall goal during the development of a medical checklist was to focus only on “killer items” that are most critical, known to be often overlooked, and put the patient at the highest risk of harm when ignored (Weiser et al., 2010). Critical omissions during general anaesthesia-prone position surgery identified by the team included electric burns, PI, POVL, PPNI, spinal injury and accidental falls. The scope of application of the checklist was found to be applicable to ORs in China, and the target users were determined to be the circulating nurses in the OR. The sequence of checking entries in the checklist must follow the actual workflow of the circulating nurse and be within his or her area of responsibility. Based on these key demands, the core team extracted and summarized evidence from 6 guidelines to develop the first edition of the GAPPNC, which consisted of 21 items.
2.2.4 Delphi expert consultation
Delphi expert consultation was used to collect expert judgements and compare the aggregate judgements of all experts until a consensus criterion is reached. There is no consensus on expert consultation sample size. The usually recommended sample size of experts is 15–30 (Shi et al., 2020). The criteria for selecting experts included: (a) an intermediate technical title or higher, (b) a bachelor's degree or higher, (c) more than 20 years of experience in the profession, and (d) were familiar with the Delphi method and volunteered for this survey. All experts worked anonymously and independently.
An expert consultation questionnaire was developed by the core team and sent to the experts via e-mail. The draft checklist's constructs and subconstructs were presented to the experts during the first Delphi round, and the experts were asked to comment on the checklist and its constructs and subconstructs. They were also asked to comment on the rationality, comprehensiveness, suitability and applicability of the proposed checklist in OR, and whether there were items that needed to be modified, deleted or added. Expert responses were reviewed and integrated into the second draft of the checklist, which was presented to the Delphi panellists during the second round together with the revised expert consultation questionnaire. The experts were asked to re-evaluate each item during the second round. The second Delphi round resulted in consensus on the checklist content.
2.2.5 Field test
To pre-test the applicability and feasibility of the checklist, the checklist was used by 5 circulating nurses in a total of 20 prone position and general anaesthesia posterior lumbar spine surgeries over the course of 2 weeks. Nurse evaluation and feedback were collected, and the team modified the checklist according to that feedback.
2.3 Application of the GAPPNC for 6 months
A 6-month prospective pre-post study was performed to assess the feasibility of the GAPPNC at Sir Run Run Shaw Hospital, affiliated with Zhejiang University. We planned to observe circulating nurses that attended to general anaesthesia and posterior lumbar spine surgery in the prone position for 3 months from October to December 2020 and then monitor them attending to the same events using the newly developed checklist for 3 months from January to March 2021. Circulating nurses were eligible for inclusion in the study if (a) they were a registered nurse at the study site with more than 2 years of OR work experience, (b) they completed training related to this study and passed the required assessment, and (c) they volunteered to participate in the study and completed the informed consent form. The exclusion criterion was OR head nurse.
The study site was selected based on its sufficient volume of general anaesthesia and prone position surgery, the general availability of supplies, its motivated leadership and the absence of other ongoing interventions. After the pre-intervention period, one investigator of the multi-disciplinary team introduced the checklist to the circulating nurses during the 1-day learning session and monitored its ongoing use. Learning was supported by lectures, written materials, an instructional video and direct guidance. The OR nursing department was responsible for the endorsement of the checklist.
2.3.1 Data collection
Patient demographic characteristics, including age, sex, body mass index and operative duration were collected from the electronic medical record system. One nursing college student who was free of responsibility at the study hospital and unknown to the circulating nurses was chosen to be the data collector before and after the intervention and taught by the investigator to observe and document the circulating nurse's practice during the procedure. Nurses were pre-informed to be observed, but they did not know the exact observer. Nursing practice was considered to be performed when the nurse correctly performed the appropriate practice during the required period of verification. Failure to perform measures, such as due to an omission, error or perform the action during the incorrect period, was considered non-performance. Observation data were recorded on standardized data sheets by data collector who directly observed the nurses. The observation took place over a 12-hr period on weekdays from the time the patient entered the OR to before the patient left the OR. Checklist use was observed during the postintervention period. Data collector did not interact with circulating nurses or patients during observation. For ethical reasons, collector was instructed to notify health workers if she observed a potentially harmful condition or practice. Nurse evaluation of the checklist consisted of six items specifically related to the checklist intervention developed by the core team (“The checklist was easy to use,” “The checklist improved prone position safety,” “The checklist improved prone position nursing care quality,” “The checklist took a long time to complete,” “If I were having a prone position and general anaesthesia operation, I would want the checklist to be used,” and “The checklist helped prevent prone position injury”) and were included only in the postintervention version of the survey. One item (“The checklist took a long time…”) was reverse scored to calculate summary statistics.
2.4 Statistical analysis
Analyses were performed using SPSS20.0 software (IBM Corp.). Chi-Squared tests were used to evaluate whether the delivery rate had different distributions before and after implementing the new checklist. A p-value less than .05 was considered statistically significant.
3 RESULTS
3.1 Checklist development
3.1.1 Literature review and quality evaluation
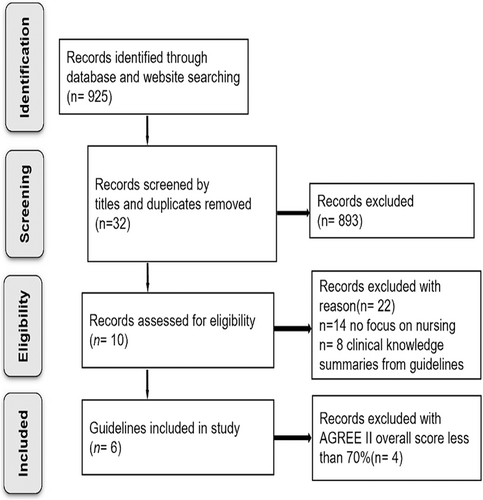
A total of 925 guidelines were initially obtained from the databases. 10 guidelines that addressed general anaesthesia and the prone position and were assessed with the AGREE II instrument. Six guidelines (Table S1) fulfilled the inclusion criteria (see Figure 2 for the search process). Table S2 shows the scores obtained using the guidelines as percentage scores.
3.1.2 Delphi expert consultation
A two-round Delphi expert consultation was performed to explore the views of experts on issues relating to this study. Twenty experts with sound theoretical knowledge and excellent practical skills in OR nursing, orthopaedics, and anaesthesiology were selected. The average age of the experts was 43, and their average working time was 20.2 years. They worked in different regions of China: Hangzhou (8), Huzhou (5), Nanchang (4), Wuhan (3). After two Delphi rounds, the panellists identified four pause points and revised two items in the draft. A pause point is the point in the process of caring for a patient when it is appropriate to pause to check that the item on the checklist has been completed. The four pause points were “before prone positioning,” “after prone positioning,” “during the operation,” and “before leaving the OR.” Two items were modified, “four caregivers should be available for a supine-to-prone patient transfer” was changed to “four caregivers must be available for a supine-to-prone patient transfer, including an anaesthetist responsible for the patient's head and tube,” because four caregivers are much safer for supine-to-prone patient positioning. The other change was from “when operating time is longer than 3 h, reposition the patient every 2 hr” to “when operating time is longer than 3 hr, communicate with the anaesthetist and the surgeon as to whether the patient should be repositioned every 2 hr,” because if the patient position is changed without communication with anaesthetist and surgeon, surgical safety and anaesthesia tube position may be jeopardized. Based on the results of the Delphi round, the second edition of GAPPNC was confirmed, which included four pause points and 21 practices (Table S3).
3.1.3 Field test
Nurse evaluations of the checklist were as follows: the average time taken to complete the checklist was 3.5 min per phase; the content of the checklist was complete, and its items were logically arranged, and the guidelines were expressed in a concise and clear manner. Two suggestions were proposed. The team members discussed the nurses' feedback and made two modifications. The first was to add an item during the immediate after prone positioning period that states that “Parts of the body that do not require treatment are covered.” The nurse thought this item was easy to forget but important for patient warmth. The CPGs also mentioned that unnecessary exposure of patients during patient positioning should be avoided, and that covering the patient not only protected their privacy but also benefited their early postoperative recovery (Stanton, 2022). The second change was that “assess the patient's vision after recovery” was changed to inform the postanaesthesia care unit (PACU) staff that patient's vision and peripheral nerve function must be assessed after recovery as the nurses believed that most patients were still under anaesthetic before leaving the OR, it was best to remind the PACU staff to complete this task to improve OR efficiency. After these revisions, the final edition of the GAPPNC (Table 1) included 22 measures over four stages: before prone positioning (5 items), after prone positioning (12 items), during operation (3 items) and before leaving the OR (2 items). Content involved standard patient positioning, privacy protection, hypothermia prevention, patient assessment, electric surgical safety, prevention of peripheral nerve and optic nerve injury, and perioperative stress. The content also covered the most basic and necessary nursing interventions to avoid preventable complications from the prone position.
| 1. Before prone positioning | 2. After prone positioning |
|
Positioning equipment is available, dry, smooth and intact, and in proper function □ Yes The patient is in limitation of motion □ Yes □ No The patient's skin is intact □ Yes □ No Operating bed and transport vehicle are locked, side rails are raised □ Yes Four caregivers must be available for a supine-to-prone patient transfer (an anaesthetist responsible for the patient's head and tube) □ Yes |
Head is level with or higher than heart □ Yes Head, neck, and trunk are a neutral position □ Yes All the tubes are intact and function properly □ Yes The padded headrest, chest rolls (i.e., from clavicle to iliac crest), and safety trap (i.e., 5 cm above the knee) are used □ Yes Positioning equipment is smooth and dry □ Yes Eyes are closed and uncompressed □ Yes Arms are placed on padded boards with the arms abducted to less than 90 degrees or placed at the side of the body, with the elbows flexed and the palms facing downwards □ Yes Body is protected from touching metal portions of the procedure bed □ Yes Face, breast, or male genitalia are free from torsion or pressure □ Yes Shins are padding high enough to avoid pressure on the tips of the toes □ Yes Elbows, hands and knees are padded □ Yes Parts of the body that do not require treatment are covered □ Yes |
| 3. During operation | 4. Before leaving the operating room |
|
Remind doctors not to put pressure on patients when not operating (i.e., lean on patients, surgical instruments, objects on patients) □ Yes □ Not applicable Operating time is longer than 3 hours □ Yes, when operating time is longer than 3 hr, communicate with the anaesthetist and the surgeon as to whether the patient should be repositioned every 2 hr □ No, less than 3 hr Reassess all the items of the second stage after repositioning or any movement of the patient, procedure bed, or equipment attaches to the bed □ Yes, already reassessed □ Not applicable |
Patient developed new pressure injury □ Yes □ No Inform the postanaesthesia care unit staff that patient's vision and peripheral nerve function must be assessed after recovery □ Yes |
3.2 Checklist testing
3.2.1 Demographic characteristics
We observed 72 nurses attending to 84 surgeries during the baseline period (October–December 2020), and 87 surgeries after introduction of the checklist (January–March 2021). Table 2 lists patient characteristics. There were no statistically significant differences between the patients in the two phases of the study. All nurses involved in the study were invited to participate and agreed to do so, and there was no nurse turnover during this study. Nurse demographic characteristics are shown in Table 3. The pre- and postintervention periods did not overlap, and data were not collected during the brief period when the program was introduced.
| Characteristics | Before (N = 84) | After (N = 87) | p value |
|---|---|---|---|
| Age | 55.94 ± 6.77 | 55.15 ± 7.01 | .499 |
| Sex (%) | |||
| Female | 38.10 | 41.38 | .661 |
| Male | 61.90 | 58.62 | |
| Body mass index | 22.22 ± 3.80 | 22.77 ± 3.24 | .163 |
| Operative duration (min) | 184.07 ± 31.18 | 191.01 ± 32.59 | .573 |
| Characteristics | N (%) |
|---|---|
| Gender | |
| Male | 9 (12.50) |
| Female | 63 (87.50) |
| Age | |
| 22–29 | 33 (45.83 |
| 30–39 | 27 (37.50 |
| 40–49 | 10 (13.89 |
| ≥50 | 2 (2.78 |
| Years of working | |
| 3–5 | 21 (29.17 |
| 5–10 | 35 (48.61 |
| >10 | 16 (22.22 |
| Job title | |
| Junior nurse | 6 (8.33 |
| Senior nurse | 43 (59.72 |
| Supervisor nurse | 23(31.94 |
| Education level | |
| College degree | 13 (18.06 |
| Bachelors' degree | 54 (75.00 |
| Master or above | 5 (6.94 |
3.2.2 Feasibility and evaluation of the checklist
There was a statistically significant difference in the rate of successful delivery of essential prone positional nursing practices following the introduction of the checklist. Sixteen out of 22 essential practices were performed prior to use of the checklist, yielding an implementation rate of 72.72%. With the use of the checklist, an average of 21 essential practices was implemented, resulting in an implementation rate of 95.45% and an increase of 22.73% in the implementation of measures (χ2 = 4.247, p = .039).
Table 4 shows the rates of successful completion of individual practices before and after introduction of the checklist. Compliance rates for three measures were 100%, and delivery rates for 14 practices improved significantly, including items 1, 2, 3, 10, 11, 13, 14, 16, 17, 18, 19, 20, 21 and 22.
| Intervention (N = 22) | Before | After | χ2 | p | ||
|---|---|---|---|---|---|---|
| Number | Rates of delivery, % | Number | Rates of delivery, % | |||
| 1. Positioning equipment is available, dry, smooth and intact, and in proper function | 64/84 | 76.19 | 85/87 | 97.70 | 17.640 | .000 |
| 2. The patient is in limitation | 22/84 | 26.19 | 80/87 | 91.95 | 76.792 | .000 |
| 3. The patient's skin is intact | 65/84 | 77.38 | 87/87 | 100.00 | 22.138 | .000 |
| 4. Operating bed and transport vehicle are locked, side rails are raised | 81/84 | 96.43 | 86/87 | 98.85 | 1.097 | .295 |
| 5. Four caregivers must be available for a supine-to-prone patient transfer | 70/84 | 83.33 | 79/87 | 90.80 | 2.128 | .145 |
| 6. Head is level with or higher than heart | 78/84 | 92.86 | 82/87 | 94.25 | 0.138 | .710 |
| 7. Head, neck, and trunk are in a neutral | 82/84 | 97.62 | 87/87 | 100.00 | 2.096 | .148 |
| 8. All the tubes are intact and function properly | 77/84 | 91.67 | 83/87 | 95.40 | 0.991 | .320 |
| 9. The padded headrest, chest rolls and safety trap are used | 75/84 | 89.29 | 79/87 | 90.80 | 0.110 | .740 |
| 10. Positioning equipment is smooth and dry | 47/84 | 55.95 | 83/87 | 95.40 | 36.489 | .000 |
| 11. Eyes are closed and uncompressed | 56/84 | 66.67 | 84/87 | 96.55 | 25.717 | .000 |
| 12. Arms are placed on padded boards with the arms abducted to less than 90 degrees with the elbows flexed and the palms facing downwards | 67/84 | 79.76 | 75/87 | 86.21 | 1.261 | .262 |
| 13. Body is protected from touching metal portions of the procedure bed | 80/84 | 95.24 | 87/87 | 100.00 | 4.242 | .039 |
| 14. Face, breast, or male genitalia are free from torsion or pressure | 72/84 | 85.71 | 83/87 | 95.40 | 4.729 | .030 |
| 15. Shins are padding high enough to avoid pressure on the tips of the toes | 74/84 | 88.10 | 81/87 | 93.10 | 1.264 | .261 |
| 16. Elbows, hands and knees are padded | 62/84 | 73.81 | 82/87 | 94.25 | 13.433 | .000 |
| 17. Parts of the body that do not require treatment are covered | 65/84 | 77.38 | 85/87 | 97.70 | 16.381 | .000 |
| 18. Remind doctors not to put pressure on patients when not operating | 13/50 | 26.00 | 33/43 | 76.74 | 23.814 | .000 |
| 19. Operating time is longer than 3 hr | 4/42 | 9.52 | 33/47 | 70.21 | 33.632 | .000 |
| 20. Reassess all the items of the second stage after repositioning or any movement of the patient, procedure bed, or equipment attaches to the bed | 2/25 | 8.00 | 15/19 | 78.95 | 29.866 | .000 |
| 21. Patient developed new pressure injury | 58/84 | 69.05 | 79/87 | 90.80 | 12.700 | .000 |
| 22. Inform the postanaesthesia care unit staff that patient's vision and peripheral nerve function must be assessed after recovery | 0/84 | 0.00 | 84/87 | 96.55 | 159.410 | .000 |
Table 5 shows the evaluations of the checklist by 72 nurses. 91.7% of nurses thought the checklist was easy to use, while only 8.3% felt it was difficult to use. A majority thought that the checklist improved general anaesthesia and prone position surgery safety and nursing care quality (97.2% and 90.3% respectively), and 93.1% agreed that the checklist helped prevent a general anaesthesia and prone positional injury. Only 16.7% of nurses thought that it would take a long time to complete the checklist. A large majority (94.4%) would want the checklist to be used if they were having a general anaesthesia and prone position operation, while only four respondents (5.6%) disagreed with this statement.
| Evaluation | Agree | Disagree, neutral or no answer | ||
|---|---|---|---|---|
| N | % | N | % | |
| The checklist was easy to use | 66 | 91.7 | 6 | 8.3 |
| The checklist improved prone position safety | 70 | 97.2 | 2 | 0.28 |
| The checklist improved prone position nursing care quality | 65 | 90.3 | 7 | 9.7 |
| The checklist took a long time to complete | 12 | 16.7 | 60 | 83.3 |
| If I were having a prone position and general anaesthesia operation, I would want the checklist to be used | 68 | 94.4 | 4 | 5.6 |
| The checklist helped prevent prone position injury | 67 | 93.1 | 5 | 6.9 |
4 DISCUSSION
Our study found that the GAPPNC is an effective tool for translating evidence into practice and standardizing the general anaesthesia and prone positioning nursing process and practice. International prone position guidelines were recognized as standard of care for patient positioning care (Spruce, 2021), while some recommendations by the CPGs were hard to apply to daily practice due to their complex content or incompatibility with local clinical practice (McArthur et al., 2021). The WHO therefore recommended that healthcare providers use a medical checklist for translating evidence into practice (Röhsig et al., 2020). We followed the WHO-recommend medical checklist development model to develop a GAPPNC based on high-quality CPGs, multidisciplinary expert opinions and frontline nurse experience. The checklist established four pause points to check 22 necessary items during the prone position nursing process, which can assist nurse to provide standardized, continuous and evidence-based prone positioning care in daily practice.
Implementation of the GAPPNC was associated with statistically significant improvement in the delivery of essential prone positional practices and improved nursing quality. The rate of the successful delivery of 22 essential practices significantly improved. The delivery rate of 14 measures achieved a statistically significant improvement. These findings are similar to those of other studies (Tsai & Tsai, 2018). Previous prone position studies or training usually aim to prevent one particular complication or to introduce the prone positioning method (Chui et al., 2018; Haleem et al., 2020; Woodfin et al., 2018), but not analyse the high-risk factors and measures during each stage of prone positioning. As a result, the nurse's prone positioning theoretical and practice level knowledge depends on their own knowledge and experience with this position. We therefore divided the prone positioning nursing process into 4 stages and identified 22 necessary items for patient safety. This tool can help the nurse quickly understand the whole prone positioning care procedure and its essential measures and then provide comprehensive and safe prone positioning care as part of daily practice (Lane et al., 2021; Vena et al., 2020). The quality of nursing in this position has consequently greatly improved.
Majority of nurses who used the checklist had a positive view of the tool. Most of them felt that the checklist was easy to use and recognized its value in ensuring patient safety. This may also explain why almost all nurses responded that they wanted the checklist to be used during their own care, including some who were against using the checklist. This fundamental perception of the value of a checklist at providing safe patient positioning care suggests that a well-designed checklist and implementation program can be successful at achieving nurse acceptance and use (Haynes et al., 2011). We believe that our research process can be used as an example for future similar checklist development and implementation studies.
5 CONCLUSIONS
In summary, our study developed a GAPPNC for use by the circulating nurse based on a scientific checklist development model and 6 high-quality CPGs. This checklist can improve the delivery of evidence-based practice, translate such evidence into practice, standardize the nursing process and be positively perceived by most nurses.
6 LIMITATIONS AND FUTURE RESEARCH
This study was performed at only one hospital for half a year. The checklist's effects of increasing the implementation of high importance measures, improving nursing quality and transforming CPGs have been affirmed to some extent, but its long-term effects, especially at decreasing the incidence of complications, remain to be verified. A variety of similar studies have shown that the long-term use of a medical checklist can effectively improve safety awareness, avoid medical errors and reduce the incidence of complications and mortality (Storesund et al., 2020). It is therefore necessary to perform multi-centre studies in the future. Besides, the Hawthorne effect is an improvement in performance due to subjects' knowledge of being measured. The contribution of the Hawthorne effect is difficult to disentangle in this study. However, similar study argued against this possibility: this knowledge was in place before and after checklist introduction. Besides, according to our nurse's evaluation of the GAPPNC, they would want the checklist to be used during their own care. So, we considered the presence of study personnel in the OR was not responsible for the change of implementation rate (Haynes et al., 2009).
AUTHOR CONTRIBUTIONS
Jianshu Cai: Made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data. Jianshu Cai and Xiaoling Huang: Involved in drafting the manuscript or revising it critically for important intellectual content. Jianshu Cai and Lifang He: Given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content. Lifang He: Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FUNDING INFORMATION
This study was supported by the National Undergraduate Innovation and Entrepreneurship Training Program (No. 202110545029), Sir Run Run Shaw Hospital Nursing Research Foundation (No. 201708HL and No. 202130HLGL).
CONFLICT OF INTEREST
There is no conflict of interest to report.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was performed following approval by the Ethics Committee of Sir Run Run Shaw Hospital of Zhejiang University School of Medicine. All participants signed informed consent.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.