Effectiveness of nurse-led discharge service on adult surgical inpatients: A meta-analysis of randomized controlled trials
Huina Mao and Yarui Xie contributed equally to this work.
Abstract
Aim
To determine the effectiveness of nurse-led discharge service for adult surgical inpatients.
Design
The report of this review was conducted by the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement checklist.
Methods
The PubMed, Web of Science, ScienceDirect, Cochrane Library (CENTRAL), MEDLINE and Embase as well as four Chinese databases including CNKI, Wanfang database, VIP database and CBM were searched for randomized controlled trials. Two reviewers independently extracted data and assessed risk of bias. And meta-analyses were conducted for the eligible studies by Review manager 5.4.1.
Results
A total of 1,649 participants were enrolled in 12 randomized controlled trials. The result of readmission rate and emergency visit of intervention group were lower than those of the control group; activities of daily living and quality of life in the intervention group were higher than that of the control group. There was no statistical difference in the length of stay between the two groups.
1 INTRODUCTION
Discharge planning is a process of concentration, coordination and multidisciplinary integration. Through the cooperation of multidisciplinary professionals, patients and their families, patients can get continuous care after discharge (Schick-Makaroff et al., 2021). However, with the wide application of enhanced recovery after surgery (ERAS), the length of hospital stay is shortened for surgical patients, which means that the time for patients to prepare for discharge is also shortened.
The study has shown that patients with higher discharge readiness were associated with lower rates of readmission, mortality and emergency visit (Schmocker et al., 2015). Therefore, it is necessary to give discharge service for these patients. The discharge service is relatively mature in the UK, USA, Canada, etc., and some researchers have applied it to different diseases, such as stroke (Hofstad et al., 2014; Schmocker et al., 2015), mental disorders (Taylor et al., 2016) and hip fracture (Huang & Liang, 2005). The efficacy of discharge services in stroke patients (Shepperd et al., 2013) and in patients with congestive heart failure (Phillips et al., 2004) has been reported in several reviews. However, for surgical patients, are discharge services more effective than routine care?
2 METHODS
2.1 Objectives
The objectives of this review were to evaluate the effectiveness of the discharge service in the surgical patients, analysing if these interventions imply a result in a reduction in the index length of hospital stay and emergency visit, if they produce a benefit on the readmission, if they reduce the emergency visit and secondarily if the discharge service increases satisfaction with discharge service and quality of life.
In order to explore these review objectives, the study applies the patients, interventions, comparison and outcomes (PICO) model for the formulation of clinical questions in the practice based on evidence. Table 1 shows the five PICO questions.
| PICO question | Participants | Intervention/comparison | Result |
|---|---|---|---|
| PICO No.1: Do the discharge service imply a result in reduction in the index length of hospital stay? | Adult surgical patients | Discharge service versus routine hospital care currently (i.e. nothing; wound care; diet education or rehabilitation exercises without brochures or written discharge summaries; no comprehensive assessment; no multidisciplinary coordination; etc.) | Reduction or increase in the index length of hospital stay |
| PICO No.2: Do the discharge service produce any benefit on readmission? | Adult surgical patients | Discharge service versus routine hospital care currently (i.e. nothing; wound care; diet education or rehabilitation exercises without brochures or written discharge summaries; no comprehensive assessment; no multidisciplinary coordination; telephone call; etc.) | Reduction or increase in the discharge readiness |
| PICO No.3: Do the discharge service produce any benefit on the activities of daily living? | Adult surgical patients | Discharge service versus routine hospital care currently (i.e. nothing; wound care; diet education or rehabilitation exercises without brochures or written discharge summaries; no comprehensive assessment; no multidisciplinary coordination; etc.) | Reduction or improvement in the patient’s activities of daily living |
| PICO No.4: Do the discharge service imply any reduction in the number of emergency visit in the surgical patients? | Adult surgical patients | Discharge service versus routine hospital care currently (i.e. nothing; wound care; diet education or rehabilitation exercises without brochures or written discharge summaries; no comprehensive assessment; no multidisciplinary coordination; telephone call; GP- and/or nurse-led follow-up; etc.) | Reduction or increase in the number of emergency visits |
| PICO No.5: Do these discharge services produce any improvement in the quality of life of the surgical patients? | Adult surgical patients | Discharge service versus routine hospital care currently (i.e. nothing; wound care; diet education or rehabilitation exercises without brochures or written discharge summaries; no comprehensive assessment; no multidisciplinary coordination; telephone call; GP- and/or nurse-led follow-up; etc.) | Reduction or improvement in the patient’s quality of life |
2.2 Design
The study was performed in accordance with the guidelines from the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy from the Cochrane Collaboration (Macaskill et al., 2010) and preferred reporting items for systematic review and meta-analysis (PRISMA) (Moher et al., 2009). Our study protocol was registered with the International Prospective Reshuister of Systematic Reviews (PROSPERO) (CRD 42021260834).
2.3 Search strategy and study selection
The electronic databases searched included six English databases and four Chinese databases. Among them, the English databases included PubMed, Web of Science, Science Direct, Cochrane Library (CENTRAL), MEDLINE and Embase. Otherwise, the Chinese databases included CNKI, Wanfang database, VIP database and CBM. The literatures which were published between 1 January 2000 and 31 December 2021 were included. Meanwhile, we also limited the studies to randomized controlled trials and written in English or Chinese, but with no regional restrictions. The two researchers jointly identified the search keywords as “discharge plan,” “discharge service,” “discharge intervention” or “discharge nursing.” Taking PubMed as an example, the search strategy was as follows: (discharge plan) OR (discharge planning) OR (discharge service) OR (discharge intervention) OR (discharge nursing). And the qualification were title, abstract or keywords.
Firstly, we imported the documents retrieved from 10 databases into NoteExpress for duplicate checking. Then, the researchers screened the titles and abstracts of the retrieving documents for preliminary inclusion according to inclusion and exclusion criteria. At last, two researchers read the full text of the preliminary included literature independently and determined whether they were finally included in this analysis. Any disagreement was resolved through consensus between two researchers. When consensus could not be reached, a third researcher independently reviewed the full text of the literature and discussed whether it was included together.
2.4 Inclusion and exclusion criteria
2.4.1 Inclusion criteria
- Language: Chinese and English
- The review considered studies that included adult surgical patients aged 18 years or older, discharged from hospital to home and not for long-term conditions. There was no limit to the type of surgery.
- The current review considered studies that assessed the following nursing discharge planning interventions, including pre-operative nursing, postoperative functional rehabilitation, development of patients' health handbooks and post hospital follow-up. Nurses should lead the discharge planning mainly. In addition, the intervention programmes in the studies need to be detailed.
- The review considered experimental study design including randomized controlled trials.
- Articles that answered at least one PICO question.
2.4.2 Exclusion criteria
- Duplicate articles.
- Not consistent with the present objectives.
- Non-RCTs were excluded.
2.5 Data extraction
All data were independently extracted by two researchers. The following details included were extracted: authors' names, publication year, publication country, number of participants, age, type of surgery, study design, outcomes, follow-up and discharge intervention elements. And two researchers resolved any differences through discussion or by seeking the opinion of a third person to reach a consensus. Finally, the information was integrated into a chart by the researchers based on consensus.
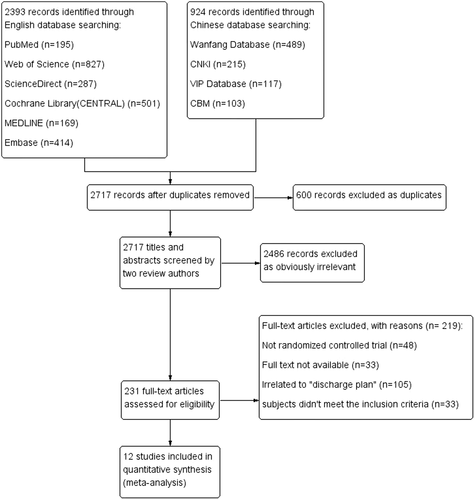
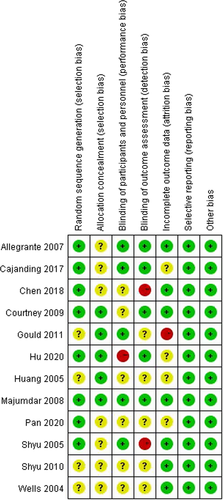
2.6 Risk of bias assessment
The quality of 12 included literature was assessed by two researchers independently using the Cochrane Handbook for Systematic Reviews of Interventions in Review manager 5.4.1. Before assessment, the researchers learned and interpreted the use of the tool (Higgins et al., 2011). It includes seven items: (1) random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessment; (5) incomplete outcome data; (6) selective reporting and (7) other bias. And each item has three options: low risk, high risk and unclear risk. Finally, all assessments were integrated into the risk of bias graph and risk of bias summary.
2.7 Data analysis
Three primary outcomes and two secondary outcomes were analysed as follows. Effect measure depends on data type, and if the data are continuous variables, the weighted mean difference (WMD) or standardized mean difference (SMD) is used; on the contrary, if they are dichotomous variables, odds ratio (OR) or risk ratio (RR) is used. And the heterogeneity represented by I2 between the studies was evaluated before data analysis through chi-square test. The random effects were selected if the heterogeneity between studies was high (I2 ≥ 50, p > .1); otherwise, the fixed effects were selected. For I2 > 50, we further explored the source of heterogeneity through sensitivity analysis by removing studies one by one and carried out funnel plots. Meanwhile, subgroup analysis was performed for outcomes with different follow-up time, such as readmission rate at 1 and 3 months after discharge. A p value <.05 was considered statistically significant.
3 RESULTS
3.1 Search results
A total of 3,317 Chinese and English literatures were retrieved from all databases. Then, 600 duplicate and 2,486 obviously irrelevant literature were excluded. Except for 33 literature for which we could not find the full text, we read the other full text of 198 literature. And 12 literatures giving information on 1,649 participants from six countries were included finally by two researchers according to the inclusion criteria (Figure 1).
3.2 Study characteristics
A total of 1,649 participants with a mean age ranging from 18 to 80 years were enrolled in 12 randomized controlled trials. The males were 37% and females were 63% among the participants. However, one trial did not provide the sex distribution. The types of surgeries that participants received included: joint replacement (knee replacement and hip replacement), breast cancer, percutaneous coronary intervention, fracture, colorectal cancer and kidney transplantation and hip replacement were at most (35.4%). Seven studies were carried out in Asia, three in North America, one in Europe and one in Australia (Table 2).
| Authors (year) | Study design | Country | Participants (I = intervention; C = control) | Outcomes | Interventions | Follow-up (months) |
|---|---|---|---|---|---|---|
| Wells et al. (2004) | RCT | Canada |
|
②⑦ | Nurse-led model of early discharge from hospital |
Time: 2 weeks, 1 month and 1 year Way: telephone |
| Shyu et al. (2005) | RCT | Taiwan, China |
|
①②③④⑥ | An interdisciplinary programme of geriatric consultation, continuous rehabilitation and discharge planning |
Time: 1 and 3 months Way: family visit |
| Huang & Liang, (2005) | RCT | Taiwan, China |
|
①②④⑥ | The discharge planning intervention extended from hospital admission through 3 months after discharge |
Time: 2 weeks, 3 weeks and 3 months Way: no mention |
| Allegrante et al. (2007) | RCT | USA |
|
⑥ | ①A novel, in-hospital, postoperative motivational patient videotape; ②An in-hospital supportive visit by a recovered hip fracture patient; ③A hospital-based, 8-week outpatient programme of physical therapy |
Time: 6 months Way: telephone |
| Majumdar et al. (2008) | RCT | Canada |
|
⑤⑦ | ①Surgeons followed up patients' treatment; ②A brief counselling session to intervention patients by telephone; ③Practice following evidence-based treatment guidelines |
Time: 6 months Way: telephone |
| Courtney et al. (2009) | RCT | Australia |
|
①②③⑤ |
①Comprehensive nursing; ②Physiotherapy assessment and individualized programme of exercise strategies; ③Telephone follow-up commencing in the hospital and continuing for 24 weeks after discharge |
Time: 1, 3 and 6 months Way: telephone |
| Shyu et al. (2010) | RCT | Taiwan, China |
|
②③④ | The interdisciplinary intervention programme included geriatric consultation services, a continuous rehabilitation programme and discharge planning services |
Time: 1, 3, 6, 12, 18 and 24 months Way: telephone |
| Gould (2011) | RCT | UK |
|
①③⑦ | ①A discharge intervention, consisting of written discharge materials and telephone follow-up by an expert cardiovascular nurse; ②The intervention was offered at discharge and continued within 24 hr of discharge |
Time: 24 hr Way: telephone |
| Chen et al. (2018) | RCT | China |
|
①②④ | ①Established a multidisciplinary discharge service team; ②Training of team members; ③Implementation of discharge service; ④Evaluated effects of intervention |
Time: 1 week, 4 weeks, 3 months and 6 months Way: telephone, family visit and outpatient |
| Cajanding (2017) | RCT | The Philippines |
|
①③⑦ | The structured discharge planning programme comprises a series of individualized lecture–discussion, provision of feedback, integrative problem-solving, goal setting and action planning that was implemented by a cardiovascular nurse practitioner |
Time: 1 month Way: no mention |
| Hu et al. (2020) | RCT | China |
|
①③⑦ | ①Patients received a written discharge summary (including the diagnosis and treatment record and post discharge medications, diet and exercise suggestions, etc.) and an oral discharge instruction; ②A weekly post discharge telephone follow-up (for a month) was conducted by ward nurse |
Time: 1, 3 months Way: telephone |
| Pan et al. (2020) | RCT | China |
|
①②③ | ①Establishment of a multidisciplinary discharge service team; ②Built the intervention scheme and make the discharge service form. |
Time: 1 month Way: “Wechat” |
- Note: Outcomes: ①readmission; ②length of stay; ③emergency visit; ④ADL (activities of daily living); ⑤health-related quality of life (SF-12); ⑥health-related quality of life (SF-36) and ⑦patients' satisfaction.
Intervention is a nurse-led discharge service, including perioperative nursing, health education, postoperative rehabilitation, follow-up after discharge and so on. Five studies (Cajanding, 2017; Chen et al., 2018; Hu et al., 2020; Pan et al., 2020; Wells et al., 2004) listed the intervention plans in detail, including time period and specific measures. Four studies (Cajanding, 2017; Chen et al., 2018; Hu et al., 2020; Pan et al., 2020; Wells et al., 2004) among them were described in some stages: perioperative period, pre-discharge phase and postdischarge phase. And two studies (Chen et al., 2018; Pan et al., 2020) included assessment, planning, implementation and evaluation. According to the guideline (ACT Health discharge planning policy), discharge service should be performed in 24 hours after admission. Four studies reported the starting time of discharge service (Chen et al., 2018; Courtney et al., 2009; Huang & Liang, 2005; Pan et al., 2020), and eight studies did not mention. The establishment of multidisciplinary team was reported in six studies (Chen et al., 2018; Courtney et al., 2009; Huang & Liang, 2005; Pan et al., 2020; Shyu et al., 2005; Shyu et al., 2010). Follow-up after discharge can track the rehabilitation and quality of life for patients, which is one of the important parts of the discharge service. Most studies reported the time and the ways of follow-up. Some of the studies used the telephone to follow up (Allegrante et al., 2007; Courtney et al., 2009; Gould, 2011; Hu et al., 2020; Majumdar et al., 2008; Shyu et al., 2010; Wells et al., 2004), and two performed family visit (Chen et al., 2018; Shyu et al., 2005). Most of the patients were followed up for 1 or 3 months (Cajanding, 2017; Hu et al., 2020; Huang & Liang, 2005; Pan et al., 2020; Shyu et al., 2005) after discharge to record readmission rate, emergency visit and activities of daily living. The other studies were followed up for 6 months, even 1 year (Wells et al., 2004) and 2 years (Shyu et al., 2010) after discharge. The primary outcomes in this analysis were the length of stay, readmission rate and emergency visit. Secondary outcomes were activities of daily living and quality of life. Seven studies reported length of stay but only five were available (Chen et al., 2018; Courtney et al., 2009; Huang & Liang, 2005; Shyu et al., 2005; Shyu et al., 2010); eight studies reported readmission rates and seven were available (Cajanding, 2017; Chen et al., 2018; Courtney et al., 2009; Hu et al., 2020; Huang & Liang, 2005; Pan et al., 2020; Shyu et al., 2005) and seven studies reported emergency visit and just four were available (Chen et al., 2018; Hu et al., 2020; Shyu et al., 2005; Shyu et al., 2010). The report of the review used the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement checklist (Moher et al., 2009).
3.3 Risk of bias
As shown in the “risk of bias summary” (Figure 2), “+” means low risk; “−” means high risk and “ ? ” means unclear risk. Eight trials (Allegrante et al., 2007; Cajanding, 2017; Chen et al., 2018; Courtney et al., 2009; Hu et al., 2020; Majumdar et al., 2008; Shyu et al., 2005) were assessed as low risk in random sequence generation because the specific randomized methods were described in the studies, such as tables of random numbers, computerized random number generator or coin toss. The other four trials only simply mentioned random allocation rather than the specific random method. So we assessed them as unclear risk. Five trials implemented allocation concealment (Courtney et al., 2009; Gould, 2011; Hu et al., 2020; Huang & Liang, 2005; Majumdar et al., 2008), which were at low risk. However, seven studies did not indicate clearly whether allocation concealment was carried out. Risk of performance bias is related to blinding of participants and personnel. In 5 of 12 studies (Allegrante et al., 2007; Cajanding, 2017; Gould, 2011; Majumdar et al., 2008; Shyu et al., 2005), blinding of participants or personnel was reported, and was assessed as low risk. As for information bias, it is related to blinding of outcome assessors. Five studies (Allegrante et al., 2007; Cajanding, 2017; Courtney et al., 2009; Hu et al., 2020; Majumdar et al., 2008) at low risk reported the implementation of blinding of outcome assessors and one study did not perform. The other six studies did not provide this information. Follow-up loss was found in all included literature. However, only seven studies (Allegrante et al., 2007; Chen et al., 2018; Courtney et al., 2009; Majumdar et al., 2008; Shyu et al., 2005; Shyu et al., 2010; Wells et al., 2004) performed intention-to-treat analysis (ITT) to reduce risk of attrition bias. Otherwise, two studies (Allegrante et al., 2007; Courtney et al., 2009) analysed the impact of the lost data on the studies. Therefore, the seven studies were assessed as low risk. And the four studies were at unclear risk. All trials were assessed as low risk in selective reporting which leads to reporting bias. Because all the outcomes which the authors wanted to explore were reported to us. Except for the above risk of bias, we did not discover other sources of bias from the included trials.
3.4 Effectiveness of nurse-led discharge service
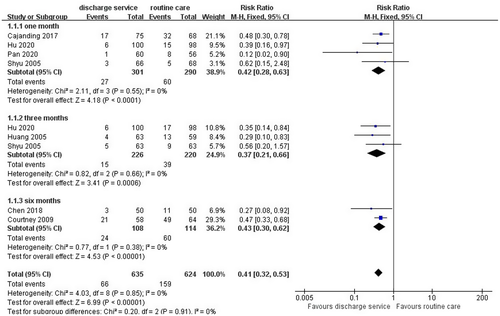
3.4.1 Readmission
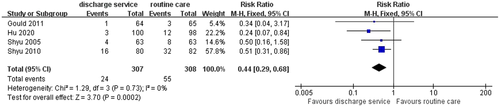
Outcome data were available for seven trials (1,259 participants), in 1 month, 3 months or 6 months of hospital discharge. Fixed effect was selected, because the seven studies were homogeneous (I2 = 0%, p = .85). And the seven studies included in the analysis were all randomized controlled trials, therefore risk ratio (RR) was used as the effect measure at first. The follow-up time between the studies was different, and the subgroup analysis was performed. Comparing with the routine care groups, the results showed that there was a statistically significant reduction in the odds of hospital readmission (RR = 0.41, 95% CI: 0.32–0.53, Z = 6.99, p < .001) in the discharge service group (Figure 3).
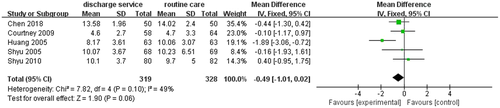
3.4.2 Length of stay
Outcome data were available for five trials (647 participants). The heterogeneity test result showed that I2 < 49%, which was set to fixed effect. Although I2 < 50 (I2 = 49%, p = .10), we further explored the source of heterogeneity through sensitivity analysis by removing studies one by one. Then, we discovered that the study (Huang & Liang, 2005) was the main source of heterogeneity. And the I2 was changed from 49% to 0% after removing the study, while the p-value was still >0.05 (p-value changed from 0.06 to 0.57). Overall, there was no apparent difference in length of stay (LOS) between the intervention group and the control group (WMD = −0.49, 95% CI: −1.01 to 0.02, Z = 1.90, p = .06; Figure 4).
3.4.3 Emergency visit
Outcome data were available for four trials (615 participants). The fixed effect was used with no statistically significant degree of heterogeneity (I2 = 0%, p = .73). The results showed that the rate of emergency visit of the intervention group was lower than that of the control group (RR = 0.44, 95% CI: 0.29–0.68, Z = 3.70, p < .001), and the difference was statistically significant (Figure 5).
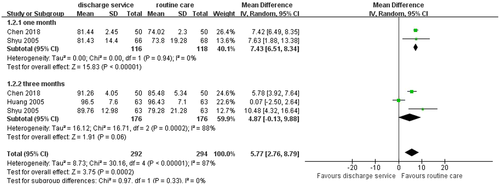
3.4.4 Activities of daily living
Outcome data were available for three trials (460 participants), in 1 month or 3 months of hospital discharge. The three studies measured activities of daily living (ADL) by Barthel Index (BI). The Barthel Index is designed to rate the level of independent functioning for 10 ADLs in individuals with neuromuscular, musculoskeletal disorders or other long-term disorders. Ratings are recorded in the areas of feeding, moving from wheelchair to bed, personal toilet, getting on and off toilet, bathing, walking on level surface, ascending and descending stairs, dressing, controlling bowels and controlling bladder (Mahoney & Barthel, 1965). The total scores are 100. And higher the scores, better the functional independence. We further performed a subgroup analysis because of the different follow-up time, and the results showed that the, total heterogeneity was high (I2 = 87%, p < .10). Then we found out that the study (Huang & Liang, 2005) was the source of heterogeneity by removing the study. The total I2 was changed from 87% to 16% and the p-value was still <0.01. Overall, the difference between the intervention group and control group was statistically significant (WMD = 5.77, 95% CI: 2.76–8.79, Z = 3.75, p < .001; Figure 6).
3.4.5 Quality of life
The 12-item short-form health survey
Outcome data were available for two trials (758 participants). The 12-item Short-Form Health Survey (SF-12) was used to measure the quality of life of patients (Ware et al., 1996). The scale has two main dimensions, namely the physical component and the psychological component. The results showed that the I2 was 97% (p < .1), which indicated that there is a great heterogeneity between the two studies. Sensitivity analysis was not performed because only two studies were included in this outcome. Therefore, the random effect was used as the effect measure. Overall, there was an apparent difference between the two groups (WMD = 7.65, 95% CI: 0.75–14.55, Z = 2.17, p = .03; Figure 7).
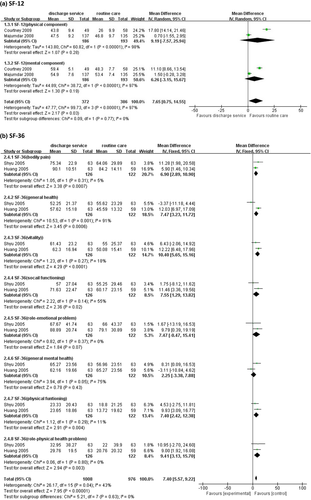
The 36-item short-form health survey
Outcome data were available for two trials (1,984 participants). Scores of this scale for each dimension range from 0 to 100, with higher scores representing better health outcomes (Ware, 2000). And this scale has eight dimensions, so we analysed these data from eight subgroups. The total I2 was less than 50% (I2 = 43%, p = .04), and the fixed effect was selected. Overall, the results showed that the scores of the intervention group were higher than that of the control group (WMD = 7.40, 95% CI: 5.57–9.22, Z = 7.95, p < .001; Figure 7).
3.5 Sensitivity analysis
Sensitivity analyses were performed for each of the other outcomes except quality of life (only two studies included). It was found that the study was the most significant source of heterogeneity in terms of length of stay (Huang & Liang, 2005). Meanwhile, the I2 became 0% and tended to be stable after removing the study. In addition, the heterogeneity of ADL also came from the study (Huang & Liang, 2005), and the I2 was changed from 89% to 16% and tended to be stable after excluding it.
4 DISCUSSION
This review was performed to determine the effectiveness of discharge service on resource use, activities of daily living and quality of life for surgical patients compared with routine care. Meta-analyses showed that the intervention group had a lower readmission rate and emergency visits as well as higher activities of daily living and quality of life, but the length of stay was not statistically significant. The subgroup analyses were also performed according to different follow-up time and dimension of scale in order to reduce bias.
4.1 Resource utilization
Along with limited per capital hold of medical resources and increased requirement of medical services, it is necessary to implement discharge service. And this analysis demonstrated that discharge service reduced hospital resource utilization including readmission rate and emergency visits. It means that discharge service not only reduces waste of medical resources but also the cost of patients and the financial waste of the country. In addition, discharge service not only includes the hospital stage but also emphasizes the resource coordination after the hospital. Especially for some countries with a large population or severe ageing problem, such as China and Japan, the rational use of medical resources is very essential. Medical system and the level of medical development are different in many countries; therefore, patients get different resources after discharge. For China, community health service has been developing continuously in recent year, but still not perfect and universal. And patients are generally discharged at home for rehabilitation and go to comprehensive hospital to solve health problems rather than a local community hospital. From the results of this study, it is suggested that discharge service should be expanded in clinical practice to provide more comprehensive nursing and health care for patients, so as to reduce the waste of medical resources.
4.2 Activities of daily life and quality of life
Patients often suffer from trauma during surgery, which leads to a decline in self-care ability. If the preparation for discharge is inadequate for patients, the length of hospital stay may be prolonged or the recovery after discharge may be more difficult. From the results, ADL and QoL were higher in the intervention group than the control group. But, the heterogeneity test showed that the I2 of SF-12 was 97%. And the sensitivity analysis could not be carried out so that the result may not unreliable. However, the heterogeneity of SF-36 was 46%, indicating that there was heterogeneity among the studies but not high. Overall, we believe that ADL and QOL were statistically significant. Therefore, we should provide patients with health education to teach patients basic rehabilitation exercises and recovery skills. In addition, personalized health manuals for patients can be established in order to follow the health status of patients.
4.3 Strengths and limitations of the review
This analysis focused on surgical patients to explore the effectiveness of discharge services, rather than on patients with long-term diseases. In order to ensure the reliability of the analysis results, subgroup analyses were conducted based on different follow-up times. Meanwhile, sensitivity analyses were performed for the meta-analysis of more than two studies by excluding the studies one by one. And studies with high heterogeneity in the analyses should be carefully considered to exclude. However, only two studies were respectively included in two outcomes of quality of life (SF-12 and SF-36). So the results of this meta-analysis may be unreliable.
Literature search may have missed eligible studies: unpublished grey literature and non-Chinese or English literature were excluded. In addition, some original data form of some studies was not specific and hence the outcome was missing. Lastly, although subgroup analysis and sensitivity analysis were carried out for the outcomes, interventions heterogeneity could not be avoided among the trials, which may have an impact on the results.
4.4 Implications for practice
Discharge service in the intervention group had a positive effect compared to the control group, which should be widely performed in clinical practice. However, the medical system and development degree of each country are different, so it is meaningful to add different elements into discharge service to make it suitable for a country according to the medical characteristics. For example, community hospital and rehabilitation institutions developed early and rapidly, and the patients' post hospital referral should be paid attention to. And hospital discharge service is an essential process for effectively coordinating the transition care from hospital to community (Holland et al., 2013). Therefore, nurses should contact the referral agency to hand over health information in advance under physical conditions and needs of patients so as to make health services continuous.
Meanwhile, with the rapid development of electronic health, network platforms can be a way to provide discharge service to patients. A trial (Cheng, 2017) showed that follow-up based on WeChat (a network application in China) was effective. However, no meta-analysis has been found to prove the effectiveness of health tracking based on a network platform. And more trials should be performed to further explore the effectiveness in the future.
4.5 Implications for future research
This systematic review highlighted that further researches on discharge service are necessary. However, most of the existing trials did not mention the start time of discharge service and the specific intervention method. Moreover, some countries have published guidelines or clinical best practices for discharge service which recommend it should start in 24 hr of admission. And King and Macmillan (1994) proposed that discharge service should include the following four stages: evaluation, planning, implementation and evaluation. Therefore, more well-designed randomized controlled trials are needed, which should clarify specific intervention form, intensity and duration according to guidelines or best practice. In addition, studies should report data in the correct form in more detail to avoid data unavailability, such as mean ± standard deviation (M ± SD). Furthermore, the data should be classified in terms of different follow-up times in order to perform subgroup analyses, such as 1, 3, 6 or 12 months, because follow-up time may lead to different outcome effects for patients.
AUTHOR CONTRIBUTIONS
Research project elaboration: Huina Mao and Yingxia Luo. Study design: Huina Mao, Yarui Xie, Mei Wang and Yingxia Luo. Literature searching and initial records screening: Yarui Xie and Ying Shen. Abstract and article screening for eligibility: Huina Mao, Mei Wang and Yingxia Luo. Data extraction and risk of bias assessments: Huina, Mao Yarui Xie and Yingxia Luo. Manuscript: Huina Mao. Manuscript editing: Mei Wang. All authors read and approved the final manuscript.
ACKNOWLEDGEMENTS
This study was supported by the Nursing research and special project of Southern Medical University [grant number Y2021025].
CONFLICT OF INTERESTS
The authors declare that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
All data included in this study are available upon request by contact with the corresponding author.