Medium Term Outcomes for Robotic Sacral Colpopexy With Autologous Fascia Lata
ABSTRACT
Objectives
To evaluate the medium-term outcomes of robotic sacral colpopexy (RSC) using autologous fascia lata for the treatment of apical pelvic organ prolapse.
Methods
An IRB-approved retrospective review was conducted on patients who underwent RSC with autologous fascia lata at a single institution between November 2017 and August 2022. Only patients with a minimum of 24 months of follow-up were included as short-term results have already been published. Data collected included patient demographics, operative details, surgical complications, Pelvic Organ Prolapse Quantification (POP-Q) measurements, and patient-reported outcomes using the Urogenital Distress Inventory-6 (UDI-6) and Incontinence Impact Questionnaire-7 (IIQ-7). The primary outcome was the medium-term durability of autologous fascia lata RSC, with recurrence defined as > 0 cm from the hymen in any compartment on postoperative POP-Q examination or recurrence at the apex of ≥ 2 cm.
Results
Nineteen patients met the inclusion criteria, with a mean follow-up of 42.8 ± 11.9 months. All POP-Q values showed significant improvement postoperatively, with only one (6.3%) patient experiencing posterior compartment recurrence and one (6.3%) with exactly 2 cm of apical descent. One patient (5.2%) required surgical retreatment with posterior colporrhaphy and a pubovaginal sling. Patient-reported outcomes demonstrated significant improvement in UDI-6 and IIQ-7 scores (p < 0.05). Minor complications related to fascia lata harvest were observed, including seroma (10.5%), transient paresthesia (21%), hematoma (5.2%), and deep vein thrombosis (5.2%), with most resolving spontaneously.
Conclusions
RSC with autologous fascia lata provides durable medium-term anatomic and symptomatic improvement for apical POP, with low recurrence and retreatment rates. While minor harvest-related complications were observed, most were self-limiting. These findings support the use of autologous fascia lata as a viable alternative to synthetic mesh in RSC. Larger, multicenter studies with extended follow-up are needed to further validate these results.
1 Introduction
Sacrocolpopexy (SCP) has been demonstrated to be the most effective and durable repair for apical pelvic organ prolapse [1, 2]. For sacral suspensions, many graft options exist, including porcine dermis, autologous fascia, cadaveric fascia, and synthetic mesh. Although the gold standard is synthetic mesh, mesh erosion remains a concern. The probability of mesh erosion at extended follow-up was reported to be 9.9% in the multicenter CARE trial [3]. Further, following the Food and Drug Administration warning on vaginal mesh due to its risks of related mesh complications, there has been a renewed issue in native tissue repair [4].
We previously reported comparable short-term success rates of SCP with autologous fascia lata with one identified apical failure [5]. Many studies have also shown SCP with autologous fascia lata to be comparable to synthetic mesh in terms of efficacy; however, the studies are limited by small sample size with short-term outcomes [6-9]. To date, there are no robust medium-term studies assessing the durability of autologous fascia lata in SCP. The aim of this study is to present our medium-term outcomes of robotic sacrocolpopexy (RSC) with autologous fascia lata.
2 Materials and Methods
An IRB-approved retrospective review of all fascia lata RSCs performed at a single institution between November 2017 and August 2022 was conducted. Eligible patients included those undergoing RSC with or without concomitant supracervical hysterectomy and/or urethral sling. All patients who underwent RSC during the study period were analyzed, but women with less than 24 months of follow-up were excluded since short-term data has already been described [5, 6].
The decision to use mesh versus autologous fascia lata was the result of an informed discussion between the physician and patient. Patients were educated regarding each approach during preoperative counseling. The associated risks and benefits unique to each were described, including the FDA black box warnings regarding utilization of mesh as well as the risk of seroma, hematoma, thigh numbness, pain, muscle bulge, and deep vein thrombosis associated with fascia lata [4].
Patient data was extracted from medical records and patient surveys. Patient follow-up included 2 weeks postoperatively, 6 weeks, 6 months, then yearly. Data analyzed included preoperative demographics, operative timing, postoperative hospital stay, surgical complications, Pelvic Organ Prolapse Quantification (POP-Q) exam, and patient-reported outcomes including Urogenital Distress Inventory-6 (UDI-6) and Incontinence Impact Questionnaire-7 (IIQ-7) [10]. Follow-up data was established as the last POP-Q exam performed. Patients completed UDI-6 and IIQ-7 inventories at each follow-up appointment and for the purposes of this study, the most recently completed questionnaires were utilized.
POP-Q stage was defined according to standard criteria as defined by the International Continence Society and American Urogynecologic Society [11]. The primary outcome was medium-term failure rates associated with fascia lata RSC. Recurrence was defined as > 0 cm from the hymen in any compartment on postoperative POP-Q exam (Aa, Ba, Ap, Bp). Recurrence at the apex was defined as ≥ 2 cm of apical descent as determined by point C relative to total vaginal length.
2.1 Statistical Analysis
Statistical comparisons were principally performed between preoperative data and at the last follow-up for each patient using a paired t-test. All statistical analyses were conducted with STATA BE version 17 (College Station, TX). Continuous variables were summarized using means and medians. Categorical variables were summarized using frequencies and percentages. Continuous variables were analyzed using a two-tailed t-test. A p-value less than 0.05 was considered statistically significant.
3 Results
3.1 Baseline Characteristics
A total of 35 patients elected to undergo RSC with autologous fascia lata from 2017 through 2022. Nineteen (54.3%) had greater than 2 years of follow-up and were included in this study to determine the medium-term durability of fascia lata RSC. Median follow-up for included patients was 48 months (range 24−60).
Baseline clinical characteristics are summarized in Table 1. The mean age was 57.5 years and BMI was 26.7. Mean parity was 2.5 ( ± 1.5). Seven (36.8%) patients had prior pelvic surgery and nine (47.4) with a prior hysterectomy.
| Variable | Fascia (N = 19) |
|---|---|
| Agea | 57.5 (37−83) |
| Follow-upa | 42.8 (24−60) |
| BMIa | 26.7 (18.2−33.9) |
| Paritya | 2.5 (1−4) |
| Prior hysterectomy | 9 (47.4%) |
| Prior pelvic surgery | 7 (36.8%) |
| Operative time (min)a | 269.5 (175−365) |
| Fascia harvest time (min)a | 24.4 (11−40) |
| Estimated blood loss (mL)a | 25 (10−50) |
| Concomitant supracervical hysterectomy | 10 (52.6%) |
| Concomitant fascia sling | 6 (31.6%) |
| Length of stay (days)a | 0.8 (0−2) |
- Abbreviation: BMI, body mass index.
- a Summarized by mean (range).
Preoperatively, pelvic measurements according to POP-Q exam are described in Table 2. At the time of surgery, all patients had ≥ 2 cm apical descent with a median POP-Q stage of 2 (range 2−4). Preoperative patient questionnaires including UDI-6 and IIQ-7 are displayed in Table 2.
| Variable | Preoperative | Postoperative | p value |
|---|---|---|---|
| UDI-6a | 10.1 ± 4.2 | 4.6 ± 3.4 | < 0.001 |
| IIQ-7a | 9.3 ± 9.0 | 1.5 ± 2.8 | < 0.05 |
| POP-Q valueb | |||
| Aa | 0 (2 to −3) | −2 (0 to −3) | < 0.001 |
| Ba | 1 (3 to −3) | −2 (0 to −3) | < 0.001 |
| Ap | −1 (2 to −3) | −2 (0 to −3) | 0.2 |
| Bp | −1 (3 to −3) | −2 (1 to −3) | < 0.05 |
| C | −6 (−4 to −8) | −8 (−6 to −10) | < 0.001 |
| TVL | 8 (6 to 10) | 9 (6 to 11) | 0.3 |
| POP-Q stageb | 2 (2 to 3) | 1 (0 to 2) | 0.001 |
| Stage 0 | 0 | 3 (15.8%) | |
| Stage 1 | 0 | 3 (15.8%) | |
| Stage 2 | 12 (63.2%) | 13 (68.4%) | |
| Stage 3 | 6 (31.6%) | 0 | |
| Stage 4 | 1 (5.3%) | 0 | |
- Abbreviations: IIQ-7, incontinence impact questionnaire-7; UDI-6, urogenital distress inventory-6.
- a Summarized by mean (standard deviation).
- b Summarized by mean (range).
3.2 Operative Details
All cases were performed robotically. Mean total operative time was 269.5 min and mean fascial harvest time was 24.4 min (Table 1). At the time of fascia lata RSC, 10 (52.6%) patients underwent concurrent supracervical hysterectomy and six (31.6%) underwent fascia sling. One (5.3%) patient underwent posterior colporrhaphy at the time of fascia lata RSC. Mean length of stay was 0.8 days.
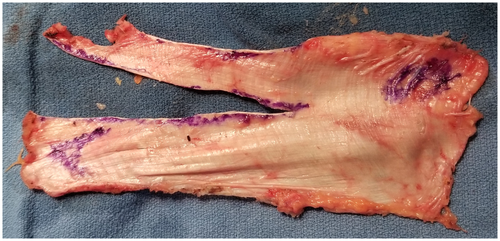
The average length of the graft was 14.4 cm and the width was 4.8 cm. Fascia was secured to the vaginal wall using a running delayed absorbable 2-0 monofilament suture and to the sacrum using three nonabsorbable 0 monofilament sutures as described previously [5]. Figure 1 demonstrates a representative graft and the harvest site, while Figure 2 demonstrates how the graft is configured. Figure 3 demonstrates the postoperative appearance. Fascia lata harvest was associated with one Clavien grade 2 complication. There were two (10.5%) patients that developed a seroma which resolved, four (21%) that endorsed temporary paresthesia, one (5.2%) that developed a hematoma, and one (5.2%) that developed a deep vein thrombosis which was managed with anticoagulation. Ten (52.6%) patients had no adverse events associated with the fascia harvest. At the longest term follow-up visit, there were no ongoing complaints with the fascia lata harvest site.


3.3 Medium-Term Outcomes
Postoperatively, pelvic measurements according to POP-Q exam at the most recent follow-up are displayed in Table 2. All POP-Q values showed durable improvement from preoperative values over a medium-term timeframe. There were no failures in the anterior compartment, one (6.3%) failure in the posterior compartment, and one (6.3%) recurrence at the apex with exactly 2 cm of apical descent. These failures occurred in the same patient at 37 months postoperatively. This patient was symptomatic from the posterior vaginal bulge to Bp +1 as well as stress incontinence and underwent subsequent posterior colporrhaphy with pubovaginal sling. Patient-reported outcomes based on standardized questionnaires showed significant improvement over medium-term follow-up (p < 0.05).
4 Discussion
Prior studies on fascia lata RSC have focused on short-term outcomes, whereas this study specifically selected patients with greater than 2 years follow-up with an average follow-up of 42.8 months. To the best of our knowledge, this is the first study to report medium-term outcomes of autologous fascia lata RSC.
We found that RSC with autologous fascia lata showed durable medium-term improvements in both patient-reported and anatomic outcomes. Patients reported a significant improvement in quality of life on standardized questionnaires, and POP-Q measurements demonstrated anatomical improvement. Of the 19 patients, only one patient underwent surgical retreatment for posterior compartment prolapse and stress incontinence. Our results echo those of an abstract published by Rajamaheswari et al. in 2018 highlighting the results of their randomized controlled trial comparing autologous fascia lata to synthetic mesh in open SCP [12]. From data analysis from 2009 to 2012, they found that 28 out of 30 patients who underwent autologous fascia lata SCP had all POP-Q measurements less than −2 at a follow-up of 3 years. Furthermore, all patients reported complete resolution of bladder, bowel, and sexual symptoms. However, the study had significant limitations, namely, that it was a published abstract with no follow-up manuscript published. Due to the nature of abstracts, it is difficult to evaluate the methodology of the study. Second, standardized questionnaires were not used to assess patient-reported outcomes, making it difficult to truly assess patient's quality of life postoperatively.
Other studies on biologic grafts with outcomes from more than 2 years of follow-up have been published in the literature. Wang et al. reported on the objective and subjective outcomes of 132 women who underwent open SCP with autologous rectus fascia, with a mean follow-up of 27.9 ± 20.5 months [13]. Similar to our findings, their study demonstrated significant improvement in all POP-Q measurements and patient-reported standardized questionnaires. At follow-up, 0.8% had stage 3 prolapse and none had stage 4 prolapse. Additionally, 5% of patients in their cohort underwent surgical retreatment, matching the rate observed in our study.
Autologous rectus fascia serves an alternative biologic graft material; however, its harvest in Wang et al.'s study required a 12 cm skin incision, whereas fascia lata graft harvest in our study required only a 4 cm incision [13]. This difference has important implications for postoperative pain and recovery. Furthermore, while Wang et al. did not report any incisional hernias, such complications have been documented following rectus fascia harvests. We also reported immediate postoperative complications at the fascia lata harvest site, though all were self-limiting, and at the longest term follow-up, there were no ongoing issues. These potential risks underscore the importance of thorough preoperative counseling to help patients weigh the benefits and drawbacks of different graft materials.
Among biologic grafts, dehydrated cadaveric fascia lata has been shown to have a significantly lower anatomic success rate when compared to mesh at 5-year follow-up in a randomized controlled trial (62% vs. 93%, p = 0.02) [14]. Despite this, clinical success rates were found to be comparable between the two graft materials (90% vs. 97%, p = 0.61) [14]. Notably, only one patient (3%) required surgical retreatment. Although the original study had a double-blinded randomized design, patients informed of their graft material at the 1-year follow-up visit, which may have influenced reported clinical success rates. Additionally, clinical success was assessed using indirect questions rather than standardized questionnaires. These results have led to the hypothesis that cadaveric fascia lata may act as an immunologic material, compromising tissue integrity over time.
Our study has several limitations, including data collection from a single institution and a relatively small sample size. We suspect that some patients were lost to follow-up due to the COVID-19 pandemic, which overlapped with the first half of our data collection period. Additionally, because all procedures were performed by a single surgeon, our findings may not be generalizable to a broader population. Despite these limitations, the use of objective POP-Q measurements and standardized patient-reported outcome measures (UDI-6 and IIQ-7) helped reduce investigator bias during data analysis. However, an additional limitation is the absence of a validated questionnaire targeting pelvic floor symptoms, which was unfortunately not utilized in our office setting.
5 Conclusion
This study provides the first medium-term assessment of RSC with autologous fascia lata, demonstrating durable anatomic and patient-reported improvements. Our findings suggest that autologous fascia lata is a viable alternative to synthetic mesh, with low recurrence and retreatment rates over an average follow-up of 42.8 months. While minor complications related to fascia harvest were observed, all were self-limiting. Despite the study's limitations, including its single-surgeon, single-institution design and small sample size, these results contribute valuable insights into the long-term durability of autologous fascia lata SCP. Further multicenter studies with larger cohorts and longer follow-up are warranted to confirm these findings and better define the role of autologous fascia lata in pelvic organ prolapse repair.
Author Contributions
Ramzy T. Burns: data curation, conceptualization roles/writing – original draft, and writing – review and editing. Morgan Black: roles/writing – original draft, and writing–review and editing. Ginnie Jeng: conceptualization, data curation, methodology roles/writing – original draft, and writing – review and editing. Charles R. Powell: conceptualization, project administration, supervision, writing – review and editing.
Acknowledgments
The authors have nothing to report.
Ethics Statement
This retrospective data review was approved by the Institutional Review Board (IRB number 20098).
Consent
The authors have nothing to report.
Conflicts of Interest
Charles R. Powell: Medtronic—investigator; Neuspera—investigator; AUA Practice Guidelines Committee—member; Oakstone Medical Publishing—editor; Wiley Publishing—editorial board; Springer Publishing—section editor. The other authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data is stored in a centralized REDCap database and is available at request.




