Ultrasound-assisted prompted voiding care for managing urinary incontinence in nursing homes: A randomized clinical trial
Abstract
Aims
To determine whether ultrasound-assisted prompted voiding (USAPV) care is more efficacious than conventional prompted voiding (CPV) care for managing urinary incontinence in nursing homes.
Methods
Thirteen participating nursing homes in Japan were randomized to CPV (n = 7) or USAPV care group (n = 6). Residents of the allocated nursing homes received CPV (n = 35) or USAPV (n = 45) care for 8 weeks. In the CPV group, caregivers asked the elderly every 2-3 h whether they had a desire to void and prompted them to void when the response was yes. In the USAPV group, caregivers regularly monitored bladder urine volume by an ultrasound device and prompted them to void when the volume reached close to the individually optimized bladder capacity. Frequency-volume chart was recorded at the baseline and after the 8-week intervention to measure the daytime urine loss.
Results
The change in daytime urine loss was statistically greater in the USAPV (median, −80.0 g) than in the CPV (median, −9.0 g; P = .018) group. The proportion of elderly individuals whose daytime urine loss decreased by >25% was 51% and 26% in the USAPV and CPV group, respectively (P = .020). Quality-of-life measures of elderly participants showed no significant changes in both groups. The care burden scale score of caregivers was unchanged in the USAPV group (P = .59) but significantly worsened in the CPV group (P = .010) after the intervention.
Conclusions
USAPV is efficacious and feasible for managing urinary incontinence in nursing homes.
1 INTRODUCTION
Urinary incontinence (UI) is common in community-dwelling and institutionalized elderly populations, with a prevalence ranging from 25% to 50%.1, 2 UI is associated with multiple health problems, such as dermatitis,3 falls,4 lower activity of daily living,5 longer hospital stays, and higher mortality,6 thus impairing patients’ quality of life (QOL) and dignity.7 In addition, management of UI imposes a heavy burden on the society because of the need for human and financial resources.8, 9 Changing diapers is one of the most stressful tasks for care workers.9
Management of UI in elderly individuals usually involves the use of absorbents and toileting programs such as bladder training, habit retraining, timed voiding, and prompted voiding (PV).10 In PV care, care workers regularly prompt elderly individuals to void and provide positive feedback for appropriate voiding. PV is recommended by the International Consultation on Incontinence as an effective modality for the care of nursing home residents and home-care clients. However, the efficacy of PV is limited11; less than 30% of cases achieve reduction in absorbent use.12 More efficacious and feasible care for UI in elderly populations is an urgent need in the globally aging society.
In this decade, we developed an ultrasound-assisted prompted voiding (USAPV) care program for the management of UI in elderly individuals; care workers regularly monitor the intravesical urinary volume of elderly individuals via ultrasonography, and prompt to void when the volume reaches the pre-fixed optimal value. Regular monitoring of intravesical urine volume may prevent delayed prompting or non-voiding in the toilet. In previous studies, the USAPV method was found to reduce absorbent consumption in 63% (50/80) of hospitalized incontinent adults13 and 52% (40/77) of nursing home residents.14 However, these studies lacked controls receiving conventional prompted voiding (CPV) care. In the present randomized clinical trial, we aimed to compare the efficacy and feasibility between USAPV and CPV for UI care in nursing home residents.
2 MATERIALS AND METHODS
At first, we recruited participant nursing homes. Then, using a random number table, we randomized the nursing homes into the CPV and USAPV groups with a ratio of 1:1 in the geographical clusters of western and eastern parts of Japan. All residents were assessed for care-needs level (1 [mild] to 5 [severe]), which has been defined by the Long-Term Care Insurance system, a public social service for elderly individuals in Japan.15 Elderly individuals with care-needs levels of 1-3 are usually ambulant or partially dependent, whereas those with care-needs levels of 4 or 5 are almost dependent.16
We recruited residents to participate in the trial from September 1, 2015 to September 30, 2016. The inclusion criteria for residents were as follows: (a) aged 65 years and older; (b) care-needs level of 1 or more; (c) using pads or diapers because of UI; and (d) post-void residual urine volume of less than 300 mL. Individuals with serious consciousness disorder, acute phase disease, end-of-life care, or a mass in the lower abdomen (eg, pelvic tumor, pelvic cystic disease, and abnormal ascites detected by ultrasonography) were excluded from recruitment. Written informed consent was obtained from each participant or a family member. Written informed consent was also gained from care workers.
Before the start of the study, the co-morbidities QOL, cognitive function, mental state, depression, physical function, and motivation level were assessed using the Charlson comorbidity index,17 EQ-5D,18 mini-mental state examination (MMSE),19 geriatric depression score (GDS),20 Barthel index,21 and vitality index,22 respectively. In the CPV group, we recorded a frequency-volume chart for 1 day during daytime before the intervention to measure the volume of voided urine and urine loss. Urine loss was determined by weighing the pads on a scale. In the interventional phase, caregivers regularly asked the residents every 2-3 h whether they had a desire to void and prompted them to void when the response was yes. The residents were also allowed to void whenever they had a desire to void. The individuals who were physically unable to visit the toilet were provided physical assistance. In the USAPV group, we measured the amount of residual urine volume at least twice during the recording of the frequency-volume chart by using a portable ultrasound device (BladderScan BVI6100; Verathon, Bothell, WA). The rental cost of BladderScan BVI6100 was 95 USD per month. The sum of the mean values of voided volume and residual volume was considered as the participant's optimal intravesical urine volume for voiding. Subsequently, caregivers regularly monitored the urine volume in the bladder every 2-3 h with an ultrasound device and prompted the participant to void when the volume was more than 75% of the individually pre-fixed bladder capacity. After an 8-week intervention of CPV or USAPV, the frequency-volume chart was recorded for 1 day to measure the daytime volume of voided urine and urine loss. Measures and indices to assess physical and mental conditions were also repeated. The participating care team of five care workers per institution was kept unchanged during the study. The care teams of all nursing homes had a protocol meeting before the start of the study to standardize the care. None of the family members were involved in the intervention.
The primary outcome measures for efficacy were the change in daytime urine loss and QOL assessed using the EQ-5D from baseline to the end of the intervention. The secondary outcome measures were the scores of mental state, depression, physical function, and level of motivation assessed using the EQ-5D, MMSE, GDS, Barthel index, and vitality index, respectively. We also assessed the change in caregivers’ QOL with the SF-12v223 and mental stress for care burden with the visual analog scale (VAS).24 The VAS scores ranged from 0 (not stressful at all) to 100 (very stressful).
The sample size was calculated with the following assumptions: the rates of urine loss reduction were 22% with CPV12 and 52% with USAPV,14 two-sided α = .05, 80% power, and 1:1 ratio of CPV and USAPV. The simulation indicated a sample size of 92 elderly individuals (46 in each group). With an estimated dropout of 20%, 115 elderly individuals were to be recruited.
Statistical analysis was performed using the JMP software, version 13.1.0 (SAS, Cary, NC). Randomization had been performed by a facility based; however, we analyzed data at an individual level. The Wilcoxon rank sum test was used to compare the baseline characteristics, except the sex, between the groups. The chi-squared test was performed to compare the sex between groups. The Wilcoxon signed rank test was used to compare the changes in daytime urine loss; daytime voided volume; EQ-5D, MMSE, GDS, Barthel index, vitality index, SF-12v2, and VAS. We calculated a propensity score including facility and factors in the characteristics of the study participants, with a P-value less than .20. The change in daytime urine loss between the groups was evaluated using the Wilcoxon rank sum test. We conducted analysis of covariance using propensity score as a covariate to compare the change in daytime urine loss. In a post hoc analysis, we used a chi-square test to compare the proportion of elderly individuals whose daytime urine loss decreased by more than 25%. We also evaluated the effect of USAPV care by calculating a propensity score-adjusted odds ratio for improving urine loss by a logistic regression analysis. The model performance for improving urine loss was evaluated by calculating the concordance index (c-index), which is a generalization of the area under the curve of the receiver operation characteristic curve. P-values less than .05 were considered statistically significant.
3 RESULTS
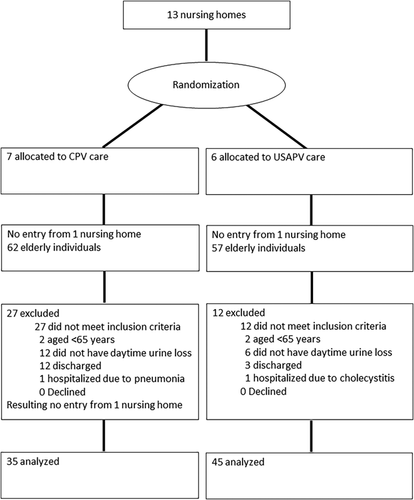
Thirteen nursing homes participated in the study and they were randomly assigned to the CPV (n = 7; four from western part and three from eastern part) and USAPV group (n = 6; three from western part and three from eastern part). Among the 13 randomized nursing homes, no participants were enrolled from two nursing homes (one nursing home each for the CPV and USAPV groups). We excluded 39 of the 119 incontinent residents enrolled because of the following reasons: no daytime urine loss during baseline frequency-volume chart recording (n = 18), discharged within 8 weeks (n = 17), and age younger than 64 years (n = 4), resulting in one nursing home without a CPV group. The statistical power of the enrollees (n = 119) and evaluable subjects (n = 80) was estimated as 90.3% and 72.8%, respectively. The remaining 80 participants (35 from 5 nursing homes for the CPV group and 45 from 5 nursing homes for the USAPV group) underwent a full-term 8-week intervention (Figure 1). Both arms included three western and two eastern facilities. The mean institutional capacity was 95 and 92 residents in the CPV and USAPV groups, respectively (P = .68). All the elderly participants were long-term care recipients. Mean care-needs levels were 3.2 in the CPV and 3.5 in the USAPV groups, respectively (P = .25).
The general characteristics of the participants at the baseline (Table 1) were not statistically different between the groups, except for the EQ-5D score and Barthel index, which were significantly worse in the USAPV group than in the CPV group (P = .024, and P = .006, respectively). As for frequency-volume chart variables, daytime urine volume was equivalent between the groups, whereas daytime urine loss was significantly larger in the USAPV group than in the CPV group (median, 300 g vs 150 g; P = .001). We calculated a propensity score including covariates of age, baseline scores of EQ-5D and Barthel index, daytime urine loss at baseline, and institution. The c-index of our model was 1.000.
| Entire cohort (n = 80) | CPV group (n = 35) | USAPV group (n = 45) | |
|---|---|---|---|
| Age, median (IQR), years | 85 (81-90) | 86 (83-89) | 84 (80-90) |
| Sex, female/male, n | 62/18 | 29/6 | 33/12 |
| Body mass index, median (IQR), kg/m2 | 21.3 (19.0-23.6) | 21.0 (18.3-22.9) | 22.2 (19.2-24.8) |
| Care-needs level, n | |||
| Level 1 | 5 | 3 | 2 |
| Level 2 | 9 | 6 | 3 |
| Level 3 | 26 | 11 | 15 |
| Level 4 | 30 | 10 | 20 |
| Level 5 | 10 | 5 | 5 |
| Charlson comorbidity index, median (IQR) | 3 (1-4) | 3 (1-4) | 2 (1-4) |
| EQ-5D, median (IQR)* | 0.536 (0.359-0.624) | 0.596 (0.485-0.676) | 0.533 (0.204-0.605) |
| MMSE, median (IQR) | 15 (8-20) | 17 (8-22) | 15 (8-18) |
| GDS, median (IQR) | 7 (4-11) | 6 (4-10) | 8 (4-11) |
| Barthel index, median (IQR)* | 40 (25-50) | 45 (35-55) | 30 (20-45) |
| Vitality index, median (IQR) | 6 (5-8) | 6 (5-8) | 6 (5-8) |
| Daytime voided volume at baseline, median (IQR), mL | 550 (400-688) | 550 (340-670) | 550 (415-718) |
| Daytime urine loss at baseline, median (IQR), mL* | 245 (150-409) | 150 (120-270) | 300 (195-470) |
- CPV, conventional prompted voiding; GDS, geriatric depression score; IQR, interquartile range; MMSE, mini-mental scale examination; USAPV, ultrasound-assisted prompted voiding.
- * These factors at baseline were significantly different between the groups (P < .05).
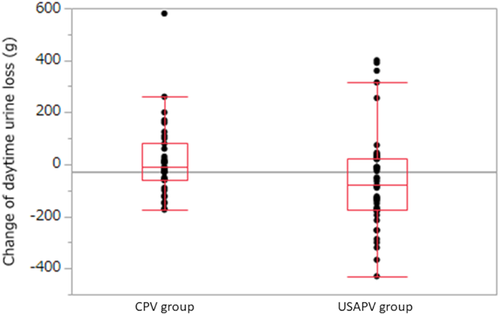
When the parameters were compared at the baseline and at the end of the study (Table 2), the median daytime urine loss in the USAPV group alone significantly decreased after the intervention (P = .008). As for the change in daytime urine loss, which is a primary outcome, the change was significantly larger in the USAPV group (median [IQR], −80.0 [−175 to +24] g) than in the CPV group (median [IQR], −9.0 [−60 to +80] g; crude P = .018 and propensity score-adjusted P = .048, respectively) (Figure 2). Four participants in both groups attained complete dryness (0 g daytime urine loss) at the end of the study. In supplemental analysis, the proportion of elderly individuals whose daytime urine loss decreased by more than 25% was 51% (23/45) in the USAPV group and 26% (9/35) in the CPV group (P = .020).
| CPV group (n = 35) | USAPV group (n = 45) | |||||
|---|---|---|---|---|---|---|
| Baseline | After 8 weeks | P-value | Baseline | After 8 weeks | P-value | |
| Daytime urine loss, median (IQR), g | 150 (120-270) | 180 (100-320) | .90 | 300 (195-470) | 250 (100-438) | .008 |
| Daytime voided volume, median (IQR), mL | 550 (340-670) | 540 (375-700) | .97 | 550 (415-718) | 580 (473-725) | .69 |
| EQ-5D, median (IQR) | 0.596 (0.485-0.676) | 0.596 (0.459-0.670) | .72 | 0.533 (0.204-0.605) | 0.533 (0.200-0.613) | .42 |
| MMSE, median (IQR) | 17 (8-22) | 17 (9-21) | .89 | 15 (8-18) | 14 (9-18) | .36 |
| GDS, median (IQR) | 6 (4-10) | 7 (4-10) | .44 | 8 (4-11) | 8 (5-10) | .19 |
| Barthel index, median (IQR) | 45 (35-55) | 45 (30-51) | .65 | 30 (20-45) | 33 (19-45) | .82 |
| Vitality index, median (IQR) | 6 (5-8) | 6 (5-8) | .68 | 6 (5-8) | 6 (5-8) | .52 |
- CPV, conventional prompted voiding; GDS, geriatric depression score; IQR, interquartile range; MMSE, mini-mental scale examination; USAPV, ultrasound-assisted prompted voiding.
Of the 50 care workers participating in the study (5 each from the facility), 49 (25 of the CPV group and 24 of the USAPV group) completed the SF-12v2 questionnaire and VAS for care burden (Table 3). The median [IQR] age was 36 [30 to 45] years in the CPV group and 42 [32 to 49] years in the USAPV group (P = .22), and the median [IQR] professional career was 149 [113 to 183] months in the CPV group and 141 [88 to 258] months in the USAPV group (P = .94). At baseline, three subscales of SF-12v2 (physical component summary, mental component summary, and role component summary) and VAS score addressing care burden were not statistically different between the groups (P = .92, P = .35, P = .89, and P = .62, respectively). The subscales of SF-12v2 showed no significant changes after the intervention in both groups. The VAS score was almost unchanged in the USAPV group (P = .59), but it significantly worsened after the intervention in the CPV group (P = .010). The change in the VAS score was not significant between the groups (median [IQR], +9 [−1.5 to +25] in the CPV group and 0 [−5 to +14] in the USAPV group; P = .10). No adverse events related to the study protocol were observed in elderly individuals or care workers.
| CPV group | USAPV group | |||||
|---|---|---|---|---|---|---|
| Baseline | After 8 weeks | P-value | Baseline | After 8 weeks | P-value | |
| SF-12v2, median (IQR) | ||||||
| PCS | 50.3 (47.9-53.9) | 49.7 (43.3-57.0) | .68 | 50.4 (35.5-54.5) | 50.4 (44.5-58.1) | .17 |
| MCS | 49.1 (45.2-53.4) | 51.1 (45.1-56.3) | .60 | 52.3 (47.8-54.7) | 49.9 (45.3-52.0) | .15 |
| RCS | 48.4 (35.9-52.9) | 42.2 (39.0-50.1) | .93 | 45.8 (32.0-55.6) | 43.8 (38.6-50.7) | .76 |
| VAS, median (IQR) | 58.0 (49.5-76.0) | 75.0 (63.0-84.0) | .010 | 50.5 (46.5-83.8) | 52.5 (41.5-87.5) | .59 |
- CPV, conventional prompted voiding; IQR, interquartile range; MCS, mental component summary; PCS, physical component summary; QOL, quality of life; RCS, role/social component summary; USAPV, ultrasound-assisted prompted voiding; VAS, visual analog scale.
4 DISCUSSION
The present study demonstrated that USAPV care significantly reduced daytime urine loss of incontinent nursing home residents compared with CPV care. We have previously shown that USAPV care decreases absorbent consumption in incontinent hospitalized adults13 and incontinent elderly living in nursing homes.14 This study is the first randomized controlled trial to confirm the significantly higher efficacy of USAPV than of CPV in managing UI, which is common in the elderly population.
USAPV care could reduce urine loss. Care workers can determine the intravesical urine volume and relative proportion of the individual's optimal bladder capacity at the bedside. They can prompt the elderly individuals to go to the toilet with certainty when the intravesical urine volume reaches the optimal value. Alternatively, the care workers could wait until the next monitoring rather than prompting the elderly individuals to go to the toilet when the intravesical urine volume is still low. This could prevent delayed prompting or non-voiding in the toilet. Given these positive experiences, the elderly individuals and caregivers may be more motivated to void properly in the toilet.
As for the participants’ QOL, cognitive function, mental state, depression, physical function, and level of motivation were assessed using the EQ-5D, MMSE, GDS, Barthel index, and vitality index, respectively. All these indices showed no change after the 8-week intervention in both groups. We previously reported that the vitality index did not change after 12 weeks of USAPV care. Extended intervention may detect changes in these variables, as UI negatively affects multiple aspects of physical, mental, and social health.3-7
A concern with USAPV is the greater burden for care workers because ultrasound monitoring may be too labor-demanding or bothersome. However, none of the QOL domains of SV-12v2 showed significant changes. The VAS score assessing the burden of voiding care was almost unchanged in the USAPV group, but it worsened in the CPV group. We previously reported significant improvement in two subscales of emotional and mental health of SF-36 in care workers practicing USAPV.14 These results consistently indicate that USAPV did not deteriorate the care workers’ QOL. Worsening of care burden VAS scores in the CPV group may be related to the lack of improvement in urine loss among elderly individuals despite excessive tasks to follow the study protocol.
The study limitations include the cluster randomized trial design in a single country with a lower statistical power, and lack of information on time for care, number of prompted voiding, nighttime urine loss, long-term outcomes, and cost-effectiveness. Further studies with a larger number of samples in countries/areas with different socio-cultural backgrounds or focusing on nighttime urine loss, long-term outcomes, and care cost are warranted to support the results. Additional measures to assess work engagement or burnout of care workers are also to be investigated.
In conclusion, USAPV care is efficacious and feasible for managing UI in elderly individuals living in nursing homes. USAPV potentially counteracts the increasing demand for managing UI of dependent elderly individuals.
5 CONCLUSION
Ultrasound-assisted care reduced daytime urine loss of incontinent nursing home residents more greatly than conventional care without increasing caregivers’ care burden. Ultrasound-assisted prompted voiding is efficacious and feasible for managing urinary incontinence in elderly individuals living in nursing homes.
ACKNOWLEDGMENTS
We sincerely thank all the participants and care staff for their co-operation in this study. This study was completely supported financially by grants from the Japanese Society of Geriatric Urology (Tokyo, Japan). The funder had no role in the study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit the manuscript for publication.
ETHICAL STATEMENT
This randomized open-label clinical trial was approved by the institutional review board of the University of Tokyo (No. 10667) and registered in the UMIN Clinical Trials Registry (ID No. UMIN000017963).
AUTHORS' CONTRIBUTIONS
YH designed the study and wrote the initial draft of the manuscript. MS and HM equally contributed to acquisition, analysis and interpretation of data, and assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
CONFLICTS OF INTEREST
None.