Low-field MRI: A report on the 2022 ISMRM workshop
Abstract
In March 2022, the first ISMRM Workshop on Low-Field MRI was held virtually. The goals of this workshop were to discuss recent low field MRI technology including hardware and software developments, novel methodology, new contrast mechanisms, as well as the clinical translation and dissemination of these systems. The virtual Workshop was attended by 368 registrants from 24 countries, and included 34 invited talks, 100 abstract presentations, 2 panel discussions, and 2 live scanner demonstrations. Here, we report on the scientific content of the Workshop and identify the key themes that emerged. The subject matter of the Workshop reflected the ongoing developments of low-field MRI as an accessible imaging modality that may expand the usage of MRI through cost reduction, portability, and ease of installation. Many talks in this Workshop addressed the use of computational power, efficient acquisitions, and contemporary hardware to overcome the SNR limitations associated with low field strength. Participants discussed the selection of appropriate clinical applications that leverage the unique capabilities of low-field MRI within traditional radiology practices, other point-of-care settings, and the broader community. The notion of “image quality” versus “information content” was also discussed, as images from low-field portable systems that are purpose-built for clinical decision-making may not replicate the current standard of clinical imaging. Speakers also described technical challenges and infrastructure challenges related to portability and widespread dissemination, and speculated about future directions for the field to improve the technology and establish clinical value.
1 INTRODUCTION
There is a growing ISMRM community interested in developing and applying low-field MRI technology. In March 2022, the first ISMRM Workshop on Low-Field MRI was held virtually (with low field defined as <1.5T for the Workshop): https://www.ismrm.org/workshops/2022/LowField/. The goals of the Workshop were to discuss recent low-field MRI hardware and software developments, to discuss clinical applications of low-field MRI, to describe contrast mechanisms at low field, and to explore methods for disseminating this more accessible MRI technology. The program included invited talks, panel discussions, live demonstrations of prototype low-field MRI systems, and proffered papers, as well as vendor participation.
The revitalized interest in low-field MRI by researchers, clinicians, and vendors has primarily been driven by accessibility, portability, and new clinical applications. Lower field affords flexibility in magnet design, enabling wider patient bores, unconventional geometries, point-of-care imaging, and even portable systems. Such portable low-field MRI systems enable clinicians to answer certain important clinical questions at the bedside, and enable MRI to reach new populations; system portability opens a new realm of possibilities for how and where MRI is used and by whom. Lower field MRI systems are inherently lower cost compared to high-field systems, although the cost savings varies depending on the exact system design and specifications, and the cost to the consumer is more than the cost of the equipment alone. Moreover, contemporary techniques for low-field MRI compensate for the lower fundamental SNR with more efficient acquisitions and with modern image reconstruction and processing strategies, which are inexpensive to implement and deploy. There have been several recent review articles and editorials responding to this growing interest,1-9 and there are newly developed commercial systems with United States Food and Drug Administration (FDA) approval that have benefitted from recent advances in both software and hardware.
The purpose of this report is to summarize the scientific content and discussion from the ISMRM Workshop on Low-Field MRI. The Workshop covered research spanning two orders of magnitude in field strength from 6.5 mT to 0.75T, including several different system designs and target clinical applications. The Workshop also sought to describe the current state of the field and establish the community's vision and goals moving forward, as outlined in this report.
2 WORKSHOP DETAILS, DEMOGRAPHICS, AND CONTENT
The virtual Workshop was attended by 368 registrants from 24 countries, including several regional watch parties. Table S1 summarizes the demographics of the registrants. There were 100 abstract presentations, and seven companies provided vendor sponsorship.
Table S2 provides the agenda from the ISMRM Workshop on Low-Field MRI. The Workshop recording is available for all ISMRM members at https://www.ismrm.org/workshops/2022/LowField/, or can be purchased by non-members. The Workshop content reflected ongoing developments in low-field MRI, with field strengths spanning two orders of magnitude from 6.5 mT to 0.75T. A range of system designs were described, including FDA 510(k) cleared clinical scanners; prototype systems; systems designed using superconducting magnets, resistive magnets, and Halbach arrays; systems using alternative spatial encoding strategies; single-sided systems; and field cycling systems. Moreover, a diverse range of applications were described including portable MRI, MRI-guided interventions, neuroimaging, cardiac imaging, abdominal imaging, breast imaging, musculoskeletal imaging, body composition assessment, real-time imaging, neonatal imaging, ex-vivo studies, quantitative imaging, and implant imaging.
2.1 Scientific sessions
The Opening Plenary session (Session 1) focused on the current state of the field. Jürgen Hennig provided historical context on field strength,1 starting with the commercialization of 1.5T MRI in 1983, and the subsequent relegation of “low-field” systems to permanent magnet designs which were inherently limited by their high weight and relatively low performance.7 He emphasized that new low-field MRI system designs perform well for routine imaging, and additionally offer unique opportunities as well as unique challenges. He encouraged careful consideration of the specific trade-offs between cost and performance for each application.
Matthew Rosen provided an insightful lecture on his 20 years of working on a custom biplanar 6.5 mT electromagnet MRI technology and on a more recent commercial 64 mT system (Swoop, Hyperfine Inc, Guilford CT). His approach focused on the combination of physics and computation to address the SNR challenges, specifically through coil design,10 noise reduction, high efficiency data sampling,11 and deep learning reconstruction. He provided examples of AUTOMAP image reconstruction,12, 13 MR fingerprinting, portable neuroimaging,14-16 neuronal current MRI,17 and the use of low-field MRI contrast agents.18
Johnes Obungoloch provided a valuable perspective on the deployment of low-field MRI technology in Africa where there are fewer than three MRI devices available in most countries.19 To increase access, he suggested developing systems, such as Halbach arrays,20 that can be built, installed, and maintained with local expertise; establishing local manufacturing capacity and training; developing systems that are inexpensive and flexible; understanding local infrastructure constraints such as low power requirements and power instability; cultivating multi-national multi-disciplinary teams; and advocating to local governments for support.2, 21, 22
Session 2 focused on the dissemination of low-field MRI technology. Larry Wald described the cost versus performance trade-off when designing low-field MRI systems.23 He emphasized that cost is more than just hardware and computational resources, but also includes development costs, maintenance costs, and infrastructure costs. Sairam Geethanath provided an overview of autonomous scanning, including automated acquisitions, automated quality assessment, and the implications of automation to reduce barriers to access by augmenting local expertise (e.g., technologist, nurse, physician, or radiologist).24 Francis Shen described the ethical, legal and social implications of portable MRI systems that offer a new opportunity for field-based research when MRI is used more broadly in community settings outside of major hospitals.25, 26 Jana Delfino provided an overview of the FDA's perspective on low-field MRI. She emphasized that the FDA is supportive of informed access to this technology for appropriate use, and that implant safety and labeling warrants further investigation.
Session 3 provided representative clinical images from a variety of low-field MRI systems. Specifically, Vikas Gulani described abdominal imaging on a commercial 0.55T system (MAGNETOM Free.Max, Siemens Healthcare, Erlangen, Germany),27 Ed Wu provided neuroimaging examples on a custom 0.055T system,28 and W. Patricia Bandettini showcased cardiac imaging using a prototype 0.55T scanner (modified MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany).29, 30 In each case, examples of high-quality images were contrasted against examples where additional optimization is still warranted.
Session 4 focused on acquisition strategies for low-field MRI. Craig Meyer discussed the opportunities for deploying highly efficient data sampling methods and the challenges of concomitant field artifacts. He focused on spiral imaging, EPI, and bSSFP for high SNR-efficiency, which leverage the longer T2* and more homogenous B0 available using a contemporary superconducting 0.55T system, compared to ≥1.5T systems. He demonstrated applications in the heart, lung, brain, and vocal tract.31, 32 William Grissom described sequences in a world without specific absorption rate (SAR) constraints, which included examples of high B1 field amplitudes (up to an order of magnitude higher than at 1.5T); full 180° refocusing pulses in turbo spin echo readouts33; high-amplitude spin locking pulses for efficient T1ρ imaging; Overhauser effect MRI; imaging with intrinsically inhomogeneous B0 designs using wide bandwidth pulses34; and spatial encoding using RF gradients.35 Mark Griswold made an argument for MR fingerprinting at low field, which allows imaging in transient magnetization states, longer data collection times during a period of relaxation and/or diffusion processes, and pattern matching as a nonlinear filter to reduce sensitivity to low SNR. He provided examples from field strengths ranging from 6.5 mT to 0.55T.36-40
Session 5 described hardware for low-field MRI. Charlotte Sappo provided an overview of coil design for low-field MRI. She focused on simple solenoid designs, optimization of wire patterns, and separate transmit/receive coils.41, 42 She emphasized the importance of harmonizing system design with intended applications. Thomas O'Reilly provided an overview of flexible Halbach array magnet design.43, 44 He described optimization tools and analytical methods for designing B0 and shim arrays, and provided practical guidance to implement these designs.43, 45 Lukas Winter described the OSI2-ONE open-source MRI system project (https://gitlab.com/osii-one). The goal of this project is to develop an open-source MRI system, including hardware and software, that combines existing open-source projects into a single reproducible system. This 30 cm Halbach array system (48mT) is affordable (20–30 k euros) and low weight (100 kg), and it has been reproduced by others. Clarissa Cooley discussed the hardware requirements for portable MRI.34 She described “downsizing” using anatomy-specific scanners, reducing system weight, modifying spatial encoding strategies, safety considerations, eliminating cryogen usage and power requirements, and mitigating electromagnetic interference.28, 46
Session 7 described image contrast at low field. José Marques provided a detailed overview of how physical properties and contrast mechanisms vary across field strengths from 0T to 7T.5 In particular, he highlighted the field-dependence of dipole–dipole interactions, paramagnetic interactions, and macromolecular exchange effects.47, 48 He emphasized that each field is unique, and each contrast is unique at each field; meaning that, depending on the field strength selected, different dynamics are probed. Nathan Williamson described his work on ex vivo hydrophysiology in which he used a 0.32T single sided NMR MOUSE (Magritek, Aachen, Germany) to probe water diffusion49 and exchange across membranes at short timescales in live spine tissue. His results indicate that the relationship between water exchange and tissue viability can be measured using NMR. Lionel Broche provided an overview of field cycling MRI, a technique that has recently moved from benchtop to in vivo imaging.50, 51 He described the importance of T1 dispersion across field strengths (0.2 mT to 0.2T for his work), which could be related to the confinement of water as illustrated in cancer and stroke patients. T1 signatures obtained with field cycling MRI could be used as biomarkers and/or exploratory tools to identify relevant field strengths for specific applications.
Session 11 focused on point-of-care MRI. Charles Dumoulin discussed MRI in the NICU environment, and barriers to clinical adoption.52-54 He outlined the requirements for his approach to NICU imaging: namely, a general-purpose MRI system customized to imaging of premature babies. Commercial dedicated neonatal systems are available with field strengths ranging from 1T to 3T. Low field may offer the advantages of improved safety, ease of installation, and low acoustic noise,55 but he cautioned that compromises in image SNR may not satisfy key clinical requirements for neonatal imaging. Shaoying Huang outlined the international need for point-of-care systems with a small footprint, light weight, low power consumption, and low cost. She described the use of MagTetris for fast simulations of magnetic fields.56, 57 Mathieu Sarracanie described fast acquisitions targeted for point-of-care imaging. He emphasized that fast acquisitions must be paired with other methods to mitigate noise, and that it is important to be mindful of hardware to enable optimal, advanced acquisitions. He also showed examples of quantitative imaging and non-Cartesian imaging performed at 0.1T.38, 58-60 Zheng Xu described work with a 2.1 MHz scanner (49 mT) for stroke imaging, which included a new permanent magnet design, active electromagnetic interference (EMI) cancelation, and excellent GRE and bSSFP image quality.61
Session 13 focused on image reconstruction and processing methods for low-field MRI. Rizwan Ahmad provided an overview of compressed sensing at low fields. He emphasized cardiac imaging with 0.35T1, 62 and 0.55T29, 63, 64 superconducting whole body scanners and demonstrated excellent image quality. Patricia Johnson described the role of AI for low-field MRI. She focused on denoising, accelerated imaging, image quality transfer methods designed to impart low-field images with some of the appearance of higher field images, and transfer learning methods in which machine learning models developed at higher fields are fine-tuned or retrained to apply to lower fields.65 Matt Bernstein described concomitant fields, which are an unwanted consequence of Maxwell's equations that can lead to image artifacts that become more significant as field strength decreases (and as gradient amplitude increases). He summarized several mitigation strategies including waveform modification, symmetrizing, reshaping, quadratic nulling, and correction via image reconstruction methods.66-68 Brian Hargreaves provided an overview of imaging artifacts near metallic implants.69 These artifacts manifest as signal displacement, signal pileup, signal loss, and distortion, which are mainly corrected by multispectral imaging. The benefits of using low field for imaging near metallic implants are artifact reduction, shorter scan times for multispectral imaging, and the availability of high bandwidth pulses that allow excitation of a broad range of frequencies to avoid signal loss.70, 71
Session 14 described how low-field MRI may fill a clinical niche. Scott Reeder used the lens of value (defined as quality/cost)72 to examine the potential clinical role of low-field imaging. He indicated that ongoing increases in clinical volume may render the purchase of high-field systems unsustainable. He encouraged the Workshop participants to consider the clinical questions at hand, for both niche applications and “standard” applications where higher field MRI exceeds minimum diagnostic requirements. Hersh Chandarana described unmet needs in lung imaging. He emphasized that CT provides excellent anatomical detail, but lacks functional information and is limited for longitudinal monitoring. Superconducting low-field MRI systems (e.g., 0.55T) that offer improved field homogeneity may yield significant value for combined structural and functional examinations.73-76 Yingli Yang described MRI-guided radiotherapy using the 0.35T MRI/linear accelerator (MRIdian, ViewRay, Denver, CO), and especially the added value of MRI compared to other modalities.77, 78 MRI provides improved soft-tissue contrast, which is valuable for real-time inter-fraction imaging, planning (reduced margins) and setup based on tumor position (instead of using bony landmarks or skin contours).79 Frank Shellock described implant safety at lower field, from 100 mT to 1.5T, including the impact of field direction (horizontal or vertical fields) on force/torque, and the dependence of device heating on a combination of device length, RF wavelength, and E-field direction.
The Closing Plenary session (Session 16) provided future perspectives. Kevin Sheth talked about his extensive clinical experience in more than 700 patients using a point-of-care 64 mT MRI system (Swoop, Hyperfine Inc, Guilford CT) in an ICU setting.14-16, 80, 81 He has demonstrated the utility of portable low-field MRI to make several basic, but clinically relevant, diagnoses at the bedside, such as midline shift or mass effect, and to monitor the progression of patients over time. These example applications of point-of-care imaging would be challenging with a traditional non-portable MRI system. Some images were compared to 3T to demonstrate diagnostic confidence. Adrienne Campbell-Washburn provided a closing summary of the Workshop. She described unique clinical applications that are enabled by low field. Examples included portable imaging, MRI-guided procedures, MR of patients with implants, and imaging anatomy with large magnetic susceptibility gradients (e.g., lung and bowel).31 She also described how low-field MRI may aid clinical adoption of some existing applications by increasing scanner accessibility, bringing MRI to different point-of-care settings, and changing the workflow in Radiology enterprises. Finally, she highlighted the opportunities to develop new technology including hardware, software, and tools to facilitate dissemination.
2.2 Abstract sessions
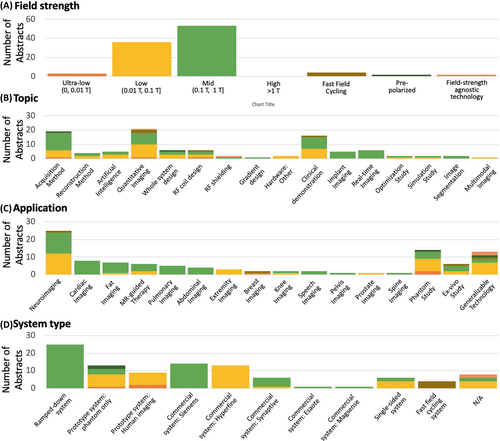
One hundred abstracts were presented in live breakout sessions, and 18 of these were also selected for short oral presentations (Sessions 6 and 12). Abstracts and recorded presentations are available here: https://www.ismrm.org/workshops/2022/LowField/posters.htm. The contents of the abstracts, divided into field strength, system type, topic, and application, are summarized in Figure 1. Twenty-three23 unique system configurations were described in the abstracts. Approximately 62% of abstracts used prototype systems (used for human, animal, or phantom imaging), and 38% used commercial systems approved for clinical use. Thirty-six percent (36%) of abstracts used a system with field strength range 0.01–0.1T, 53% used 0.1–1T, and the remaining 11% were ≤0.01T systems, fast-field cycling systems, prepolarizer systems, or generalizable technology across field strengths.
2.3 Panel discussions
The workshop included two panel discussions and the “Key Themes” section below elaborates on the topics of these two panel discussions. The first panel (Session 8) focused on the tradeoffs between cost, performance, and applications. This panel conversation centered around clinical paradigms for which low-field MRI is attractive. Such paradigms range from offloading patient volume from backlogged conventional ≥1.5T scanners in existing Radiology enterprises to answering targeted questions at the bedside to performing imaging-based monitoring of subjects where they live or work. It was noted that different levels of image quality may be required for different use cases, and that our field's long-standing bias toward high-SNR images may not always serve us well. Additionally, panelists described the power of harnessing the different contrast available at widely-varying field strengths, the potential contribution of low-field MRI to multimodality imaging systems, and the documented value of low-field MRI for image-guided therapies. The potential role of accessible low-field systems in facilitating the collection of longitudinal information on subjects' health over time was also noted.
The second panel discussion (Session 17), led by the Workshop organizing committee, focused on future directions for low-field MRI. In particular, the panel summarized ongoing community initiatives, noted opportunities for collaborative research, cited the need for open-source data sets, and encouraged engagement of other stakeholders, especially physician groups. One outcome of this discussion was the formation of a new ISMRM Study Group (https://groups.ismrm.org/low-field-mri/).
2.4 Live demonstrations
The National Heart, Lung, and Blood Institute provided a live demonstration (Session 9) of invasive heart catheterization in a swine model using a ramped-down prototype 0.55T MRI system (MAGNETOM Aera, Siemens Healthcare, Erlangen).31 Robert Lederman and Adrienne Campbell-Washburn narrated the demonstration, and catheterization was performed by Christopher Bruce with Amanda Potersnak and Rajiv Ramasawmy in the control room. This demonstration included a tour of the combined X-ray/MRI catheterization suite, a presentation of the catheters, guidewires, and other equipment used during procedures, and a live right- and left-heart catheterization performed in the swine model using real-time bSSFP image guidance with high tissue contrast for device navigation, all within 30 min. Metallic devices (guidewire and stainless-steel braided pigtail catheter), which have been shown to generate negligible heating at 0.55T,31 were used during the procedures.
Leiden University provided a live demonstration (Session 10) of their 50 mT home-built MRI system, which they are using for healthy volunteer imaging.43 Andrew Webb and Chloe Najac performed the hands-on demonstration and Thomas O'Reilly answered questions in real-time in the chat. They showed their cylindrical 50 mT Halbach array magnet design, 3D printed gradient and RF coils, off-the-shelf electronics, a home-built console based on a Red Pitaya platform, and configurable shim trays. They emphasized the low cost of the system components, and the system modularity that simplifies service and repair. They demonstrated live scanning in a phantom, generating negligible acoustic noise, and their home-built scanning software. In addition, they showed previously acquired in vivo images and discussed opportunities for high B1 sequences, long echo trains, and imaging of implants.
2.5 Vendor session
Four Workshop Tier IV sponsors (Synaptive Medical Inc, Siemens Healthineers, Cook Medical, and Aspect Imaging) provided live presentations, one additional Tier III vendor sponsor (Hyperfine Inc) provided a pre-recorded presentation (Session 15). Additionally, representatives from a Tier II sponsor (Fujifilm) were present at the Workshop. Vendor support of this emerging community is crucial in creating strong collaborations and facilitating clinical translation.
3 KEY THEMES
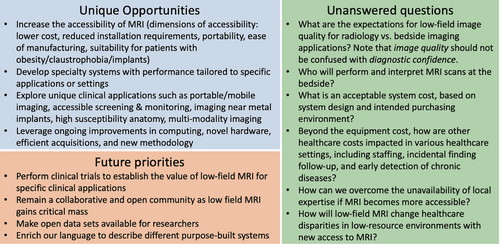
The Workshop provided ample opportunity for audience discussion, during which a few key themes emerged, particularly during the panel discussions and in the very active chat window. We have summarized these themes below, and Figure 2 highlights some unique opportunities, unanswered questions, and future priorities in low-field MRI, as discussed during the Workshop.
3.1 Selection of appropriate clinical applications
The selection of appropriate clinical questions that can be confidently answered with low-field MRI was discussed numerous times. In general, low-field MRI may expand the clinical use of MRI both within traditional settings (e.g., hospital and outpatient Radiology enterprises), as well as to bedside and point-of-care settings. Ultrasound imaging offers a useful analogy: ultrasound systems are manufactured with varying resolutions, portability, and cost, and are used to answer different clinical questions through all stages of patient care. Low-field MRI may transform MRI into a similar imaging paradigm, in other words, different systems with different image quality for different purposes. Importantly, low-field MRI systems are not aimed at replacing, but rather at complementing, conventional ≥1.5T clinical MRI systems.
So far, we have referred to any field strength <1.5T as “low field”; however, it is apparent that there are different low-field imaging regimes that should be treated differently, with their own unique challenges and opportunities. As of yet, there is no consensus on low-field strength nomenclature, and for this discussion, we use the following definitions: ultra-low-field [0, 0.01T], low-field (0.01, 0.1T], and mid-field (0.1T, 1T].
Mid-field systems can, quite successfully, achieve diagnostic image quality that is completely adequate for many applications. These systems are sufficient to answer many clinical questions where 1.5T or 3T image quality exceeds minimum diagnostic requirements, or where modest additional time expenditures to boost image quality are acceptable. For example, mid-field systems have been used successfully to evaluate patients presenting with headaches or with suspected skeletal fractures, and could be used for imaging hemorrhage or ischemia, or for evaluation of cardiac anatomy. Therefore, these mid-field systems could be deployed in harmony with 1.5T and 3T systems to address an institution's specific clinical volume.82 Mid-field system may be acquired at a lower cost and then can allow conventional ≥1.5T clinical MRI systems to be used when they are necessary, enabling departments to complete more MRI exams at an overall lower cost. Alternatively, mid-field systems could facilitate deployment of MRI to good effect for general purpose radiology imaging in lower-resource regions and outpatient settings where 1.5T or 3T systems are scarce, as long as suitable diagnostic information can be gleaned.83 Additionally, these systems offer advantages in niche applications, such as imaging high-susceptibility anatomy (e.g., lung and bowel), imaging near metallic implanted devices, or performing MRI-guided interventions.70 Furthermore, the lower cost of these systems may encourage the adoption of applications that are difficult to justify, economically, with current high field system – for example, cardiac imaging may be achievable at mid-field, and is currently underutilized at ≥1.5T due to cost and complexity, despite clinical evidence of its diagnostic and prognostic value.1
On the other hand, low- and ultra-low-field systems require a different approach, and different expectations. The goal for these systems is to obtain maximum clinically useful information from the available low signal, and to perhaps to unveil new information via new endogenous contrasts. Such systems tend to be portable, and they can therefore be brought directly to the patient, shifting the traditional dynamic in which patients are brought to cross-sectional imaging devices. Point-of-care settings of particular interest include the bedside, the ambulance, mobile MRI brought to a patient's home, mobile stroke units, and the battlefield. The portability of low- and ultra-low-field systems makes them well suited to answer tractable and actionable macroscale questions – such as ventricle size, presence of hemorrhage, cerebral edema, and midline shift – in acute care environments.84 Additionally, these systems may potentially offer general imaging where it was unavailable before in lower-resource and outpatient settings, with much more widespread dissemination and adoption anticipated.71, 85
Across all low-field strengths and system designs, imaging for screening, normative imaging, treatment monitoring, and serial follow-up imaging in patients are applications of great interest. Examples include body composition assessment, lung cancer screening, and childhood brain development. These types of exams are not practical using backlogged systems located in Radiology, but low-field systems promise to reposition MRI as a frontline assessment, rather than a modality of last resort.
Low-field MRI offers substantial flexibility in system design, and therefore the unique capabilities of each system configuration, and the resulting applications, should be explored in parallel to “standard” applications. Conversely, a low-field system could be purpose-built for the intended application and setting, which is not practical with current high field MRI. This could include, for example, body-part specific systems, large-bore systems for imaging severely obese and claustrophobic patients, and interventional systems.86
Additional research and dedicated clinical trials are required to fully explore the plethora of clinical applications, but in the long term, selecting the appropriate patients and/or exams is critical for widespread adoption and acceptance of low-field MRI.
3.2 Image quality
The concept of “image quality” when assessing low-field MRI was discussed at length. In general, image quality should not be confused with information content, diagnostic accuracy, and diagnostic certainty, which are the important metrics for clinical utility. Of course, SNR is intrinsically lower due to reduced polarization and reduced Larmor frequency at low field; and while there are many methods to improve SNR (e.g., hardware optimization, noise canceling, efficient acquisitions, advanced reconstruction, AI), this should not be the only goal.
The aspiration to attain SNR and image contrast similar to 1.5T and 3T is derived from bias toward these familiar looking images by radiologists, surgeons, and others who use MRI clinically. Familiar image appearance is valuable to accelerate clinical adoption, but often not necessary to answer clinical questions. A specific image appearance could be attained using synthetic contrast from parametric mapping across field strengths. However, it is unclear whether the focus should be on matching 1.5T and 3T image appearance, or instead embracing different endogenous contrasts and image quality offered at low field for suitable applications.
Mid-field “value” systems (0.1–1T) have been providing accurate diagnosis worldwide for decades, including body-part specific systems and open bore geometries. Historically, commercial low-field systems have employed additional hardware compromises (e.g., lower gradient performance, heavy permanent magnets with lower field homogeneity, or few receive channels). Modern mid-field systems have improved on these system specifications to yield faster, higher resolution, and higher SNR imaging, with minimal cost increase. Clinicians can “read through” lower SNR to some extent, and one might hypothesize that the adoption of contemporary mid-field MRI systems could resemble that of low dose CT.
Low-field (0.01–0.1T) and ultra–low-field (<0.01T) MR images, on the other hand, should not be expected to resemble those of standard clinical systems, especially since different clinical questions are addressed with these systems. These low-field systems are purpose-built to support clinical decision making in scenarios where high-field MRI is impractical, unobtainable, or otherwise ill-suited.
3.3 System costs
Low-field MRI systems are often touted as low-cost systems, but the exact system cost in-practice depends on several factors, including magnet design (magnet type and cryogenic requirements), other hardware specifications (RF systems, gradient performance, shim coils, array coils, spatial encoding methods, console), siting requirements, and computational requirements. Additionally, the acceptable cost will depend on the purchaser, the setting, reimbursement, patient throughput, and the intended use-case. Many of the systems presented at the workshop were prototype systems that are not marketed.
In 2022, as a rule-of-thumb, for clinical systems the breakdown in component costs is 40% magnet, 30% gradient coils/amplifiers, and 25% radiofrequency/receivers.23 Top-of-the-line clinical systems ≥1.5T cost millions of dollars, maintenance contracts run in the tens of thousands of dollars per year, and the construction and shielding requirements can be conservatively estimated at $100 k. Whereas, if one moves to a “lower end” 1.5T system, then the overall purchasing costs might be reduced by up to 50%. However, these general rules-of-thumb do not apply for contemporary low-field MRI systems.
An identical superconducting magnet design operating at a mid-field, instead of 1.5T, is inherently less expensive because less material is required and siting requirements are reduced (lower weight, less helium, less shielding, and smaller footprint). Currently marketed high-performance mid-field systems can be expected to cost approximately one-third to one-half of a top-of-the-line 1.5T system. Fixed permanent magnet-based systems operating at 0.1–0.2T are approximately the same cost, but typically do not require as extensive shielding.
Rare earth arrays magnets or resistive magnets (typically <0.5T) do not require cryogenics and are common in low- and ultra-low-field system designs. These magnet designs can reduce expense more dramatically, for example, by an order of magnitude compared to 1.5T.23 For example, a home-built 50 mT Halbach array system has been reported to cost <€15 000 for only the material and production costs, with almost no siting requirements.20 Currently marketed portable point-of-care units cost more than this, but they require fewer financial resources in terms of siting and maintenance.
The impact on healthcare costs, meanwhile, extends beyond the hardware itself. If MRI becomes more accessible, other costs, such as the costs of staffing and maintenance, must also be considered. Additional costs, or cost savings, associated with chronic disease monitoring and management of incidental findings will certainly have to be studied extensively in the future. Downstream costs may be reduced if accurate, earlier diagnosis can be enabled by more accessible MRI.
3.4 Dissemination challenges
The affordability and portability of low-field MRI are as much a component of the innovation as the engineering itself, and dissemination was a topic that was discussed at length during the Workshop. Portable MRI systems are designed to address some physical barriers to MRI access, including availability of equipment, power stability in some settings, and travel requirements to reach MRI equipment.
However, availability of local expertise is another barrier to access, which, in many ways, is harder to overcome. In some cases, the cost of travel for experts to perform system installation, maintenance, and training may be prohibitive. Therefore, systems that are easy to install and maintain with local expertise are appealing, as is leveraging local manufacturing capabilities to produce system components. Open-source initiatives, such as the OSI2-ONE project, are important for this purpose.87, 88 Automation of system operation, debugging, and interpretation, or remote support, are also important to complement available expertise.
Bringing MRI systems to the bedside raises important questions such as “Who should be performing the exam?”, “Who should be interpreting images?”, “What is a reasonable safety protocol?”, and “What is the certainty/uncertainty of an incidental finding, and how is that communicated?”.89, 90 Point-of-care ultrasound exams are often performed and read by local physicians, not radiologists. These questions will need to be addressed within individual healthcare systems.
The societal implications of widespread MRI availability are also widely unexplored. For example, accessible MRI may change the healthcare disparities in low-resource environments with new access to MRI, whereby access to some MRI is better than none; but access to only low-field MRI may disadvantage these populations. Looking further into the future, the societal impact of possible direct-to-consumer MRI requires more consideration. Additionally, the pathway to regulatory approval is unclear for many current home-built low-field systems.
3.5 Technology development
Substantial opportunities remain to further improve low-field MRI technology, including both software and hardware developments. Of course, the same is true for higher fields, and ongoing developments are expected to benefit a range of field strengths. The theme of improved imaging methods threaded through several sessions at the Workshop. Leveraging inexpensive computational power to recover image quality was a commonly proposed solution to low SNR. Many flavors are envisaged, including more traditional image reconstruction and denoising, as well as methods based on transfer learning from datasets acquired in cohorts studied at both high and low field. Beyond improving individual images, computational power can also be leveraged to increase information content, or to take advantage of mutual information present in images acquired serially over time, which may have benefits to outpatient imaging including screening and therapeutic monitoring. New methods to compensate for artifacts that are specific to each system design and setting, for example eddy currents, concomitant fields, and electromagnetic interference, are critical to the success of low-field MRI systems. Another advantage of low-field MRI is the ease of incorporating multi-modal imaging (e.g., EEG, PET, NIRS, or neuronal currents). This area remains relatively unexplored and offers significant promise.
3.6 Next steps
The modern era of low-field MRI is still relatively new, meaning that many questions of interest remain unanswered. As the low-field MRI community gains critical mass and low-field systems become more widely available, there will be expanded opportunities for research and clinical trials that establish the value of low-field MRI for a variety of applications.
As the low-field MRI community grows within ISMRM, there are several initiatives that we plan to undertake. A new ISMRM Study Group on Low-Field MRI has been formed as a result of the Workshop. We anticipate that our community will continue to develop novel technology, and carefully consider target applications. We also plan to increase the availability of low-field MRI datasets to facilitate software development.91 Over time, we hope for more engagement from radiologists and non-imaging clinicians who may become the eventual users of low-field MRI.
In the long term, we will need to enrich our language and develop specific nomenclature to clearly describe low-field systems in a way that encompasses the diversity of configurations and methods. To date, the low-field MRI community has been open and collaborative, and we aim to maintain this ethos to realize the goal of making MRI accessible. To achieve this, we will continue to embrace open-source hardware and software, open dialogue, and prioritizing dissemination.
4 CONCLUSIONS
Low-field MRI offers many exciting opportunities for the ISMRM community, and early studies have shown significant promise for low-field MRI to disrupt the current medical imaging ecosystem. There are numerous remaining challenges, which will be addressed under the stewardship of this community. This ISMRM Workshop offered an early opportunity to discuss the ongoing research in low-field MRI, and to foster collaborations and dialogue to enhance these technologies.
ACKNOWLEDGMENTS
The authors of this paper are the Low-Field MRI Workshop organizers, plenary speakers, and panelists. We are grateful to the ISMRM staff for their assistance in organizing and hosting the Workshop. We thank the Workshop speakers and moderators for their contributions and the attendees for their active participation. We also thank ISMRM's corporate members, and specifically Aspect Imaging, Cook Advanced Technologies, Siemens Healthcare, Synaptive Medical, Hyperfine, and Fujifilm for their sponsorship.
CONFLICT OF INTEREST STATEMENT
Certain commercial equipment, institutions, or materials are identified in this paper in order to specify the experimental procedure adequately. Such identification is not intended to imply recommendation or endorsement by NIST, nor is it intended to imply that the materials or equipment identified are necessarily the best available for the purpose. Matthew S. Rosen is a founder and equity holder of Hyperfine, Inc., Kevin N. Sheth and Joel M. Stein receive sponsorship from Hyperfine, and Krishna S. Nayak receives funding from Siemens Healthcare. Adrienne E. Campbell-Washburn is an investigator on a research agreement with Siemens Healthcare. Daniel K. Sodickson oversees departmental research agreements with Siemens Healthcare and Hyperfine.