Cardiovascular diseases after liver transplantation—a still emerging and unsolved problem!
See Article on Page 889
Abbreviations
-
- CV
-
- cardiovascular
-
- CVD
-
- cardiovascular disease
-
- EF
-
- ejection fraction
-
- LT
-
- liver transplantation
-
- MS
-
- metabolic syndrome
-
- NAFLD
-
- nonalcoholic fatty liver disease
-
- NASH
-
- nonalcoholic steatohepatitis
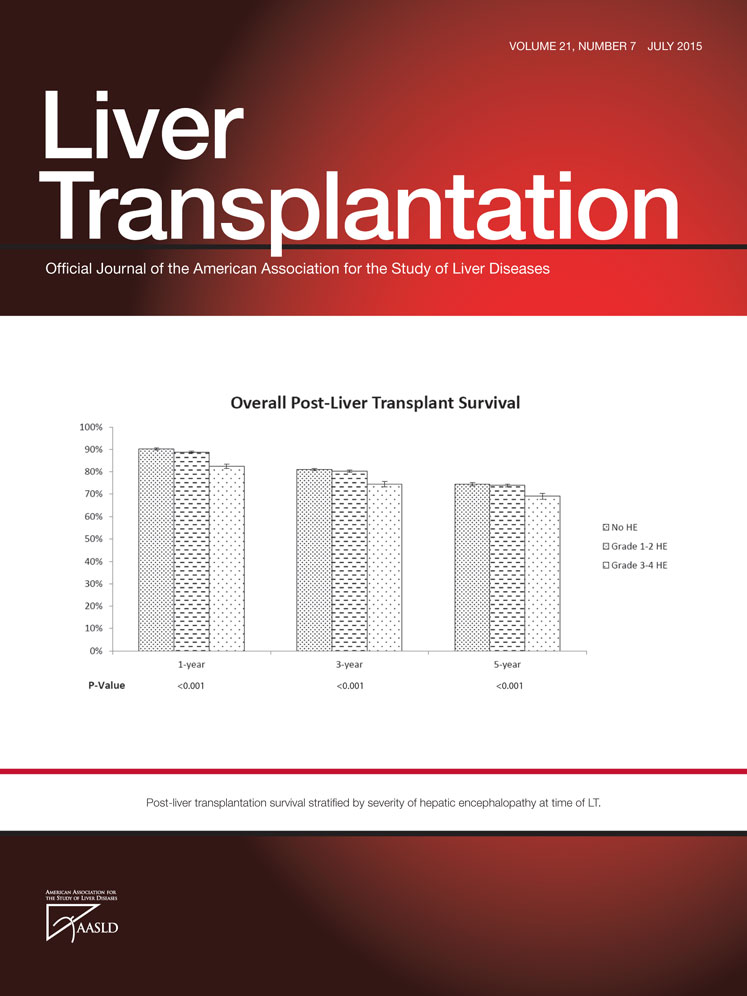
The outcome of adult liver transplantation (LT) recipients has improved incrementally over the last 4 decades with patient survival rates of approximately 90% at 1 year and 70%-80% at 5 to 10 years. The greatest progress has been mainly achieved in the early postoperative period because of improved selection criteria, advances in surgical techniques, and improvements in immunosuppressive and anti-infective drug therapies. The survival rates beyond 1 year, however, have remained relatively stagnant during the same time period. This fact as well as the growing number of long-term survivors has increased the importance of understanding the underlying mechanisms and risk factors for intermediate and late post-LT complications and death attributed to medical complications. Beside de novo malignancies, cardiovascular diseases (CVDs) have emerged as one the leading causes of non-graft-related morbidity and mortality in LT recipients, accounting for 12%-16% of deaths.1
Several studies have shown that LT recipients have a significantly increased risk of cardiovascular (CV) events and deaths compared to an age- and sex-matched general population. This elevated CVD rate ranges from 9% at 5 years to up to 25% at 10 years. 2 The high prevalence of metabolic syndrome (MS) and its clinical features, in particular insulin-resistant (type 2) diabetes, obesity (body mass index >30 kg/m2), dyslipidemia, and arterial hypertension, either alone or in combination, are the main contributors to the high risk of CVD in the post-LT period. It has been shown that patients with post-LT MS are approximately 4 times more likely to have a CV event than recipients without MS. In addition, recent studies have reported a significantly higher post-LT prevalence of MS ranging from 40% to 58% at 1 year compared to the general population.3, 4 Interestingly, the higher incidence of MS in LT recipients is not only seen in patients transplanted for nonalcoholic fatty liver disease (NAFLD) but also in patients transplanted for other indications.
NAFLD, the hepatic manifestation of MS, is the leading cause of abnormal liver function tests in the Western world. Fatty liver disease leads to a spectrum of liver diseases ranging from simple steatosis to nonalcoholic steatohepatitis (NASH), fibrosis, and ultimately liver cirrhosis. End-stage liver disease secondary to NASH cirrhosis has become the second most common cause for LT and presumably will be the leading indication in the next decade. This is of further importance as current studies have shown that CVDs are especially overrepresented in patients with NASH-related liver disease,5 independent of common underlying risk factors, such as MS and diabetes.6
Several studies have determined the cumulative risk of CVD after LT. Independent predictive factors of CVD are older age at transplantation, male sex, preexisting cardiac disease, and components of the MS.7-9 In addition, patients with underlying NASH cirrhosis have a significantly higher risk of CVD compared to other indications. The frequency of major intraoperative and postoperative cardiac complications was markedly increased in recipients with known heart disease compared to those without. Therefore, it is important to identify and to treat all the parameters of the MS promptly, because these contribute to the development of CVD before LT, and to stratify patients with a high risk for postoperative CVD who are already in the pre-LT setting in order to offer them targeted medical and/or interventional management.
The commonly used immunosuppressive agents, in particular the calcineurin inhibitors cyclosporine A and tacrolimus as well as corticosteroids, are associated with an exacerbation of preexisting as well as the development of de novo MS and each of its individual components, further contributing to the high-CVD risk in LT recipients. Cyclosporine mainly leads to new-onset arterial hypertension and dyslipidemia, whereas tacrolimus is associated with posttransplant diabetes. Mammalian target of rapamycin inhibitors (sirolimus, everolimus) accelerate hypercholesteremia as well as hypertriglyceridemia. Although corticosteroids have the worst CV risk profile by inducing a variety of metabolic effects including insulin resistance, hypertension, dyslipidemia, and obesity, mycophenolates have a better safety profile regarding metabolic disorders. Therefore, tailoring of the immunosuppression is mandatory to ameliorate CVD risk profiles and to minimize CV morbidity and mortality.
In the current issue of Liver Transplantation, Fussner et al.10 provide interesting data regarding the cumulative incidence of obesity, MS, and CVD and potential risk factors associated with these morbidities following LT. In this single-center, retrospective study, 455 patients were included. Although obesity increased significantly from 23.8% at 4 months to 40.8% after 3 years, the prevalence of post-LT MS remained stable with 30% to 50% of LT recipients being affected. Obesity was the only independent predictor for the development of MS. Interestingly, 40% of the patients were obese after 3 years, but only 10% of patients underwent transplantation because of NASH cirrhosis, confirming the fact that all LT recipients independent of the underlying liver disease are at high risk of developing obesity and MS. Confirming previous studies, this article also showed a high prevalence of CVD in LT recipients, which is markedly higher compared to the general population. A steady increase of patients with symptomatic CVD from 10.6% at 1 year to 20.7% and 30.3% at 5 and 8 years after LT, respectively, was observed by the authors. Almost half of the events in the LT group were directly related to atherosclerotic coronary artery disease or myocardial infarction. Overall, 4.4% of patients died because of CVD, and 15.7% of deaths were accounted to CVD demonstrating the negative impact of CVD on the short- and long-term outcome of LT patients.
Beside the traditional risk factors for CVD, such as age, diabetes, and prior history of CVD, this study showed that serum troponin levels of >0.07 ng/mL were associated with an increased risk of CVD in the long-term period. Smoking, sex, hyperlipidemia, serum ferritin, and serum C-reactive protein levels were not predictable. Regarding immunosuppression, the use of tacrolimus showed a beneficial effect on CVD in contrast to other immunosuppressant agents. In patients without a prior history of CVD, age, diabetes, renal dysfunction, immunosuppression, and serum troponin levels were all predictive of de novo CV events defining a potentially high-risk group for the development of CVD.
The pre-LT cardiac work-up is an important issue in order to identify LT candidates with (high) risk for CVD, as (1) more elderly and more patients with preexisting MS are transferred for LT assessment and (2) NASH cirrhosis, an independent risk factor for atherosclerosis and CVD, will be the main indication for LT in the near future. In this study, pretransplant cardiac testing included electrocardiography and echocardiography in all patients; stress imaging studies were performed in all diabetic patients and patients over the age of 50 years followed by angiography in patients with a positive stress test. In a univariate analysis, the left ventricular ejection fraction (EF; 3.5-fold increase with an EF < 50%) and left ventricular hypertrophy were associated with an increased risk of CVD. However, no other predictive parameters could be found during the pre-LT cardiac assessment, demonstrating the limited usefulness of this work-up in order to identify patients with high CVD risk after LT.
Which conclusions can be drawn from this article? The study confirms that CVDs are a still emerging, highly relevant problem in the management of LT recipients. Almost one-third of all patients were diagnosed with a CV event in the long-term follow-up and 15% of all deaths were related to CVD. This fact clearly emphasizes the importance to identify patients with high risk for CVD ideally before LT in order to optimize the postoperative course by closer follow-up visits and aggressive management of potential risk factors. Beside already well-established risk factors for CVD (age, diabetes, positive history of CVD), the authors were able to show that elevated serum troponin I levels before LT were independent predictors of recurrent CVD as well as de novo CVD following LT. Serum troponin I, a specific biomarker for cardiac myofibrillar dysfunction, was measured from stored serum samples obtained at least 6 months before LT and a cutoff of 0.07 ng/mL was chosen. This is no doubt an interesting finding, and troponin I might be a useful marker, independent from MS and other traditional parameters, to identify high-risk patients; however, larger prospective studies are needed to approve of the prognostic efficacy of troponin I for CVD in LT recipients. Regarding postoperative management, this study emphasized the importance to avoid weight gain already in the first months in order to minimize the adverse impact of MS on CVD. Optimizing immunosuppression is a further issue of importance. On the basis of this study, tacrolimus might have a beneficial impact on MS and subsequently CVD; however, randomized trials are needed to confirm this finding.
In summary, this study by Fussner et al.10 from the Mayo Clinic provides new, clinically relevant information regarding the prevalence of CVD, its impact on the short- and long-term outcome as well as potential risk factors. However, more data from larger, prospective studies are needed both to identify patients with high risk of CVD and to optimize the post-LT management in order to minimize MS and CVD and to further improve the long-term outcome of LT recipients.