Liver transplant readmissions: The cost of the revolving door
See Article on Page 953
Abbreviations
-
- CMS
-
- Centers for Medicare and Medicaid Services
-
- LT
-
- liver transplantation
-
- SRTR
-
- Scientific Registry of Transplant Recipients
Unnecessary health care utilization and costs have been increasing, which is of great importance to stakeholders including hospitals, health care systems, policymakers, and insurers. A 2012 provision in the Affordable Care Act called for reductions of Centers for Medicare and Medicaid Services (CMS) reimbursement for excess 30-day readmissions for certain high-risk conditions, the list of which is expected to expand. Though liver transplantation (LT) is a necessary and lifesaving procedure, it is costly and resource intensive. Over time, LT recipients have become progressively sicker at transplantation, leading to longer postoperative stays and a greater risk of readmission.1 However, the scope of this on the national scale and the variability in practice patterns are largely unknown.
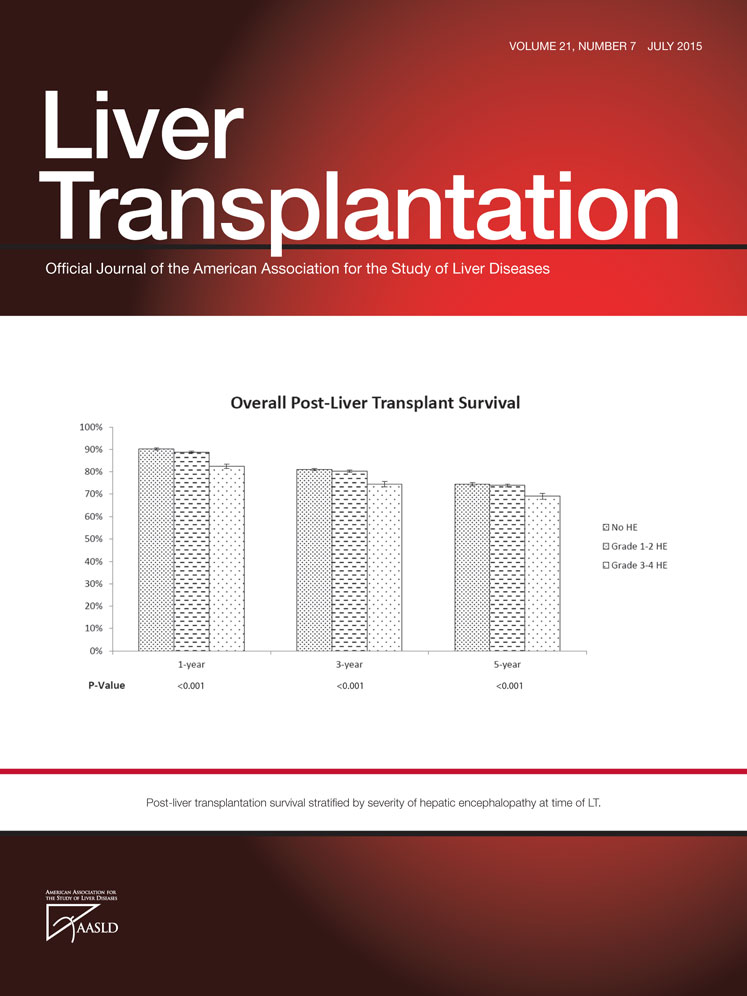
The study by Wilson et al.2 is timely because it is one of the first to quantify the burden of early post-LT readmissions and associated costs by merging 2 national data sources: the University HealthSystem Consortium, which is an administrative claims database that captures data from 50% of transplant centers, and the Scientific Registry of Transplant Recipients (SRTR). Their 5-year analysis of more than 12,000 LT recipients demonstrated 30-day readmission rates of 38% and 90-day readmission rates of 48%—strikingly, approximately one-half of all readmissions occurred within 7 days of discharge. Readmissions within 90 days were associated with about $44,000 in additional transplant-related costs. Their analyses revealed several factors that were strongly associated with an increased risk of readmissions, including pretransplant functional status and the need for pretransplant dialysis. These are important because of the continued prioritization of the sickest patients for LT and how this impacts health care costs. Importantly, despite adjusting for donor, recipient, and geographic factors, there was dramatic variation in readmission rates among hospitals, ranging from 26.3% to 50.8%, with readmitted patients having higher mortality that persisted up to 3 years after LT. The top reasons for readmission were fever in approximately 8.7% of patients, abdominal pain in 3.7%, and acute kidney injury in 2.8%. Interestingly, fever was the top hospitalization reason at centers at both “high risk” and “low risk” for readmission.
This is one of the first studies to examine readmission in LT on a national level with a large sample size and to report on associated costs of readmission. This study provides more detailed data on patient baseline characteristics and clinical outcomes than are available in SRTR, and it adds to a growing literature of the detrimental effects of poor functional status on pretransplant and posttransplant outcomes.3 One of the potential limitations was the inability to track whether the readmission occurred at a different hospital from the transplant surgery as many patients live far from the transplant center. The reasons for admission were administratively coded and may not reflect the true admission reason.4 Lastly, the authors were unable to assess what proportion of readmissions may have been preventable, including patient-specific factors of poor medication understanding and nonadherence, which have been shown to impact posttransplant hospitalizations.5 Though coding inaccuracies may exist and transplant center practices vary, these data suggest the need for quality improvement efforts in the areas of early postoperative infectious complications and close follow-up of renal function.
The 30-day readmission rates noted by the investigators are higher than for conditions currently targeted under the CMS Hospital Readmissions Reduction Program. This will undoubtedly have important implications for payers and transplant centers if LT becomes one of the CMS’ targeted conditions. In the future, it will be important to identify what proportion of readmissions may be preventable, to define quality benchmarks, and to develop targeted interventions to improve posttransplant care and decrease costs.