The impact of pretransplant hepatic encephalopathy on survival following liver transplantation
Financial support: Nothing to report.
Potential conflict of interest: Nothing to report.
Abstract
Hepatic encephalopathy (HE) is a surrogate marker of liver disease severity, and more severe HE is associated with higher mortality among patients with chronic liver disease. However, whether severity of HE at the time of liver transplantation (LT) directly impacts post-LT survival or whether this suspected mortality linkage is due to more severe liver disease and subsequently higher rates of post-LT infection is not well defined. Using population-based data from the 2003 to 2013 United Network for Organ Sharing registry, we evaluated the impact of HE at the time of LT on post-LT survival among adults in the United States. Survival was stratified by HE severity (none, grade 1-2, grade 3-4) and Model for End-Stage Liver Disease score and was evaluated using Kaplan-Meier methods and multivariate Cox proportional hazards models. From 2003 to 2013, 59,937 patients underwent LT (36.1%, no HE; 53.8%, grade 1-2 HE; 10.2%, grade 3-4 HE). Compared to no HE, patients with grade 3-4 HE had significantly lower overall post-LT survival (1-year, 82.5% versus 90.3%; P < 0.001; 5-year, 69.1% versus 74.4%; P < 0.001). On multivariate regression, grade 3-4 HE was independently associated with lower overall post-LT survival (HR, 1.27; 95% CI, 1.17-1.39; P < 0.001). However, the increased mortality associated with HE is observed primarily within the first year following LT and was a reflection of higher rates of infection-related deaths among patients with more severe HE. In conclusion, grade 3-4 HE at the time of LT is associated with lower post-LT survival, with a proposed direct or indirect association of more severe HE before LT with increased rates of post-LT infections. Increased awareness and vigilance toward treating HE before LT and more aggressive monitoring and treatment for infections in the perioperative setting may improve LT outcomes. Liver Transpl 21:873-880, 2015. © 2015 AASLD.
Abbreviations
-
- BMI
-
- body mass index
-
- CI
-
- confidence interval
-
- HCC
-
- hepatocellular carcinoma
-
- HCV
-
- hepatitis C virus
-
- HE
-
- hepatic encephalopathy
-
- HR
-
- hazard ratio
-
- INR
-
- international normalized ratio
-
- IRB
-
- institutional review board
-
- LT
-
- liver transplantation
-
- MELD
-
- Model for End-Stage Liver Disease
-
- OPTN
-
- Organ Procurement and Transplantation Network
-
- SD
-
- standard deviation
-
- UNOS
-
- United Network for Organ Sharing
The implementation of the Model for End-Stage Liver Disease (MELD) score in the prioritization of patients awaiting liver transplantation (LT) is based on the principle of using objective criteria to offer LT to patients with the highest MELD score and thereby the sickest patients first.1, 2 Although the MELD score performs well in predicting the risk of wait-list mortality, it does not incorporate the severity of hepatic encephalopathy (HE) into risk calculations because of the lack of an objective and quantitative scoring system. The grading systems for HE have significant limitations, and the degree of subjectivity with current systems have called into question the accuracy of incorporating HE into risk calculations.3-6 However, the impact of HE on survival among patients with cirrhosis is well established, and HE severity is a component of the well-validated Child-Turcotte-Pugh scoring system.7-10 Despite these limitations, a recent study using data from the United Network for Organ Sharing (UNOS) LT registry in the United States demonstrated that patients with grade 3-4 HE had significantly higher wait-list mortality when compared to patients with no HE, independent of MELD score.3
However, once a patient undergoes LT, it is not clear if the severity of HE at the time of LT affects the post-LT outcomes. A recent retrospective cohort study of 393 adult LT recipients evaluated the impact of pre-LT severe HE on post-LT outcomes.11 Although there was a nonsignificant trend toward a lower 1-year survival among patients with severe HE compared to patients without severe HE (HR, 2.19; P = 0.08), overall hospital length of stay was significantly longer in patients with severe HE. Furthermore, persistent encephalopathy and cognitive impairments may persist following LT among patients with pre-LT HE, which may increase the risk for infections related to aspiration events.12-18 Currently, residual HE or cognitive impairments following LT are not well captured by LT registries. Understanding the impact of pre-LT HE on post-LT outcomes is important in raising awareness of the need to aggressively treat HE during the preoperative period. Using US population–based data from the UNOS and Organ Procurement and Transplant Network (OPTN), the current study evaluates the impact of pre-LT HE on survival following LT.
PATIENTS AND METHODS
Study Population
Using data from the UNOS/OPTN registry, we evaluated adult men and women (age > 18 years) with chronic liver disease who underwent LT in the United States from January 1, 2003 to December 31, 2013. Patients undergoing LT for fulminant liver failure via status 1A prioritization were excluded. MELD scores at the time of LT were calculated for each individual using a standard formula that incorporates the natural logarithms of the international normalized ratio (INR) of prothrombin time, bilirubin, and creatinine with a lower limit of 1 mg/dL for all variables and an upper limit of 4 mg/dL for creatinine. Patients on hemodialysis were given a creatinine score of 4 mg/dL.
HE severity at the time of LT was graded using the West Haven Criteria (grade 0, no HE; grade 1, trivial lack of awareness, euphoria or anxiety, shortened attention span, impaired performance of addition or subtraction; grade 2, lethargy or apathy, minimal disorientation for time or place, subtle personality change, inappropriate behavior; grade 3, somnolence to semistupor but responsive to verbal stimuli, confusion, gross disorientation; grade 4, coma [unresponsive to verbal or noxious stimuli]).4, 6 The grade of HE at the time of LT (no HE, grade 1-2 HE, grade 3-4 HE) was based on clinical diagnosis coding as documented in UNOS. Data regarding the treatment for HE was not captured in the UNOS registry, and additional data points assessing the presence and severity of HE following LT were not available for analysis. Survival following LT was our primary outcome, and the etiology of post-LT death as provided by UNOS was included in our analyses.
Statistical Analysis
Descriptive statistics were stratified by severity of HE and presented as proportions (%) and frequencies (n) for categorical variables, mean and standard deviation (SD) for normally distributed continuous variables, and median and range for nonnormally distributed variables. Comparisons between groups were performed with chi-square testing and analysis of variance methods. Survival following LT was evaluated using Kaplan-Meier methods and log-rank testing for equality of survivor functions. Post-LT survival was further stratified by MELD score and severity of HE to determine whether the association of HE and post-LT survival is dependent on MELD score at the time of LT. Specifically, we calculated 1-year and 5-year post-LT survival rates for each MELD score (from 6 to 40) for patients with no HE, grade 1-2 HE, and grade 3-4 HE. Using this stratified approach, linear regression models were applied to determine whether a significant association between HE at the time of LT and post-LT survival was present, independent of MELD score at LT. Overall long-term survival following LT was further evaluated using multivariate Cox proportional hazards models. Forward stepwise regression methods included variables that were biologically significant (eg, age, sex) and those that demonstrated significant associations in the univariate models (P < 0.10). The final multivariate model was adjusted for sex, age at the time of LT, hepatitis C virus (HCV) infection (versus non-HCV), hepatocellular carcinoma (HCC; versus non-HCC), diabetes, ascites, race/ethnicity, MELD score at the time of LT, and HE grade. Statistical significance was met with a 2-tailed P value < 0.05. Differences in cause of death following LT were stratified by HE grade at the time of LT and evaluated using chi-square testing and probability density functions. All statistical analyses were performed using the Stata statistical package, version 10 (Stata Corporation, College Station, TX) and Prism Statistical Software, version 6.0 (GraphPad Software, Inc., La Jolla, CA). This study was exempt from institutional review board (IRB) review after Stanford University Medical Center IRB review.
RESULTS
Overview
From 2003 to 2013, 59,937 patients with chronic liver disease underwent LT, among which 10.2% (n = 6086) had grade 3-4 HE, 53.8% (n = 32,226) had grade 1-2 HE, and 36.1% (n = 21,625) had no HE at the time of LT (Table 1). Although the majority of patients were men, there was a higher proportion of men with no HE compared to patients with grade 3-4 HE (68.3% versus 64.5%; P < 0.001). When compared to patients with no HE at the time of LT, there was a higher proportion of Hispanics (14.4% versus 11.9%; P < 0.001) and lower proportion of Asians (3.8% versus 6.5%; P < 0.001) among patients with grade 3-4 HE (Table 1). When we evaluated the proportion of patients with grade 3-4 HE within each race/ethnic group, 100% of non-Hispanic whites, 9.9% of blacks, 11.0% of Hispanics, and 8.8% of Asians had grade 3-4 HE. LT recipients with no HE were also significantly more likely to have concurrent HCC when compared to patients with grade 3-4 HE (30.2% versus 5.5%; P < 0.001). Patients with grade 3-4 HE had higher MELD scores and higher prevalence of concurrent moderate ascites (Table 1).
| No HE, n = 21,625 | Grade 1-2 HE, n = 32,226 | Grade 3-4 HE, n = 6086 | P Value | |
|---|---|---|---|---|
| Sex, male | 14,776 (68.3) | 21,959 (68.1) | 3928 (64.5) | <0.001 |
| Age, years | 53.7 ± 10.9 | 54.2 ± 9.3 | 52.7 ± 10.3 | <0.001 |
| Race/ethnicity | <0.001 | |||
| Non-Hispanic white | 15,215 (71.0) | 23,850 (74.8) | 4363 (72.6) | |
| Black | 2295 (10.7) | 2710 (8.5) | 553 (9.2) | |
| Hispanic | 2541 (11.9) | 4354 (13.7) | 862 (14.4) | |
| Asian | 1391 (6.5) | 978 (3.1) | 229 (3.8) | |
| HCV | 8199 (51.4) | 13,392 (49.1) | 2215 (46.6) | <0.001 |
| HCC | 6521 (30.2) | 3960 (12.3) | 333 (5.5) | <0.001 |
| MELD score | 17.2 ± 8.7 | 22.3 ± 9.0 | 29.9 ± 8.7 | <0.001 |
| Moderate ascites | 2725 (12.9) | 10,036 (31.2) | 4155 (68.3) | <0.001 |
| Diabetes | 3941 (19.5) | 5948 (20.1) | 1070 (19.2) | 0.13 |
| Obesity, BMI > 30 kg/m2 | 6411 (29.7) | 11,385 (35.3) | 2086 (34.3) | <0.001 |
| BMI, kg/m2 | 27.6 ± 5.5 | 28.4 ± 5.7 | 28.1 ± 5.9 | <0.01 |
| Albumin g/dL | 3.1 ± 0.7 | 2.9 ± 0.7 | 2.9 ± 0.8 | 0.02 |
| Sodium mmol/L | 136.8 ± 4.6 | 135.4 ± 5.2 | 137.2 ± 6.4 | 0.02 |
| INR | 1.4 (0.9-4.3) | 1.7 (1.0-5.2) | 2.2 (1.1-9.9) | <0.001 |
- NOTE: Data are given as n (%), as mean ± SD, or as median (range).
Survival Following LT
Compared to patients with no HE at the time of LT, patients with grade 3-4 HE had significantly lower survival following LT (Fig. 1). For example, overall 1-year post-LT survival among patients with grade 3-4 HE was 82.5% (95% CI, 81.6%-83.4%) compared to 90.3% (95% CI, 89.8%-90.7%) among patients with no HE. Similar trends were seen when evaluating 5-year post-LT survival (69.1% [grade 3-4 HE] versus 74.4% [no HE]); P < 0.001; Fig. 1). To determine whether the impact of HE on post-LT survival varied by MELD score at the time of LT, we stratified post-LT survival by MELD score categories (<15, 15-25, >25; Fig. 2). Among patients with a MELD score of <15, there was a nonsignificant trend toward lower 1-year post-LT survival among patients with grade 3-4 HE compared to patients with no HE at the time of LT. With higher MELD scores, the impact of HE on post-LT survival became more significant. For example, among patients with a MELD score of >25 at the time of LT, patients with grade 3-4 HE had significantly lower 1-year post-LT survival when compared to patients with no HE at the time of LT (79.2% versus 85.9%; P < 0.01; Fig. 2). Similar trends were seen when evaluating 5-year post-LT survival with the greatest impact of HE seen among patients with a MELD score of >25 (64.6% versus 71.5%; P < 0.01; Fig. 2). Using linear regression methods, we further evaluated the impact of HE stratified by incremental 1-unit increases in MELD score at the time of LT (Fig. 3). Although higher MELD scores were associated with lower 1-year post-LT survival for all categories of HE (grade 3-4 HE, P < 0.001; grade 1-2 HE, P < 0.02; no HE, P < 0.001), there was no significant difference in 1-year post-LT survival between patients with grade 3-4 HE versus no HE when stratified by individual MELD score at the time of LT (P = 0.18; Fig. 3). Similar findings were observed for 5-year survival, with no significant difference in survival between grade 3-4 HE versus no HE when stratified by individual MELD score at the time of LT (P = 0.47; Fig. 3).
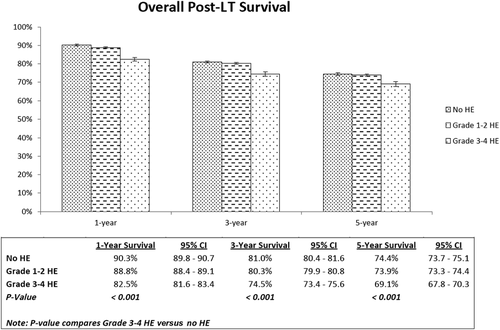
Overall post-LT survival stratified by severity of HE at the time of LT.
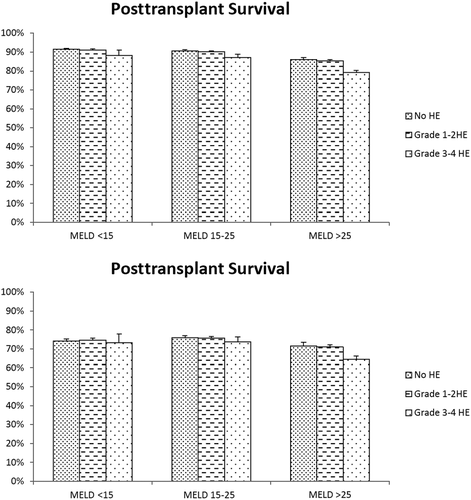
Overall 1-year and 5-year survival following LT stratified by MELD categories. Error bar represents upper limit of 95% confidence interval.
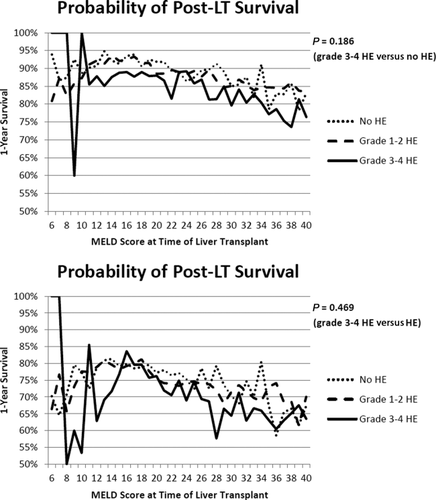
Crude 1-year and 5-year post-LT survival stratified by HE grade and MELD score.
However, when MELD at the time of LT was adjusted for in the multivariate Cox regression model, grade 3-4 HE at the time of LT was independently associated with significantly lower post-LT survival compared to patients with no HE (HR, 1.27; 95% CI, 1.17-1.39; P < 0.001; Table 2). Compared to non-Hispanic whites, blacks had lower post-LT survival, whereas Asians and Hispanics had higher post-LT survival. HCV, HCC, and concurrent diabetes mellitus were also associated with significantly lower survival following LT (Table 2). Given that both HCV and HCC are associated with lower overall post-LT survival, we performed a sensitivity analysis by removing each of these groups to determine whether the impact of HE on post-LT survival persisted. Despite removing HCV and HCC patients, the effect measure associated with the impact of HE on survival following LT remained unchanged.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P Value | HR | 95% CI | P Value | |
| HE Grade | ||||||
| No NE | 1.00 | Reference | — | 1.00 | Reference | — |
| Grade 1-2 HE | 1.06 | 1.02-1.10 | <0.01 | 1.04 | 0.98-1.11 | 0.15 |
| Grade 3-4 HE | 1.34 | 1.27-1.41 | <0.001 | 1.27 | 1.17-1.39 | <0.001 |
| MELD score | 1.01 | 1.01-1.01 | <0.001 | 1.01 | 1.01-1.02 | <0.001 |
| Race/ethnicity | ||||||
| Non-Hispanic white | 1.00 | Reference | — | 1.00 | Reference | — |
| Black | 1.32 | 1.26-1.39 | <0.001 | 1.30 | 1.32-1.40 | <0.001 |
| Hispanic | 0.95 | 0.91-1.00 | 0.07 | 0.88 | 0.82-0.94 | <0.001 |
| Asian | 0.78 | 0.72-0.85 | <0.001 | 0.86 | 0.75-0.97 | 0.02 |
| Sex | 1.04 | 1.01-1.08 | 0.01 | 0.98 | 0.93-1.03 | 0.44 |
| Recipient age | 1.02 | 1.01-1.02 | <0.001 | 1.02 | 1.02-1.02 | <0.001 |
| HCV | 1.42 | 1.36-1.47 | <0.001 | 1.55 | 1.48-1.63 | <0.001 |
| HCC | 1.17 | 1.12-1.22 | <0.001 | 1.20 | 1.13-1.28 | <0.001 |
| Year of LT | 0.99 | 0.99-1.00 | <0.01 | 0.98 | 0.97-0.99 | <0.001 |
| Diabetes mellitus | 1.28 | 1.23-1.34 | <0.001 | 1.23 | 1.17-1.30 | <0.001 |
| Ascites | 1.09 | 1.04-1.13 | <0.001 | 0.99 | 0.92-1.06 | 0.76 |
| Serum sodium | 1.01 | 1.01-1.01 | <0.001 | 1.01 | 1.00-1.01 | <0.01 |
| Portal vein thrombosis | 1.26 | 1.18-1.34 | <0.001 | 1.23 | 1.13-1.33 | <0.001 |
| Dialysis | 1.52 | 1.45-1.60 | <0.001 | 1.35 | 1.25-1.46 | <0.001 |
| UNOS region | 0.99 | 0.99-1.00 | 0.70 | 1.01 | 1.00-1.01 | 0.08 |
| Donor age | 1.01 | 1.01-1.01 | <0.001 | 1.01 | 1.01-1.01 | <0.001 |
To further investigate these discrepant results, we evaluated the etiology of post-LT death stratified by grade of HE at the time of LT (Supporting Table 1). In addition, the etiology of post-LT death was also evaluated separately for patients who died within 1 year following LT and patients who survived 1 year but died within 5 years following LT, given the hypothesis that the increased mortality associated with HE may be primarily observed within the first year following LT. Overall, infection was a leading etiology of post-LT death, accounting for 18.4% of deaths among patients with grade 3-4 HE, 15.4% among patients with grade 1-2 HE, and 14.4% among patients with no HE (Supporting Table 1). Among patients who died within 1 year following LT, higher rates of infection-related deaths were seen with higher grades of HE, but this trend was not seen among patients who survived beyond 1 year but died within 2 to 5 years. Using probability density functions, patients with grade 3-4 HE demonstrated a significantly different 1-year probability death curve compared to patients with grade 1-2 HE or patients with no HE, but no difference was seen in 5-year probability death curves (Fig. 3). A major contributor of HE grade-specific differences in 1-year probability death curves was a result of differences in rates of infection-related deaths at 1 year between patients with different severities of HE (Fig. 4). We also evaluated hospital stay following LT stratified by HE severity (no HE, median, 9 days, range, 2-739; grade 1-2 HE, median, 10 days, range, 1-1121; grade 3-4 HE, median, 16 days, range, 1-419).
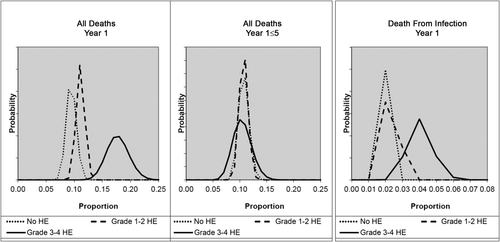
Probability density function of post-LT death stratified by HE severity.
DISCUSSION
Current prioritization models among patients with chronic liver disease awaiting LT do not incorporate HE severity. Although previous studies have suggested that severity of HE is associated with higher LT wait-list mortality, this observation may be explained by the fact that HE is a surrogate for more severe overall liver dysfunction, thereby leading to higher wait-list mortality.2, 3, 11, 18-20 It follows then that if more severe HE is a surrogate for more severe liver dysfunction before LT, more severe HE at the time of LT may be associated with higher perioperative complications leading to higher postoperative mortality because of increased risks of post-LT infections. The impact of pre-LT HE on post-LT outcomes is not well understood, and current studies are conflicting as to whether inadequately treated HE at the time of LT negatively impacts post-LT survival and if correcting HT pre-LT would improve post-LT survival and cognitive function.11, 13, 18-22 Using MELD-era registry data from UNOS/OPTN, our current study suggests that although patients with grade 3-4 HE at the time of LT had 28% higher risk of post-LT mortality compared to patients with no HE, this survival difference is predominantly explained by differences in survival within the first year following LT. Furthermore, the higher post-LT mortality associated with grade 3-4 HE is largely explained by infection-related deaths.
The higher post-LT mortality associated with severe HE is not entirely clear and reflects the multifactorial nature of post-LT death. In a single-center retrospective cohort study of 393 adult LT recipients in the United States from 2002 to 2005, Brandman et al.11 evaluated the impact of severe HE within 30 days before LT on post-LT outcomes. Patients with severe HE had a significantly longer hospital stay, greater odds of infection in the post-LT period (odds ratio, 3.26; 95% CI, 1.61-6.59), and greater odds of prolonged post-LT altered mental status (odds ratio, 3.62; 95% CI, 1.80-7.29). However, the study noted no significant differences in post-LT survival or etiology of post-LT death between patients with severe HE and those with no HE. The relationship between HE and post-LT mortality was further diminished after adjusting for MELD score, and HE alone was not an independent predictor of post-LT mortality.11 However, the authors acknowledged their relatively smaller sample size and limited power to detect statistically significant differences in post-LT survival between groups with and without severe HE. In addition, the overall post-LT survival among all patients was higher than expected, which may have further limited the ability to detect survival differences.11 In our current study, whereas there was no significant difference in 1-year post-LT survival between patients with grade 3-4 HE versus no HE when stratified by individual MELD scores, after correction for MELD score in a multivariate Cox proportional hazards model, the presence of grade 3-4 HE was independently associated with lower post-LT survival compared to patients with no HE.
The impact of HE on post-LT survival is complex and likely reflects multiple measured and unmeasured factors. Although more severe HE at the time of LT may simply reflect more severe liver dysfunction, which is associated with a higher risk of perioperative complications and mortality, additional studies have also demonstrated that more severe HE is associated with higher rates of post-LT infections, which may subsequently directly or indirectly impact post-LT outcomes.2, 3, 11, 13, 18, 20, 22-25 Our current study demonstrated that grade 3-4 HE is associated with increased post-LT mortality, but this increase in mortality was primarily seen within the first year following LT. When evaluating the cause of death following LT, we also observed that the increased mortality associated with HE is significantly associated with infection-related deaths. Although these findings confirm the findings of previous studies, they must be interpreted with some caution. The observational nature of our study and others only allows for the determination of association and not causation. Thus, although we postulate that more severe HE at the time of LT may lead to more infections following LT, it is also plausible that post-LT de novo infections precipitate the development of HE following LT, a biological mechanism that is well established and may further contribute to poorer survival.6, 22, 26-28 Nevertheless, our study does raise concerns that severe HE before LT is directly or indirectly associated with higher post-LT mortality, and there is a need for increased awareness and vigilance to aggressively treat pre-LT HE and perioperative infections.
The current study incorporates 11 years of MELD era data from a population-based LT registry that includes all adult LTs performed in the United States. The utilization of data from a single registry strengthens the consistency of demographic and clinical data reported, and the use of population-based data improves the generalizability of our findings. However, there are inherent limitations of registry-based cohort studies that must be acknowledged. Data available for study analyses are subject to potential data entry errors or miscoding, and cross-checking for accuracy of data entry may not be implemented in all reporting centers. Specific to our study, although data regarding HE severity are reported from grades 0 to 4 as per West Haven Criteria, it is not entirely clear whether all reporting centers used structured grading schemes, and there exists the potential for misclassification of HE severity both at the time of diagnosis and at the time of data entry. The relative subjectivity of HE severity has also been criticized, and this may further contribute to misclassification of HE in our study. Although severity of HE at the time of LT was available for analysis, data regarding HE treatment and post-LT HE severity were not available. It is possible that differences in how aggressive HE was treated after LT may have impacted perioperative complications (eg, aspiration, infection). Furthermore, evaluating the severity of HE at the time of LT does not capture the period immediately preceding LT, and patients who had severe HE in the short-term before LT may not be captured in the current analysis. However, it is likely that HE at the time of LT is not directly causative of increased post-LT mortality but rather a surrogate for other unmeasured factors (eg, sepsis, multiorgan failure) that impact post-LT outcomes. In an attempt to clarify this association, our study demonstrated that the higher mortality seen among patients with grade 3-4 HE during the first year following LT is partly explained by higher infection-related deaths. However, more specific details about the source and severity of the infection (eg, what organ system involved, what organism isolated, what treatments attempted) were not available for analysis. Furthermore, data for etiology of death following LT is provided in broad categories, and more specific details (eg, what types of perioperative complications, what types of malignancies, what types of cardiovascular complications) were not available for inclusion in this study. In addition, other clinical and nonclinical data (eg, socioeconomic status) including unmeasured confounders that were not available for analyses may have affected overall post-LT survival. Although our data was inclusive of all adult LTs in the United States, we did not have the ability to evaluate outcomes at the level of each individual LT center, and differences in practice patterns at the center level may contribute to some of the variations in post-LT outcomes observed. Despite these limitations, our large population-based cohort study adds greatly to better understanding the potential impact of pre-LT HE on post-LT outcomes.
In conclusion, among adult patients with chronic liver disease in the United States, the presence of grade 3-4 HE at the time of LT was independently associated with lower survival following LT. This increased mortality associated with severe HE is observed primarily within the first year following LT and is a reflection of higher rates of infection-related deaths among patients with more severe HE. Increased awareness and vigilance toward treating HE in the pre-LT setting as well as infections in both the pre-LT and post-LT settings may further contribute to improved outcomes among patients with chronic liver disease in the United States.
ACKNOWLEDGMENT
We would like to acknowledge the statistical assistance provided by Dr. Jerry Gardner.