Right lobe split liver transplantation versus whole liver transplantation in adult recipients: A systematic review and meta-analysis
Potential conflict of interest: Nothing to report.
The study was supported by the Key Joint Research Program of Shanghai Health Bureau (2013ZYJB0001) and a subtopic of Scientific and Technological Innovation and Action Project of Shanghai Science and Technology Commission (14411950404).
Abstract
Split liver transplantation (SLT) has proven to be an effective technique to reduce the mortality of children on the waiting list, but whether creating 2 split grafts from 1 standard-criteria whole liver would compromise outcomes of adult recipients remains uncertain. We conducted this meta-analysis to compare outcomes of right lobe SLT and whole liver transplantation (WLT) in adult patients. PubMed, Embase, and the Cochrane Library were searched for relevant articles published before December 2014. Outcomes assessed were patient survival (PS), graft survival (GS), and major surgical complications after transplantation. Pooled odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to synthesize the results. Seventeen studies with a total of 48,457 patients met the full inclusion criteria. PS and GS rates were all found to be equivalent between SLT and WLT recipients. However, SLT was associated with higher rates of overall biliary complications (OR = 1.66; 95% CI = 1.29-2.15; P < 0.001), bile leaks (OR = 4.30; 95% CI = 2.97-6.23; P < 0.001), overall vascular complications (OR = 1.81; 95% CI = 1.29-2.53; P < 0.001), hepatic artery thromboses (OR = 1.71; 95% CI = 1.17-2.50; P = 0.005), and outflow tract obstructions (OR = 4.17; 95% CI = 1.75-9.94; P = 0.001). No significant difference was observed in incidences of biliary stricture, portal vein complications, postoperative bleeding requiring surgical treatments, primary nonfunction, and retransplantations. In subgroup analyses, biliary and vascular complications only increased after ex vivo SLT rather than in situ SLT, and SLT recipients had more retransplantations if they matched with WLT recipients in terms of urgent status. In conclusion, adult right lobe SLT was associated with increased biliary and vascular complications compared with WLT, but it did not show significant inferiority in PSs and GSs. Liver Transpl 21:928-943, 2015. © 2015 AASLD.
Abbreviations
-
- CI
-
- confidence interval
-
- CIT
-
- cold ischemia time
-
- df
-
- degrees of freedom
-
- ERG
-
- extended right graft
-
- GS
-
- graft survival
-
- HAT
-
- hepatic artery thrombosis
-
- LT
-
- liver transplantation
-
- MELD
-
- Model for End-Stage Liver Disease
-
- M-H
-
- Mantel-Haenszel
-
- NA
-
- not available
-
- NITp
-
- North Italian Transplant program
-
- OR
-
- odds ratio
-
- OTO
-
- outflow tract obstruction
-
- PBRST
-
- postoperative bleeding requiring surgical treatments
-
- PNF
-
- primary nonfunction
-
- PRISMA
-
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
-
- PS
-
- patient survival
-
- PVC
-
- portal vein complication
-
- RG
-
- right graft
-
- SLT
-
- split liver transplantation
-
- S1+S4-8
-
- segments I and IV to VIII
-
- S1+S5-8
-
- segments I and V to VIII
-
- S4-8
-
- segments IV to VIII
-
- UNOS
-
- United Network for Organ Sharing
-
- WLT
-
- whole liver transplantation
Full-size liver transplantation (LT) was first introduced by Starzl et al.1 and has currently evolved as the optimal treatment modality for patients with end-stage liver diseases. With an increasing number of patients requiring donor organs, the number of whole liver cadaveric grafts is progressively inadequate. Split liver transplantation (SLT) was initially described in 1988 by Pichlmayr et al.,2 which offered an attractive concept because it allowed transplantation of 2 recipients with 1 liver. Facing a severe shortage of size-matched pediatric whole organs, SLT has proven to be an effective technique to reduce the mortality of children on the waiting list.3
However, the splitting procedure has not gained wide acceptance. This is not only because SLT is technically complicated, but also because it might yield outcomes merely comparable to marginal grafts in right graft (RG) recipients even though it uses ideal quality organs from optimal donors.4-10 Many studies have directly compared SLT with whole liver transplantation (WLT), but these studies have failed to reach a consensus on outcomes or impacts of splitting livers. On the other hand, SLT is associated with prolonged cold ischemia time (CIT)11 and a potential risk for increased complications after transplantation,12-14 which also results in caution at many centers when considering this technique. Whether creating 2 split grafts from 1 standard-criteria whole liver would compromise outcomes of adult recipients remains uncertain. If results with right split grafts are to be as good as with whole grafts in adult patients, the use of split livers for pediatric patients could be fully accepted and implemented. We herein performed a systematic review and meta-analysis to compare survival outcomes and postoperative complication rates between right lobe SLT and WLT in adult recipients.
PATIENTS AND METHODS
Literature Search
The literature search was conducted on major medical databases such as PubMed, Embase, and the Cochrane Library for relevant articles published before December 2014. To supplement the primary search, we performed an additional search with Google Scholar. Combinations of the following terms were used: SLT, WLT, full-size LT, split liver, cadaveric donor, and LT. Reference lists in all relevant studies and related review articles were also checked for eligible studies. Two authors (P.W. and Q.L.) carried out searches independently. Only studies published in English were identified. There were no search restrictions with respect to publication types. The study protocol was approved by the Science and Research Office of Ren Ji Hospital (Shanghai).
Inclusion and Exclusion Criteria
All published clinical studies that compared SLT with WLT in adult recipients were included for further screening. The exclusion criteria were as follows: (1) reviews, case reports, letters, and editorials; (2) studies without WLT recipients as a control group; (3) studies that included too many pediatric recipients (>20%) but lacked a separate analysis for adult patients; (4) studies without any available data of outcomes of interest; (5) studies investigating only patients with hepatocellular carcinoma; (6) studies excluding patients who died in the perioperative period; (7) studies without a separate analysis for right lobe SLT recipients or studies that did not clearly describe the splitting graft types; and (8) studies comparing full-right-full-left SLT for 2 adult recipients with WLT. As described in our previous work,15 studies based on overlapping cohorts from the same institutions might be included in the meta-analysis simultaneously if these studies reported different outcome data. However, only 1 study of better quality was chosen in each synthetic analysis for a single outcome.
Outcomes of Interest
We assessed posttransplant survival outcomes and surgical complications in the meta-analysis. As for survival outcomes, 3-month, 1-year, 3-year, and 5-year patient survival (PS) rates as well as graft survival (GS) rates were analyzed. Specific posttransplant surgical complications included overall biliary complications, bile leak, biliary stricture, overall vascular complications, hepatic artery thrombosis (HAT), portal vein complications (PVCs), outflow tract obstruction (OTO), postoperative bleeding requiring surgical treatments (PBRST), primary nonfunction (PNF), and retransplantation.
Data Extraction and Quality Assessment
Data were independently extracted by 2 observers (J.Z. and Q.X.) from each study with standardized forms. The following information was entered into a database: study characteristics (first author, year of publication, country, source journal, study design, and study period), population characteristics in each group (sample size, ages of donors and recipients, sexes of donors and recipients, body weights of donors and recipients, the Model for End-Stage Liver Disease [MELD] score, the United Network for Organ Sharing [UNOS] status, patient diagnosis, graft-to-recipient weight ratio, and CIT), split methods (in situ/ex situ), splitting graft types, and data of outcomes of interest. We used the Newcastle-Ottawa quality assessment scale16 to assess the quality of selected studies.
Statistical Analysis
Data analyses were performed using RevMan software version 5.0.0 in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17 All variables were expressed as dichotomous data, for which odds ratios (ORs) with 95% confidence intervals (CIs) were calculated. P values of <0.05 were considered to indicate statistical significance in tests for the size of effect. Heterogeneity among studies was evaluated using the Q statistic and the I2 statistic (P values < 0.1 or I2 > 50% were considered to represent significant heterogeneity).18 If no significant heterogeneity was observed, the fixed-effect model was used for the calculation of pooled ORs; otherwise, the random-effect model was used. To test the robustness of results and investigate the source of heterogeneity, subgroup analyses were performed using several important factors that might have a potential impact on the results obtained. In sensitivity analyses, we also excluded each study in turn to estimate the influence of a single study on the pooled estimate. Potential publication bias was evaluated using funnel plots.
RESULTS
Study Characteristics
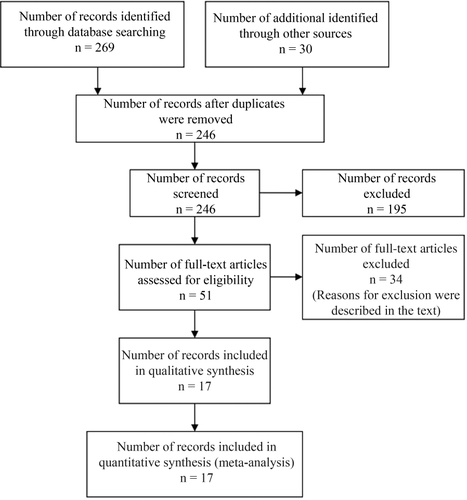
As shown in Fig. 1, we identified 246 relevant articles through a systematic literature search, from which 195 ineligible or irrelevant articles were excluded after retrieving titles and abstracts. The remaining 51 articles were formally reviewed in the full text. After independent reviews, 34 full-text articles were excluded for the following reasons: (1) 10 studies did not have WLT recipients as a control group; (2) 4 studies involved too many children but lacked a separate analysis for adult recipients; (3) 9 studies lacked available data of outcomes of interest; (4) 1 study excluded patients who died in the perioperative period; (5) 7 studies lacked a separate analysis of right lobe SLT recipients or did not clearly describe the splitting graft types; and (6) 3 studies investigating the comparison of outcomes between full-right-full-left SLT and WLT. Finally, 17 clinical studies were included in the meta-analysis, all of which were performed on the basis of retrospective cohorts.12, 19-34
Characteristics of the 17 included studies are summarized in Table 1. Fourteen studies had comparable recipient ages between SLT and WLT groups, but SLT recipients were younger than WLT recipients in the study by Mallik et al.26 Donor ages were equivalent between the 2 groups in 6 studies (conducted by Corno et al.,23 Bonney et al.,24 Broering et al.,28 Wilms et al.,29 Takebe et al.,12 and Sainz-Barriga et al.33), whereas the SLT group had significantly younger donor ages in 10 studies. Moreover, we extracted different outcome data from the studies based on overlapping cohorts, and thus, no overlapping cohorts were simultaneously involved in the synthesis for a single outcome. After quality assessments with the Newcastle-Ottawa scale, all studies were assigned with 6 or more stars except that the study by Ghobrial et al.31 received only 5 stars (Table 2).
| References | Country | Study Period | Arm | Sample Size | Recipient Age, Years | Donor Age, Years | Urgent Status Matchinga | Split Method (In Situ/Ex Situ) | Graft Type |
|---|---|---|---|---|---|---|---|---|---|
| Maggi et al.19 (2005) | Italy | 1993–2004 | SLT | 20 | 46 ± 12 | 31 ± 14 | Yes | In situ | ERG in 19 patients, RG in 1 patient |
| WLT | 261 | 45 ± 10 | 41 ± 17 | ||||||
| Cardillo et al.20 (2006)b | Italy | 1997–2002 | SLT | 154 | 48 ± 13 | 31 ± 15 | Yes | In situ | ERG |
| WLT | 1126 | 46 ± 15 | 44 ± 20 | ||||||
| Spada et al.21 (2005)c | Italy | 1997–2003 | SLT | 15 | 51 (24-62) | 26 (13-60) | Yes | In situ | ERG |
| WLT | 87 | 52 (19-65) | 53 (5-78) | ||||||
| Baccarani et al.22 (2005) | Italy | 1998–2004 | SLT | 14 | 54 | 32 ± 18 | NA | In situ | ERG |
| WLT | 194 | NA | 45 ± 18 | ||||||
| Corno et al.23 (2006)c | Italy | 1997–2005 | SLT | 22 | 50 (23-63) | 22 (12-61) | Yes | In situ | ERG |
| WLT | 48 | 55 (19-65) | 54 (17-79) | ||||||
| Bonney et al.24 (2008) | United Kingdom | 2000–2006 | SLT | 27 | 52 (22-68) | 40 (15-54) | Yes | Ex situ | ERG |
| WLT | 27 | 53 (34-74) | 47 (19-79) | ||||||
| Mabrouk Mourad et al.25 (2015)d | United Kingdom | 2000–2012 | SLT | 171 | 50 ± 13 | 29 ± 10 | Yes | 98% ex situ | S1+S4-8 in 131 patients, S4-8 in 29 patients, S1+S5-8 in 6 patients |
| WLT | 1412 | 51 ± 12 | 46 ± 14 | ||||||
| Mallik et al.26 (2012) | United Kingdom | 2004–2010 | SLT | 17 | 50 (28-69) | 23 (12-60) | Yes | Ex situ | ERG |
| WLT | 32 | 58 (46-69) | 34 (14-64) | ||||||
| Leithead et al.27 (2014)d | United Kingdom | 2007–2011 | SLT | 72 | 52 ± 13 | 29+10 | Yes | Ex situ | ERG |
| WLT | 72 | 52 ± 11 | 48+15 | ||||||
| Broering et al.28 (2002)e | Germany | 1993–1999 | SLT | 40 | 51 (20-65) | 32 (15-61) | Yes | 68% in situ | ERG |
| WLT | 40 | 51 (20-65) | 34 (16-65) | ||||||
| Wilms et al.29 (2006)e | Germany | 1993–2005 | SLT | 70 | 51 (16-69) | 34 (15-64) | Yes | 53% ex situ | ERG |
| WLT | 70 | 51 (16-69) | 38 (0-73) | ||||||
| Takebe et al.12 (2009) | Germany | 1998–2007 | SLT | 80 | 42 (15-65) | 33 (7-60) | Yes | Ex situ | ERG |
| WLT | 80 | 43 (18-64) | 38 (14-64) | ||||||
| Hong et al.30 (2009)f | United States | 1993–2006 | SLT | 72 | 51 | 20 | NA | In situ | ERG |
| WLT | 2433 | 52 | 37 | ||||||
| Ghobrial et al.31 (2000)f | United States | 1996–1999 | SLT | 52 | NA | NA | NA | In situ | ERG |
| WLT | 628 | NA | NA | ||||||
| Lee et al.32 (2008)f | United States | 1996–2006 | SLT | 568 | 51 ± 11 | 25 ± 10.3 | No | 52% in situ | Right-side grafts |
| WLT | 40304 | 51 ± 10 | 40 ± 18 | ||||||
| Sainz-Barriga et al.33 (2008) | Belgium | 2001–2005 | SLT | 12 | 52 ± 12 | 33 (14-16) | Yes | 75% ex situ | ERG |
| WLT | 12 | 55 ± 7 | 44 (22-63) | ||||||
| Sandroussi et al.34 (2009) | Australia | 2002–2007 | SLT | 43 | 53 (17-67) | 39 (13-61) | No | 88% in situ | ERG |
| WLT | 182 | 52 (17-69) | 47 (12-79) |
- NOTE: Data for donor and recipient age are given as mean ± standard deviation, median (range), or median.
- a Urgent status matching was based on the MELD score or the UNOS status.
- b The study cohort reported by Cardillo et al. was based on data from 7 centers, which overlapped with all other Italian cohorts.
- c These references were based on overlapping cohorts.
- d These references were based on overlapping cohorts.
- e These references were based on overlapping cohorts.
- f These references were based on overlapping cohorts.
| References | Selection Star | Comparability Star | Outcome Star | Total Star |
|---|---|---|---|---|
| Maggi et al.19 (2005) | 3 | 2 | 3 | 8 |
| Cardillo et al.20 (2006) | 3 | 2 | 3 | 8 |
| Spada et al.21 (2005) | 3 | 2 | 3 | 8 |
| Baccarani et al.22 (2005) | 3 | 0 | 3 | 6 |
| Corno et al.23 (2006) | 3 | 2 | 3 | 8 |
| Bonney et al.24 (2008) | 3 | 2 | 3 | 8 |
| Mabrouk Mourad et al.25 (2015) | 3 | 2 | 3 | 8 |
| Mallik et al.26 (2012) | 3 | 1 | 3 | 7 |
| Leithead et al.27 (2014) | 3 | 2 | 3 | 8 |
| Broering et al.28 (2002) | 3 | 2 | 3 | 8 |
| Wilms et al.29 (2006) | 3 | 2 | 3 | 8 |
| Takebe et al.12 (2009) | 3 | 2 | 3 | 8 |
| Hong et al.30 (2009) | 3 | 1 | 3 | 7 |
| Ghobrial et al.31 (2000) | 2 | 0 | 3 | 5 |
| Lee et al.32 (2008) | 3 | 1 | 3 | 7 |
| Sainz-Barriga et al.33 (2008) | 3 | 2 | 3 | 8 |
| Sandroussi et al.34 (2009) | 3 | 1 | 3 | 7 |
Patient Survival
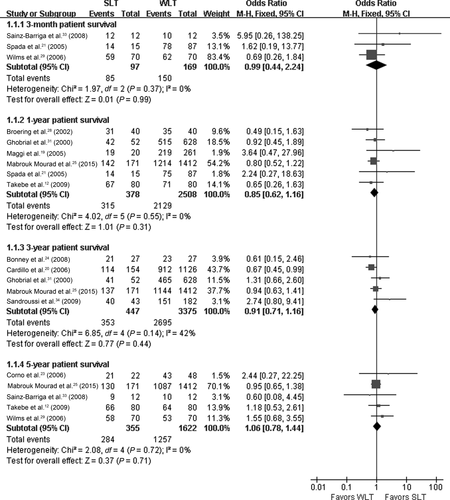
Twelve studies reported data of PS. In 11 studies, there was no significant difference observed between SLT and WLT recipients; but the remaining 1 study showed that WLT was associated with higher PS rates. Figure 2 summarizes PS outcomes for SLT and WLT recipients. No significant heterogeneity was shown among the 3 studies reporting 3-month PS rates (P = 0.37; I2 = 0%), the 6 studies reporting 1-year PS rates (P = 0.55; I2 = 0%), the 5 studies reporting 3-year PS rates (P = 0.14; I2 = 42%), or the 5 studies reporting 5-year PS rates (P = 0.72; I2 = 0%). A fixed-effect model revealed that all pooled PS rates were found to be equivalent between SLT and WLT recipients (3-month, OR = 0.99; 95% CI = 0.44-2.24; P = 0.99; 1-year, OR = 0.85; 95% CI = 0.62-1.16; P = 0.31; 3-year, OR = 0.91; 95% CI = 0.71-1.16; P = 0.44; 5-year, OR = 1.06; 95% CI = 0.78-1.44; P = 0.71).
Graft Survival
Data of GS were reported in 14 of the included studies. Among them, 12 studies showed comparable results between SLT and WLT groups, whereas 2 studies indicated higher GS rates in WLT recipients. Specifically, 3-month, 1-year, 3-year, and 5-year GS rates were available in 2 studies, 8 studies, 6 studies and 8 studies, respectively. Significant heterogeneity was observed only in 3-year GS rates (P = 0.07; I2 = 52%), and satisfactory homogeneity was found in other GS outcomes (3-month, P = 0.33; I2 = 0%; 1-year, P = 0.61; I2 = 0%; 5-year, P = 0.50; I2 = 0%). A random-effect model was used to combine the data to control potential heterogeneity (Fig. 3). Pooled data suggested that GS rates in SLT recipients were similar to those in WLT recipients (3-month, OR = 0.68; 95% CI = 0.31-1.49; P = 0.33; 1-year, OR = 0.91; 95% CI = 0.76-1.08; P = 0.27; 3-year, OR = 0.84; 95% CI = 0.62-1.13; P = 0.25; 5-year, OR = 0.98; 95% CI = 0.85-1.14; P = 0.82).

Postoperative Complications
Biliary Complications
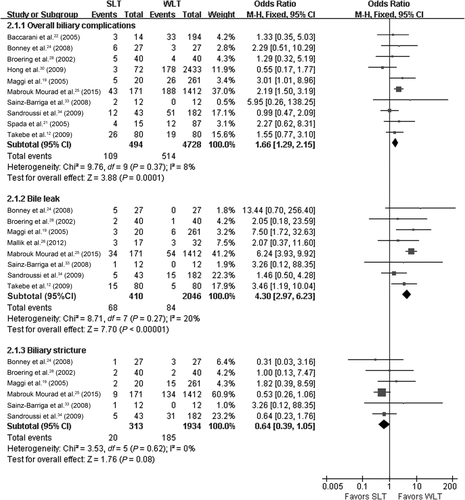
Overall biliary complication rates were reported in 10 studies. In 9 of these studies, no significant difference was observed between SLT and WLT recipients, whereas 1 study suggested the overall biliary complication rate was higher in SLT recipients. We observed no significant heterogeneity in overall biliary complications rates (P = 0.37; I2 = 8%), and pooled results of a fixed-effect model revealed that biliary complications occurred more commonly in SLT recipients (OR = 1.66; 95% CI = 1.29-2.15; P < 0.001). Bile leak rates were reported in 8 studies. Among them, 4 studies showed comparable bile leak rates between SLT and WLT groups, but other studies suggested higher bile leak rates associated with SLT. No significant heterogeneity was shown among theses 8 studies (P = 0.27; I2 = 20%), and a fixed-effect model showed that SLT recipients had higher bile leak rates than WLT recipients (OR = 4.30; 95% CI = 2.97-6.23; P < 0.001). Biliary stricture rates were reported in 6 studies, with all of them showing no significant difference between SLT and WLT groups. No heterogeneity was found among these 6 studies (P = 0.62; I2 = 0%). Pooled data using a fixed-effect model showed that biliary stricture rates did not significantly differ between SLT and WLT recipients (OR = 0.64; 95% CI = 0.39-1.05; P = 0.08). Details of the meta-analyses for biliary complications are summarized in Fig. 4.
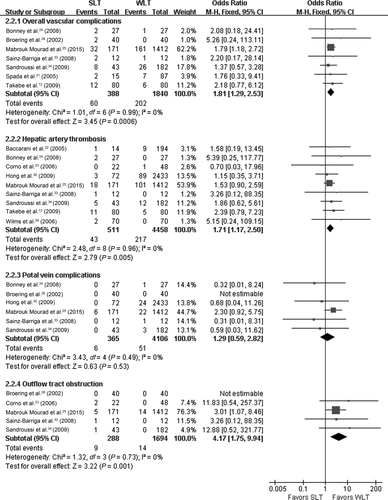
Vascular Complications
Overall vascular complication rates were reported in 7 studies. Six of these studies showed comparable results between the SLT and WLT groups, whereas 1 study reported higher vascular complication rates in the SLT group. The results of the 7 studies showed no significant heterogeneity (P = 0.99; I2 = 0%). Pooled data with a fixed-effect model suggested higher vascular complication rates associated with SLT versus WLT (OR = 1.81; 95% CI = 1.29-2.53; P < 0.001). HAT was reported in 9 studies, and all of them suggested that no significant difference existed between SLT and WLT recipients. Homogeneity among these studies was satisfactory (P = 0.96; I2 = 0%). A fixed-effect model showed that HAT was more common in SLT recipients than in WLT recipients (OR = 1.71; 95% CI = 1.17-2.50; P = 0.005). PVC rates were reported in 6 studies, and all of them showed similar results between SLT and WLT groups. No significant heterogeneity was observed among these studies (P = 0.49; I2 = 0%). According to pooled data using a fixed-effect model, PVC rates were found to be equivalent between SLT and WLT recipients (OR = 1.29; 95% CI = 0.59-2.82; P = 0.53). OTO rates were reported in 5 studies. In 4 of these studies, OTO rates did not significantly differ between SLT and WLT recipients, whereas 1 study showed a higher OTO rate in SLT recipients. There was no significant heterogeneity among these studies (P = 0.73; I2 = 0%). A fixed-effect model showed that OTO occurred more frequently in SLT recipients (OR = 4.17; 95% CI = 1.75-9.94; P = 0.001). Figure 5 shows the details of the meta-analyses for vascular complications.
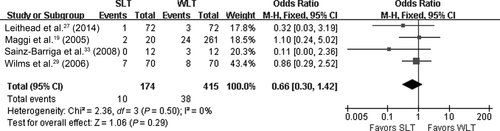
Postoperative Bleeding Requiring Surgical Treatments
Four studies compared PBRST rates between SLT and WLT recipients, with all of them showing no significant difference between the 2 groups of patients. Satisfactory homogeneity among these studies was observed (P = 0.50; I2 = 0%). Pooled results using a fixed-effect model showed that the PBRST rate in SLT recipients was similar to that in WLT recipients (OR = 0.66; 95% CI = 0.30-1.42; P = 0.29; Fig. 6).
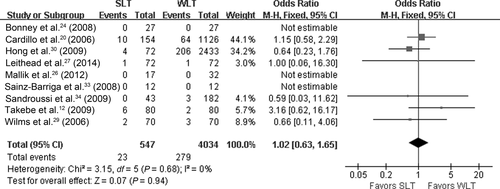
Primary Nonfunction
Nine studies provided data on PNF, and all of these studies suggested similar results between SLT and WLT recipients. No significant heterogeneity was found among the 9 studies (P = 0.68; I2 = 0%). A fixed-effect model was used to combine the data, and pooled results revealed that PNF rates were equivalent between SLT and WLT recipients (OR = 1.02; 95% CI = 0.63-1.65; P = 0.94; Fig. 7).
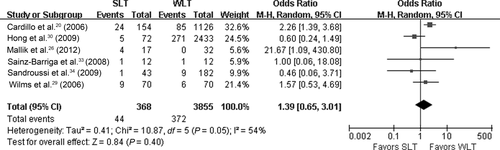
Retransplantation
Retransplantation rates were reported in 6 studies. Four studies showed no significant difference observed between SLT and WLT recipients, whereas retransplantation rates were higher in SLT recipients compared with WLT recipients in 2 studies. The heterogeneity test indicated that there was significant heterogeneity among the 6 studies (P = 0.05; I2 = 54%). Pooled results using a random-effect model were found to be comparable between SLT and WLT recipients (OR = 1.39; 95% CI = 0.65-3.01; P = 0.40; Fig. 8).
Subgroup Analysis
In the subgroup analyses for PS and GS, all syntheses were stratified according to 4 important factors that might have an influence on survival outcomes: dominating split technique (in situ or ex situ), matching of donor ages (yes or no), matching of urgent status (yes or no), and number of SLT recipients (<50 or ≥50). In subgroup analyses for PS, results in subgroups were all consistent with the main results (Table 3). However, stratifications of GS outcomes revealed some inconformity with the overall outcomes (Table 4). When we stratified studies according to whether urgent status was matched between SLT and WLT recipients, the 3-year GS rate in SLT recipients turned out to be significantly lower than that in WLT recipients within the subgroup consisting of studies matched with urgent status. Meanwhile, the 1-year GS rate was slightly lower in the former than in the latter within this subgroup.
| Outcomes and Subgroup | Studies (n) | Effect Estimate (95% CI) | P Value | Heterogeneity |
|---|---|---|---|---|
| 3-month PS | ||||
| In situ dominating | 1 | 1.62 (0.13-13.77) | 0.66 | NA |
| Ex situ dominating | 2 | 0.90 (0.37-2.20) | 0.82 | I2 = 40%; P = 0.20 |
| Donor age matched | 2 | 0.90 (0.37-2.20) | 0.82 | I2 = 40%; P = 0.20 |
| Donor age mismatched | 1 | 1.62 (0.19-13.77) | 0.66 | NA |
| Urgent status matched | 3 | 0.99 (0.44-2.24) | 0.99 | I2 = 0%; P = 0.37 |
| Urgent status mismatched | 0 | NA | NA | NA |
| SLT recipients <50 | 2 | 2.52 (0.43-14.82) | 0.31 | I2 = 0%; P = 0.50 |
| SLT recipients ≥50 | 1 | 0.69 (0.26-1.84) | 0.46 | NA |
| Overall | 3 | 0.99 (0.44-2.24) | 0.99 | I2 = 0%; P = 0.37 |
| 1-year PS | ||||
| In situ dominating | 4 | 1.03 (0.60-1.77) | 0.92 | I2 = 16%; P = 0.31 |
| Ex situ dominating | 2 | 0.77 (0.52-1.13) | 0.18 | I2 = 0%; P = 0.70 |
| Donor age matched | 2 | 0.59 (0.28-1.21) | 0.15 | I2 = 0%; P = 0.71 |
| Donor age mismatched | 3 | 0.94 (0.62-1.40) | 0.75 | I2 = 31%; P = 0.24 |
| Urgent status matched | 5 | 0.84 (0.59-1.18) | 0.31 | I2 = 0%; P = 0.42 |
| Urgent status mismatched | 0 | NA | NA | NA |
| SLT recipients <50 | 3 | 1.18 (0.52-2.67) | 0.69 | I2 = 44%; P = 0.17 |
| SLT recipients ≥50 | 3 | 0.80 (0.57-1.12) | 0.20 | I2 = 0%; P = 0.84 |
| Overall | 6 | 0.85 (0.62-1.16) | 0.31 | 0%; P = 0.55 |
| 3-year PS | ||||
| In situ dominating | 3 | 1.13 (0.54-2.37) | 0.74 | I2 = 69%; P = 0.04 |
| Ex situ dominating | 2 | 0.91 (0.62-1.34) | 0.64 | I2 = 0%; P = 0.55 |
| Donor age matched | 1 | 0.61 (0.15-2.46) | 0.49 | NA |
| Donor age mismatched | 3 | 0.93 (0.56-1.55) | 0.79 | I2 = 62%; P = 0.07 |
| Urgent status matched | 3 | 0.79 (0.60-1.03) | 0.09 | I2 = 0%; P = 0.45 |
| Urgent status mismatched | 1 | 2.74 (0.80-9.41) | 0.11 | NA |
| SLT recipients <50 | 2 | 1.34 (0.30-5.89) | 0.70 | I2 = 61%; P = 0.11 |
| SLT recipients ≥50 | 3 | 0.86 (0.66-1.11) | 0.25 | I2 = 38%; P = 0.20 |
| Overall | 5 | 0.91 (0.71-1.16) | 0.44 | I2 = 42%; P = 0.14 |
| 5-year PS | ||||
| In situ dominating | 1 | 2.44 (0.27-22.25) | 0.43 | NA |
| Ex situ dominating | 4 | 1.04 (0.76-1.42) | 0.81 | I2 = 0%; P = 0.68 |
| Donor age matched | 4 | 1.32 (0.78-2.25) | 0.30 | I2 = 0%; P = 0.77 |
| Donor age mismatched | 1 | 0.95 (0.65-1.38) | 0.78 | NA |
| Urgent status matched | 5 | 1.06 (0.78-1.44) | 0.71 | I2 = 0%; P = 0.72 |
| Urgent status mismatched | 0 | NA | NA | NA |
| SLT recipients <50 | 2 | 1.21 (0.30-4.81) | 0.79 | I2 = 0%; P = 0.35 |
| SLT recipients ≥50 | 3 | 1.05 (0.77-1.44) | 0.75 | I2 = 0%; P = 0.54 |
| Overall | 5 | 1.06 (0.78-1.44) | 0.71 | I2 = 0%; P = 0.72 |
| Outcomes and Subgroup | Studies (n) | Effect Estimate (95% CI) | P Value | Heterogeneity |
|---|---|---|---|---|
| 3-month GS | ||||
| In situ dominating | 1 | 1.82 (0.22-15.35) | 0.58 | NA |
| Ex situ dominating | 1 | 0.58 (0.25-1.35) | 0.21 | NA |
| Donor age matched | 1 | 0.58 (0.25-1.35) | 0.21 | NA |
| Donor age mismatched | 1 | 1.82 (0.22-15.35) | 0.58 | NA |
| Urgent status matched | 2 | 0.70 (0.33-1.49) | 0.35 | I2 = 0%; P = 0.33 |
| Urgent status mismatched | 0 | NA | NA | NA |
| SLT recipients <50 | 1 | 1.82 (0.22-15.35) | 0.58 | NA |
| SLT recipients ≥50 | 1 | 0.58 (0.25-1.35) | 0.21 | NA |
| Overall | 2 | 0.68 (0.31-1.49) | 0.33 | I2 = 0%; P = 0.33 |
| 1-year GS | ||||
| In situ dominating | 6 | 0.99 (0.81-1.21) | 0.95 | I2 = 0%; P = 0.92 |
| Ex situ dominating | 2 | 0.69 (0.49-0.98) | 0.04 | I2 = 12%; P = 0.29 |
| Donor age matched | 2 | 0.59 (0.32-1.09) | 0.09 | I2 = 0%; P = 0.36 |
| Donor age mismatched | 6 | 0.95 (0.79-1.13) | 0.56 | I2 = 0%; P = 0.75 |
| Urgent status matched | 5 | 0.78 (0.57-1.06) | 0.11 | I2 = 0%; P = 0.44 |
| Urgent status mismatched | 2 | 0.98 (0.79-1.21) | 0.86 | I2 = 0%; P = 0.82 |
| SLT recipients <50 | 5 | 1.11 (0.65-1.88) | 0.71 | I2 = 0%; P = 0.86 |
| SLT recipients ≥50 | 3 | 0.89 (0.74-1.07) | 0.21 | I2 = 46%; P = 0.16 |
| Overall | 8 | 0.91 (0.76-1.08) | 0.27 | I2 = 0%; P = 0.61 |
| 3-year GS | ||||
| In situ dominating | 3 | 0.90 (0.60-1.35) | 0.61 | I2 = 67%; P = 0.05 |
| Ex situ dominating | 3 | 0.48 (0.15-1.54) | 0.22 | I2 = 52%; P = 0.12 |
| Donor age matched | 1 | 0.31 (0.03-3.16) | 0.32 | NA |
| Donor age mismatched | 5 | 0.85 (0.62-1.16) | 0.31 | I2 = 58%; P = 0.05 |
| Urgent status matched | 4 | 0.72 (0.56-0.93) | 0.01 | I2 = 39%; P = 0.18 |
| Urgent status mismatched | 2 | 1.19 (0.58-2.43) | 0.63 | I2 = 57%; P = 0.13 |
| SLT recipients <50 | 3 | 0.55 (0.09-3.31) | 0.51 | I2 = 72%; P = 0.03 |
| SLT recipients ≥50 | 3 | 0.88 (0.75-1.02) | 0.09 | I2 = 37%; P = 0.20 |
| Overall | 6 | 0.84 (0.62-1.13) | 0.25 | I2 = 52%; P = 0.07 |
| 5-year GS | ||||
| In situ dominating | 4 | 0.99 (0.84-1.17) | 0.91 | I2 = 15%; P = 0.32 |
| Ex situ dominating | 4 | 0.99 (0.74-1.31) | 0.92 | I2 = 0%; P = 0.41 |
| Donor age matched | 4 | 1.22 (0.77-1.94) | 0.39 | I2 = 0%; P = 0.41 |
| Donor age mismatched | 4 | 0.97 (0.83-1.13) | 0.66 | I2 = 0%; P = 0.45 |
| Urgent status matched | 5 | 1.01 (0.76-1.34) | 0.94 | I2 = 0%; P = 0.43 |
| Urgent status mismatched | 2 | 1.19 (0.59-2.40) | 0.62 | I2 = 56%; P = 0.13 |
| SLT recipients <50 | 4 | 1.62 (0.84-3.12) | 0.15 | I2 = 0%; P = 0.65 |
| SLT recipients ≥50 | 4 | 0.96 (0.83-1.12) | 0.60 | I2 = 0%; P = 0.43 |
| Overall | 8 | 0.98 (0.85-1.14) | 0.82 | I2 = 0%; P = 0.50 |
Subgroup analyses were also performed for overall biliary complications and overall vascular complications to evaluate the robustness of the results obtained, and for retransplantations to explore the heterogeneity among studies (Table 5). Interestingly, we found that biliary complications or vascular complications rates only increased in ex situ SLT recipients, but they did not differ between in situ SLT and WLT recipients. Besides, heterogeneity in retransplantation almost disappeared when the synthesis was stratified according to whether SLT recipients matched with WLT recipients in terms of urgent status. In the subgroup with urgent status matched, SLT was associated with significantly higher retransplantation rates than WLT.
| Outcomes and Subgroup | Studies (n) | Effect Estimate (95% CI) | P Value | Heterogeneity |
|---|---|---|---|---|
| Overall Biliary Complications | ||||
| In situ dominating | 6 | 1.18 (0.77-1.82) | 0.45 | I2 = 12%, P = 0.34 |
| Ex situ dominating | 4 | 2.05 (1.48-2.83) | <0.001 | I2 = 0%, P = 0.75 |
| Overall | 10 | 1.66 (1.29-2.15) | <0.001 | I2 = 8%, P = 0.37 |
| Overall Vascular Complications | ||||
| In situ dominating | 3 | 1.61 (0.78-3.36) | 0.20 | I2 = 0%, P = 0.70 |
| Ex situ dominating | 4 | 1.86 (1.28-2.72) | 0.001 | I2 = 0%, P = 0.99 |
| Overall | 7 | 1.81 (1.29-2.53) | <0.001 | I2 = 0%, P = 0.99 |
| Retransplantation | ||||
| Urgent status matched | 4 | 2.28 (1.48-3.51) | <0.001 | I2 = 0%, P = 0.40 |
| Urgent status mismatched | 1 | 0.46 (0.06-3.71) | 0.46 | NA |
| Overall | 6 | 1.39 (0.65-3.01) | 0.40 | I2 = 54%, P = 0.05 |
Sensitivity Analysis and Publication Bias Assessment
Sensitivity analyses were conducted for all outcome data, and the exclusion of a single study from the meta-analysis did not significantly alter the overall findings. In funnel plots (not shown), no points fell outside the 95% CI limits for all outcomes. However, the funnel plots for the 1-year PS, the 1-year GS, and PVCs indicated an asymmetry, which suggested that negative studies might be less reported. For other outcomes, publication bias was not detected.
DISCUSSION
On the basis of US national data from 1998 to 2002, split grafts were identified as an independent predictor of increased graft failure for both adult and pediatric recipients,10 and these organs were therefore viewed as suboptimal or “marginal.”26 However, it is noteworthy that the sickest transplant candidates were more inclined to receive split grafts under the MELD-based allocation system in the United States, and the graft size was not always well matched with the recipient size, which led to unfavorable outcomes in SLT recipients.30 Concerns for an increased risk of graft loss to adult recipients have discouraged the widespread adoption of SLT. Proportions of SLT performed in the United States and in Europe were only 1.4% and 6.4% of total numbers of cadaveric LTs.35, 36 In north Italy, a multicenter SLT network program has been launched within the North Italian Transplant program (NITp) since November 1997.20, 37, 38 The NITp data reported the largest SLT series in Europe, which accounted for 22% of all cadaveric LTs in the NITp area.20 Despite such a trust in split liver procedures, NITp centers achieved encouraging outcomes in right lobe SLT recipients.38
Our present study demonstrated that PS rates in adult right lobe SLT recipients were comparable with those in WLT recipients, which could be regarded with a high degree of certainty under the validation of subgroup analyses and sensitivity analyses. Similar results were also obtained in GS rates if we did not stratify studies according to whether SLT recipients matched with WLT recipients in terms of urgent status. However, when only studies matched with urgent status were included for a subgroup analysis, the risk of retransplantations significantly increased in SLT recipients, and GS rates decreased in SLT recipients. These data indicated that right lobe split liver grafts were associated with a higher risk of graft loss than did full-size grafts if seriously ill patients were not selected with partiality for WLT. Here, it should be noted in Fig. 3 that the study by Lee et al.32 carried a high weight of 56.7%-61.1% in the synthesis for GS, and nonadjusted GS rates from their study were included in the current meta-analysis. Although our sensitivity analysis showed that removal of the study by Lee et al. did not significantly alter the pooled results (1-year GS, P = 0.12; 3-year GS, P = 0.31; 5-year GS, P = 0.63), the disparity between the SLT group and the WLT group in terms of patient and donor characteristics might be a limitation in the meta-analysis for GS.
Biliary and vascular complications remain major obstacles for development of LT to date. Before this meta-analysis, whether SLTs were associated with elevated incidences of these complications remains controversial. Most published studies reported negative results when comparing SLT and WLT in terms of biliary or vascular complications. However, the trend of significance could be amplified in the meta-analysis with all published data combined in 1 synthesis. Our meta-analysis showed that SLT recipients suffered significantly higher risks of biliary and vascular complications, which provided us with a more definite understanding on this issue. Analyses for specific complications further revealed that bile leaks, HAT, and OTO rather than biliary stricture and PV complications tended to be more in SLT recipients. The increased bile leaks for SLT were probably attributed to bile leakages from the transected surface.12, 25 As for vascular complications, splitting techniques leaving hilar structures with the left graft incurred an added risk of vascular complications to the right lobe SLT recipients.20 On the other hand, multiple hepatic arteries might be identified in 1 splitting graft, which exposed patients to a higher risk of HAT.25 Although HAT might lead to an increased risk of graft loss after LT,39 biliary leaks and OTO were not lethal events in most cases because they usually could be successfully controlled with endoscopic or radiological interventions.40 Besides, liver grafts from younger and more hemodynamically stable donors were more commonly used for SLT recipients in most studies. The relatively inferior donor quality in the WLT group impaired its survival outcomes even though this group of patients experienced less biliary and vascular complications than SLT recipients. In this setting, the lack of significant difference between WLT and SLT in terms of GS is not surprising.
In contrast to in situ splitting, the ex situ dissection caused greater ischemia/reperfusion injury not only by prolonging the CIT, but also by potentially exposing the graft to additional warm ischemia via manipulation.11 Moreover, identification of some vital structures may be difficult in pale bloodless grafts during ex situ procedures. The in situ splitting technique was conceived from graft procurements from a living donor and was first reported by Rogiers et al.41 Despite prolonged splitting time and the inconvenience for graft procurements, this innovation facilitates a more precise anatomical division and improves the quality of liver grafts through greatly shortening the CIT. These factors may indicate a potential advantage for in situ splitting, but different results were reported regarding the outcomes between in situ and ex vivo splitting techniques.9, 41-43 Notably, subgroup analyses of this meta-analysis revealed that risks of increased biliary and vascular complications were only seen with the use of ex situ SLT rather than the in situ procedure, but splitting methods seemed to exert minor impacts on PS or GS rates after SLT.
In the present study, we set strict criteria for the study inclusion to minimize heterogeneity among studies. Accordingly, 14 of the 18 outcomes got excellent homogeneity (I2 < 10%). We excluded full-right-full-left SLT for 2 adult recipients from our meta-analysis because this procedure could not achieve comparable outcomes with trisegment right SLT on the basis of the NITp data.37, 38 Additionally, full-right-full-left SLT is characterized by a significantly larger transection plane, central dissection, and 2 small liver grafts,44 which renders it inappropriate to be analyzed together with the conventional SLT. However, this study had several underlying limitations. We did not set a strict limit on the etiologies of liver diseases, and definitions of postoperative complications might not be uniform across different studies. Besides, all the included studies were based on retrospective cohorts, in which the selection of controls and outcome assessments could not be accurately performed.
In conclusion, adult right lobe SLT does not have significant inferiority in terms of the PS and GS compared with WLT. If seriously ill patients are not selected with partiality for WLT, retransplantations will occur more commonly in right lobe SLT recipients. The ex vivo splitting technique causes higher rates of biliary complications and vascular complications than WLT. However, SLT could still provide more aggregate years of life than WLT because it allows effective expansion of the donor organ pool.