Prognostic factors affecting survival after recurrence in adult living donor liver transplantation for hepatocellular carcinoma
Abstract
Liver transplantation is regarded as an effective treatment for early hepatocellular carcinoma (HCC). However, some patients experience recurrence and subsequently rapid progression of the disease. We investigated prognostic factors affecting survival after recurrence in patients who underwent adult living donor liver transplantation (LDLT) for HCC. From October 1992 to December 2005, 138 adult patients underwent LDLT for HCC. Among these, 28 patients (20.3%) who suffered recurrence were retrospectively reviewed. Univariate and multivariate analyses were performed to analyze factors affecting survival after recurrence. The median time to recurrence was 7.9 months. The median survival time after recurrence was 11.7 months, and the 1- and 3-year survival rates after recurrence were 52.8% and 15.8%, respectively. Initially, 7 patients (25%) showed multiorgan involvement; however, in the follow-up, 21 patients (75%) had multiorgan involvement. On univariate analysis, a pretransplant alpha-fetoprotein level >1000 ng/mL, major vascular invasion, a poorly differentiated tumor, a time to recurrence ≤6 months, unresectable disease, and bony metastases were related to shorter survival after recurrence. The independent prognostic factors by multivariate analysis were major vascular invasion [hazard ratio (HR) = 7.6], a poorly differentiated tumor (HR = 4.3), unresectable disease (HR = 10.4), and bony metastases (HR = 3.2). Two patients survived more than 36 months. One of them underwent retransplantation and survived for 45 months without additional recurrences. In conclusion, after transplantation, recurrent HCC has a tendency to involve multiple organs, and the prognosis is very poor. However, some patients have a good prognosis, and the appropriate treatment can prolong their survival. If the recurrent lesion is locally controllable, surgical resection should be considered. Liver Transpl 16:678-684, 2010. © 2010 AASLD.
The early results of liver transplantation (LT) in patients with advanced hepatocellular carcinoma (HCC) were poor because of frequent tumor recurrence.1-3 Since the introduction of the Milan criteria by Mazzaferro and colleagues in 1996,4 the survival outcome has improved. Now, LT is regarded as the best treatment modality for patients with early HCC. However, 8% to 11% of patients still experience recurrence, even though they meet the favorable selection criteria.4, 5 The patients who experience recurrence after LT show rapid progression of recurrent disease and have a very poor prognosis because the rate of progression of recurrent HCC is more rapid after transplantation than after hepatic resection.6, 7 However, some patients have a good prognosis if they are appropriately treated after the recurrence. Hence, it is important to predict not only who can experience recurrence but also who can survive longer after recurrence. Therefore, in the present study, we investigated prognostic factors affecting survival after recurrence in patients who underwent LT for HCC.
Abbreviations:
18F-FDG PET, 18-fluoro-2-deoxy-D-glucose positron emission tomography; AFP, alpha-fetoprotein; CI, confidential interval; CNI, calcineurin inhibitor; CsA, cyclosporine A; DDLT, deceased donor liver transplantation; FK, tacrolimus; HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; HR, hazard ratio; LDLT, living donor liver transplantation; LRT, locoregional therapy; LT, liver transplantation; MVI, major vascular invasion; NBNC, non-HBV and non-HCV; PIVKA-II, protein-induced by vitamin K absence or antagonist II; re-LT, liver retransplantation; TACE, transarterial chemoembolization; UCSF, University of California, San Francisco; VI, vascular invasion.
PATIENTS AND METHODS
From February 1999 to December 2005, 322 consecutive adult patients underwent living donor liver transplantation (LDLT) in our institution. One hundred thirty-eight patients (42.9%) had HCC on pathology. Among these, 28 patients (20.3%) who experienced recurrence were retrospectively reviewed. The median follow-up period was 20.1 months (range = 2.9-88 months).
Pretransplantation Patient Selection
All candidates for transplantation were checked by computed tomography, enhanced magnetic resonance imaging, and 18-fluoro-2-deoxy-D-glucose positron emission tomography (18F-FDG PET). Tumor markers, such as alpha-fetoprotein (AFP) and protein-induced by vitamin K absence or antagonist II (PIVKA-II), were also assessed. PIVKA-II has been routinely checked since 2005. On the basis of imaging studies, patients who met the Milan criteria were selected for transplantation. If patients did not meet the Milan criteria but had neither major vascular invasion nor extrahepatic malignancy and strongly desired LDLT, we performed transplantation. LDLT was performed within 1 month after the pretransplant workup. No one received any treatment for downstaging of HCC before transplantation.
Posttransplantation Management and Follow-Up
Immunosuppressive therapy after LT consisted of cyclosporine (n = 13, 46.4%) or tacrolimus (n = 15, 53.6%) in combination with corticosteroids. Mycophenolate mofetil (n = 4, 14.3%) was used in cases of toxicity from calcineurin inhibitors or renal impairment. The corticosteroid was tapered to discontinuation by 6 months after LT. We did not reduce the dose of the immunosuppressant after recurrence. Six patients changed from a calcineurin inhibitor to sirolimus after recurrence.
The prophylaxis for hepatitis B virus recurrence after LT consisted of lamivudine and hepatitis B immunoglobulin. All patients were followed up every 1 or 2 weeks for 2 postoperative months and every 3 to 6 weeks thereafter. The serum level of AFP was measured during every visit. Abdominal computed tomography or magnetic resonance imaging was performed every 3 months for the first postoperative year and then every 6 months and in cases of increasing AFP levels without abnormal liver function. If an abdominal image did not reveal a recurrent lesion despite suspicion of recurrence, bone scanning, chest computed tomography, and 18F-FDG PET were used. No adjuvant chemotherapy was administered to any patient after transplantation.
Management of Recurrent Lesions
All hepatic recurrences were initially treated with transarterial chemoembolization (TACE). The subsequent treatment depended on whether the intrahepatic lesion had progressed. Patients with multiple intrahepatic recurrences remained on TACE. Treatment for locally controllable lesions was dependent on their locations. If the lesion was peripherally located, we considered surgical resection. If the lesion was deep-seated or a new biliary anastomosis was needed for curative resection, we considered local ablation therapy. Extrahepatic recurrences were treated with chemotherapy. In addition, resectable lesions were surgically removed. For bony or peritoneal fixed lesions that could be targets for radiotherapy, radiotherapy was performed.
Statistical Analysis
The following factors were analyzed for comparison between patients with recurrence and patients without recurrence: age, sex, cause of the underlying liver disease, pretransplant AFP, positivity on 18F-FDG PET, pretransplant treatment (yes/no), radiological Milan criteria (within/beyond), pathological University of California, San Francisco (UCSF) criteria (within/beyond), maximal size of the tumor, number of tumors, major vessel invasion (yes/no), minor vessel invasion (yes/no), intrahepatic metastasis (yes/no), serosal invasion (yes/no), and differentiation of the tumor (good and moderate/poor). Other factors were analyzed as predictors of survival after recurrence: type of calcineurin inhibitor (tacrolimus/cyclosporine), change to sirolimus (yes/no), time of recurrence (≤6/>6 months), resection of the recurrent lesion (yes/no), hepatic recurrence (yes/no), pulmonary metastases (yes/no), and bony metastases (yes/no).
Categorical variables were compared with the chi-square test or Fisher's exact test when indicated. Continuous variables were expressed as means and standard deviations and compared with the Student t test. A probability curve of survival after recurrence was calculated according to the Kaplan-Meier method and compared with the log-rank test. After univariate analysis of the factors affecting survival after recurrence, only variables that were determined to be statistically significant were used in the subsequent multivariate analysis using Cox's proportional hazards model. A P value <0.05 was considered to indicate statistical significance. Statistical analysis was conducted with SPSS 17.0.
RESULTS
Characteristics of the Patients
The mean age was 55.6 ± 6.8 years (range = 43-66 years). There were 24 men (85.7%) and 4 women (14.3%). All patients had a history of hepatitis B virus infection. Among these, 27 patients had hepatitis B surface antigen at transplantation. One patient did not have hepatitis B surface antigen but had anti-hepatitis B core immunoglobulin G antibody. HCC was visible on 18F-FDG PET in 16 patients who experienced recurrence. Twenty-three patients (82.1%) received treatment for HCC before LDLT. TACE was the most common treatment. Six patients (21.4%) had undergone partial hepatic resection for HCC before LT. Eight patients (28.6%) met the radiological Milan criteria by pathology, and 11 patients (39.3%) met the pathological UCSF criteria.
Between patients with recurrence and patients without recurrence, there were significant differences in age, pretransplant AFP, positivity of 18F-FDG PET, pretransplant treatment, Milan and UCSF criteria, maximal tumor size, number of tumors, macrovessel and microvessel invasion, intrahepatic metastases, hepatic capsular invasion, and tumor differentiation (Table 1).
| Variable | Category | Recurrence (n = 28) | No Recurrence (n = 110) | P Value |
|---|---|---|---|---|
| Age (years) | Mean (range) | 55.6 (43-66) | 51.4 (32-77) | 0.009 |
| Sex | Male:female | 24:4 | 84:26 | 0.284 |
| Underlying liver disease | HBV | 28 (100%) | 98 (89.1%) | 0.094 |
| HCV | 0 | 8 (7.3%) | ||
| HBV + HCV | 0 | 1 (0.9%) | ||
| NBNC | 0 | 3 (2.7%) | ||
| Pretransplant AFP (ng/mL) | Mean (range) | 2968 (7-20,000) | 85 (3-1460) | 0.01 |
| >1000 | 10 (35.7%) | <0.001 | ||
| 18F-FDG PET | Positive | 16/22 (72.7%) | 8/72 (11.1%) | <0.001 |
| Pretransplant treatment | No treatment | 5 (17.9%) | 30/105 (28.6%) | 0.026 |
| TACE only | 14 (50%) | 50/105 (57.1%) | ||
| LRT only | 1 (3.6%) | 7/105 (6.7%) | ||
| Surgery only | 2 (7.1%) | 1/105 (1.0%) | ||
| TACE + LRT | 1 (3.6%) | 13/105 (12.4%) | ||
| TACE + surgery | 3 (10.7%) | 4/105 (3.8%) | ||
| TACE + LRT + surgery | 2 (7.1%) | 0 | ||
| Radiological Milan criteria | Exceeding | 20 (71.4%) | 18 (16.4%) | <0.001 |
| Pathological UCSF criteria | Exceeding | 17 (60.7%) | 18 (16.4%) | 0.005 |
| Maximal size (cm) | Mean (range) | 4.5 (0.8-25) | 2.9 (0.5-13) | 0.019 |
| Number of tumors | Mean (range) | 3.7 (1-20) | 1.9 (1-6) | 0.011 |
| Macrovessel invasion | Present | 3 (10.7%) | 0 | 0.001 |
| Microvessel invasion | Present | 9 (32.1%) | 9 (8.2%) | <0.001 |
| Intrahepatic metastases | Present | 7 (25%) | 6 (5.5%) | 0.002 |
| Serosal invasion | Capsular invasion | 7 (25%) | 0 | <0.001 |
| Differentiation | Good | 2 (7.1%) | 30 (27.3%) | 0.002 |
| Moderate | 6 (21.4%) | 57 (51.8%) | ||
| Poor | 20 (71.5%) | 23 (20.9%) |
Recurrence
Recurrence occurred in 28 of 138 adult LDLT cases with HCC. The median time to recurrence was 7.9 months (range = 1.8-38.2). In all patients, the serum level of AFP decreased to less than 20 ng/mL after LDLT. The AFP level of 21 patients (75%) increased to more than 20 ng/mL before the diagnosis of recurrence. Twenty-three patients (82.1%) died because of the progression of the recurrent HCC. The median survival time after recurrence was 11.7 months (range = 1.1-50.7 months). The 1- and 3-year survival rates after recurrence were 52.8% and 15.8%, respectively (Fig. 1). Initially, multiorgan recurrences appeared in 7 cases (25%). The most common site of initial recurrence was the graft liver (n = 14), which was followed by the lung (n = 10), bone (n = 8), lymph node (n = 3), peritoneum (n = 2), and adrenal gland (n = 1). Sometime after the initial recurrence, multiple organ involvement appeared in 21 cases (75%).
Survival curve after recurrence. The 1-, 2-, and 3-year survival rates were 52.8%, 15.8%, and 15.8%, respectively.
All recurrences in the graft liver were initially treated with TACE. Among these, 1 patient who had a single intrahepatic recurrent tumor with 2 peritoneal metastatic tumors underwent hepatic resection and metastatectomy. One patient underwent retransplantation for multiple recurrent tumors after TACE. The survival outcome after recurrence of those patients with hepatic recurrences seemed to be better than that of those who had extrahepatic metastases, but there was no statistical significance (1-year survival rate = 65.5% versus 30.0%, P = 0.087; Fig. 2A).
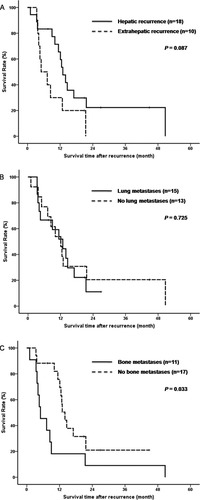
Survival curves according to the site of the initial recurrence: (A) hepatic recurrences, (B) lung metastases, and (C) bone metastases.
All pulmonary recurrences were treated with chemotherapy based on 5-fluorouracil and mitomycin C or 5-fluorouracil and cisplatin or sorafenib. One patient underwent pulmonary wedge resection 3 times. The survival outcome after recurrence did not differ whether there were pulmonary metastases or not (1-year survival rate = 51.9% versus 53.8%, P = 0.725; Fig. 2B).
Most recurrences in bone were treated with radiotherapy and/or chemotherapy. Two patients with solitary bony recurrence underwent metastatectomy. Patients with bony metastases showed significantly poorer survival outcomes than those without bony metastases (1-year survival rate = 18.2% versus 75.6%, P = 0.033; Fig. 2C).
Overall, 4 patients underwent surgical resection for recurrent lesions, including hepatic resection and retransplantation for intrahepatic recurrences, wedge resection for pulmonary metastases, and metastatectomy for bony metastases.
Prognostic Factors Affecting Survival After Recurrence
On univariate analysis (see Table 2), a pre-LT AFP level >1000 ng/mL, major vascular invasion, a poorly differentiated tumor, a time to recurrence ≤6 months, unresectable disease, and the presence of bony metastases were related to poor survival after recurrence.
| Variable | Category | n | Mean (months) | 1-Year Survival Rate (%) | 3-Year Survival Rate (%) | P Value |
|---|---|---|---|---|---|---|
| Age (years) | ≤55 | 13 | 12.4 | 51.9 | 0 | 0.686 |
| >55 | 15 | 19.5 | 53.3 | 26.7 | ||
| Sex | Male | 24 | 18.5 | 57.4 | 19.9 | 0.141 |
| Female | 4 | 8.3 | 25.0 | 0 | ||
| Pre-LT AFP (ng/mL) | ≤1000 | 18 | 22.1 | 65.8 | 26.9 | 0.012 |
| >1000 | 10 | 8.2 | 30.0 | 0 | ||
| 18F-FDG PET | Positive | 16 | 11.1 | 48.6 | 0 | 0.086 |
| Negative | 6 | 27.7 | 83.3 | 50.0 | ||
| Maximum size (cm) | ≤5 | 23 | 16.9 | 60.3 | 13.9 | 0.442 |
| >5 | 5 | 9.8 | 20.0 | 20.0 | ||
| Multiplicity | Single | 11 | 16.6 | 63.6 | 12.1 | 0.677 |
| Multiple | 17 | 15.9 | 45.3 | 19.4 | ||
| Radiological Milan criteria | Within | 8 | 22.7 | 75.0 | 30.0 | 0.374 |
| Beyond | 20 | 14.3 | 45.0 | 12.5 | ||
| Pathological UCSF criteria | Within | 11 | 22.9 | 72.7 | 31.2 | 0.277 |
| Beyond | 17 | 13.8 | 41.2 | 11.8 | ||
| Major VI | Yes | 3 | 2.7 | 0 | 0 | 0.005 |
| No | 25 | 18.1 | 59.3 | 17.8 | ||
| Minor VI | Yes | 9 | 12.1 | 44.4 | 11.1 | 0.737 |
| No | 19 | 18.9 | 56.7 | 22.7 | ||
| Differentiation | Good and moderate | 16 | 21.1 | 62.5 | 22.5 | 0.025 |
| Poor | 12 | 8.5 | 40.0 | 10.0 | ||
| Intrahepatic metastasis | Yes | 7 | 20.5 | 71.4 | 28.6 | 0.413 |
| No | 21 | 14.0 | 46.4 | 8.6 | ||
| Serosal invasion | Yes | 7 | 10.8 | 42.9 | 14.3 | 0.567 |
| No | 21 | 17.2 | 56.1 | 15.3 | ||
| CNI | CsA | 13 | 17.5 | 53.8 | 15.4 | 0.703 |
| FK | 15 | 12.4 | 51.9 | 22.2 | ||
| Change to sirolimus | Yes | 6 | 23.8 | 66.7 | 33.3 | 0.320 |
| No | 22 | 13.4 | 49.0 | 8.2 | ||
| Time of recurrence (months) | ≤6 | 13 | 8.8 | 38.5 | 0 | 0.007 |
| >6 | 15 | 24.1 | 66.0 | 30.8 | ||
| Unresectable disease | No | 4 | 41.0 | 100 | 75.0 | 0.025 |
| Yes | 24 | 11.2 | 44.6 | 6.0 | ||
| Hepatic recurrence | Yes | 18 | 20.1 | 65.5 | 22.3 | 0.087 |
| No | 10 | 9.2 | 30.0 | 0 | ||
| Pulmonary metastases | Yes | 15 | 12.5 | 51.9 | 9.7 | 0.725 |
| No | 13 | 18.2 | 53.8 | 20.5 | ||
| Bony metastases | Yes | 11 | 10.8 | 18.2 | 9.1 | 0.033 |
| No | 17 | 19.5 | 75.6 | 21.0 |
The independent prognostic factors according to Cox's proportional hazards regression for multivariate analysis were major vascular invasion [hazard ratio (HR) = 7.6, P = 0.01], a poorly differentiated tumor (HR = 4.3, P = 0.006), unresectable disease (HR = 10.4, P = 0.026), and the presence of bony metastases (HR = 3.2, P = 0.02; see Table 3).
| Variable | HR | 95% CI | P Value |
|---|---|---|---|
| Major vascular invasion | 7.6 | 1.6-35.3 | 0.01 |
| Poorly differentiated tumor | 4.3 | 1.5-12.3 | 0.006 |
| Unresectable disease | 10.4 | 1.3-81.3 | 0.026 |
| Bony metastases | 3.2 | 1.2-3.2 | 0.02 |
Survivors for More Than 36 Months After Recurrences
In our cohort, 2 patients survived more than 36 months after recurrences (Table 4). In patient 1, the tumor initially recurred at the sacrum, which was followed by the cervical spine and liver. The recurrent lesions were locally controlled by surgical resections, radio frequency ablation, and percutaneous ethanol injection. Multiple bony metastases then occurred, and he died 51 months after the initial recurrence. Patient 2 experienced multiple intrahepatic recurrences 12.3 months after transplantation and underwent retransplantation after TACE. Since then, he has survived for 45 months after the initial recurrence without evidence of further recurrences.
| Patient | Initial Recurrence | Time to Recurrence | MVI | Differentiation | Treatment | Outcome |
|---|---|---|---|---|---|---|
| 1 | Bone | 40.6 months | No | Well | Surgery | Expired 51 months later after recurrences |
| 2 | Liver | 12.3 months | No | Moderate | TACE, re-LT | Alive without recurrence for 45 months |
DISCUSSION
The aim of the present study was to analyze the prognostic factors affecting survival after recurrence in patients with HCC who underwent LDLT. The rate of HCC recurrence after transplantation has ranged from 8% to 22.7% in different series. The rate of recurrence of this study (20.3%) was relatively high. This might be due to the fact that 27.5% (n = 38) of all recipients exceeded the Milan criteria and 47.4% (n = 18) of them experienced recurrence. According to previous reports, patients who underwent LDLT had a significantly higher rate of recurrence than patients who underwent deceased donor liver transplantation (DDLT).8 In our experience, the 5-year recurrence rate of patients within the Milan criteria was 11.3% with LDLT and 7.1% with DDLT (P = 0.353). The 5-year recurrence rate of patients beyond the Milan criteria was 44.8% with LDLT and 42.9% with DDLT (P = 0.782). Most patients who experienced recurrence were relatively advanced. Hence, it seemed that the selection criteria did not need to be more restrictive in LDLT.
According to previous reports, patients who experienced recurrence showed very poor survival after recurrence, such that the median survival after recurrence ranged from 7 to 9 months.6, 7 Similarly, the median survival time after recurrence in our cohort was only 11.7 months. The main reason for this poor outcome is that the progression of the disease is usually fast because of the immunosuppressed state after transplantation. Besides, it is difficult to treat recurrences because these tumors are apt to be involved in multiple organs, and if the tumor recurs in a single organ, it usually manifests multiple lesions.
In our study, major vascular invasion, tumor differentiation, resection for recurrent lesions, and the presence of bony recurrence were independent prognostic factors for survival after recurrence. Among the risk factors for recurrence, only major vascular invasion and the histological grade of the tumor were related to survival after recurrence. These findings suggest that the aggressiveness of the tumor and the effectiveness of the treatment for the recurrent lesion were important to survival after recurrence. If the recurrent disease progressed slowly and if the recurrent lesion was locally controllable, the patient's survival could be prolonged.
The graft liver, lung, and bone were common sites of recurrence. In our study, outcomes were best for intrahepatic recurrence, which was followed by pulmonary and bony recurrences. These differences also seemed to be related to the effectiveness of the treatment. Unlike extrahepatic recurrences, more treatment options, such as TACE, radio frequency ablation, and percutaneous ethanol injection therapy, could be applied to intrahepatic recurrences.
The effectiveness of chemotherapy and radiotherapy for intrahepatic and/or extrahepatic recurrences was limited. Although there is no drug or regimen that can be clearly defined as the standard for treating HCC, it was recently reported that sorafenib improved survival in advanced HCC.9, 10 We had only 2 patients who were treated with sorafenib. However, they did not continue to receive sorafenib because of severe side effects such as pancytopenia. We therefore could not evaluate the effectiveness of sorafenib in transplantation.
Most of our patients with intrahepatic recurrences were initially treated with TACE. Ko et al.11 reported that the tumor response to TACE for recurrent HCC after transplantation was the same or more favorable than the response before transplantation. Our data showed that the 1-year survival rate of patients with intrahepatic recurrences was 65.5%; however, the survival rate decreased rapidly after 1 year. The poor outcome of the mid-term periods was due to newly developed intrahepatic metastases, especially hypovascular HCCs and extrahepatic metastases.
Of the various treatment modalities, only surgical resection showed significantly better survival outcome. In the present study, however, only 4 cases (14.3%) were surgically resectable; in contrast, some authors have reported 25% to 31.6% resectability.7, 12 One of the 4 resectable patients (see Table 4, case 1) had bony recurrence, but he had favorable tumor biology. He underwent surgical treatment for recurrence and survived for 51 months after recurrence. Two of the 4 patients had poorly differentiated HCC on pathology, and they experienced recurrence in the graft liver and in the lung within 1 year after LT. They survived for 12.1 and 20.9 months after the initial recurrence, respectively, and they survived longer than patients with poorly differentiated HCC (see Table 2). On the basis of these findings, the surgical treatment of recurrence prolonged survival, and the effect of surgical resection was more remarkable in a more favorable group. Also, surgical resection reduced the tumor burden and secondary metastases from the primary recurrent lesion. One patient who underwent retransplantation (see Table 4, case 2) survived for 45 months without recurrence. These findings also suggest that surgical resection could completely eradicate recurrent HCC in some cases. Encouraged by the good outcome of retransplantation, we recently performed retransplantation for 1 more case. This patient was followed up for only 3 months after retransplantation, and no evidence of recurrence has yet been observed. It was difficult to define clear indications for retransplantation because of a lack of experience. However, we considered the following when we decided on retransplantation. First, the recurrent lesion was confined to the liver and met the Milan criteria. Second, there were no extrahepatic recurrences after at least 6 months of follow-up. Third, the histological grade of previous HCC was favorable, and the recurrent lesion was not visible on 18F-FDG PET, which was associated with the histological grade of the tumor and vascular invasion.13 Fourth, the peak level of AFP was less than 20 ng/mL, regardless of treatment during follow-up. In our institution, AFP and PIVKA-II were checked during follow-up. AFP was significantly related to recurrence,14, 15 and our results showed that AFP was related to tumor recurrence. However, PIVKA-II was not included in the analysis because the level of PIVKA-II was not checked in early cases.
Survival after recurrence after transplantation is very poor. However, select patients may experience complete eradication of the recurrent HCC. Hence, an appropriate treatment should be considered in order to prolong survival. In particular, if the recurrent lesion is locally controllable, surgical resection should be considered.