Choledochoduodenal fistula after liver transplantation
CASE REPORT
Following orthotopic liver transplantation, biliary complications represent a substantial source of short-term to medium-term morbidity in transplant recipients, with a prevalence of 6%-35%.1-4 These include biliary leakage, strictures of anastomoses, ischemic and ischemic-type biliary lesions, concrements, and others.5 Endoscopic procedures are the treatment of choice; however, surgery is often required for refractory disease.
Here, we present the case report of a liver transplant recipient with a bile leak forming a choledochoduodenal fistula, which was treated successfully by endoscopic stenting. A 67-year-old man underwent orthotopic liver transplantation for end-stage liver disease due to hepatitis C virus infection. Biliary reconstruction was performed with end-to-end choledochocholedochostomy without intraoperative complications. The patient was discharged from the hospital 16 days after transplantation.
He was readmitted 10 days later because of painless jaundice and elevation of liver function tests. Abdominal ultrasound gave no evidence for mechanical cholestasis. Histologic analysis as well as serological tests revealed hepatitis C reinfection.
However, 3 weeks later abdominal ultrasonography showed intrahepatic bile ducts being dilated up to 4 mm in diameter. Endoscopic retrograde cholangiography revealed biliary leakage at the level of the anastomosis without communication to other organs; consequently, a stent was placed within the common bile duct which resulted in timely abrogation of jaundice.
Ten weeks later, the patient presented at our institution again because of itching, jaundice, and elevated cholestatic parameters. Magnetic resonance cholangiopancreatography (MRCP) was performed, and it showed a signal-enhancing structure dorsal to the common bile duct leading to the small intestine (Fig. 1).
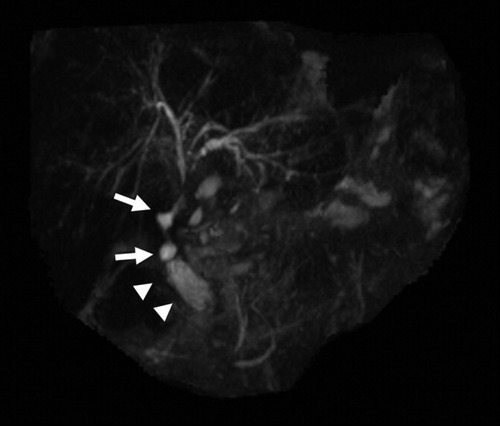
MRCP showing dorsal pearl necklace-like signal enhancement (white arrows) leading from bile duct to duodenum (arrowheads).
After endoscopic examination, absence of the biliary stent was noticed. Retrograde endoscopic cholangiography showed a pearl necklace–like contrasted fistulation originating from the bile duct anastomosis and leading to the duodenum (Fig. 2). To localize the mouth of the fistula, 0.1% methylene-blue solution was injected into the distal choledochus (Fig. 3). Remarkably, the mouth of the fistula could be localized proximal to the papilla vateri in the wall of the duodenum. Closing of the fistula was obtained by placing a 11.5-French plastic endoprosthesis into the right hepatic duct. The patient recovered from jaundice after this procedure, without further events or complications.

During ERCP contrast medium was injected via a catheter (black arrow) into the common bile duct into the region of anastomosis. Bile leakage (white arrows) is visible at the site of bile duct anastomosis with contrast flow into the bowel (white arrowheads).
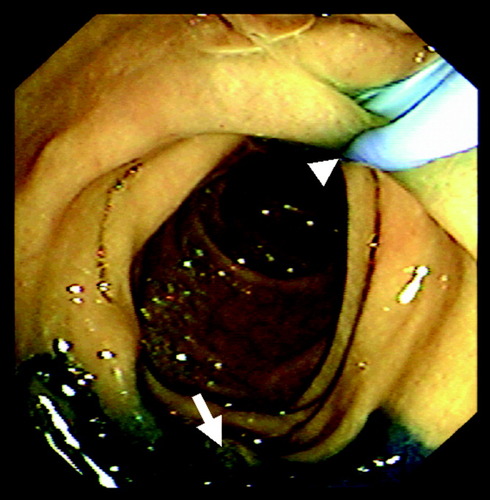
Endoscopic view of the proximal duodenum. A balloon catheter (white arrowhead) is inflated in the distal common bile duct and the endoscope is retracted into the duodenal bulb. Methylene-blue injected via the balloon catheter enters the duodenum via the fistula opening at the opposing wall (white arrow).
Abbreviation
MRCP, magnetic resonance cholangiopancreatography.
DISCUSSION
Biliary leakage is a complication usually occurring during the first few weeks after orthotopic liver transplantation. The incidence ranges from 1.6% to 19%.6, 7 In most cases, leakage occurs at the site of anastomosis; however, it may also result from other leakage sites such as from hepatic artery thrombosis or iatrogenic duct damage.8, 9 In split-liver or living related donor liver transplantation, the raw cut surface may also be the origin of a more diffuse leakage.
To our knowledge, this is the first report of an anastomotic leakage forming a choledochoduodenal fistula in a recipient after liver transplantation. Ectopic opening of the bile duct into the duodenal bulb has been described in association with recurrent duodenal ulcer and might be of congenital origin.10 Another possibility may be the retrograde formation of a fistula originating from duodenal ulcerations.11 Development of choledochoduodenal fistula has been found to be caused by tuberculosis12, 13 and gallstones.14, 15 Diagnosis is usually established by transabdominal sonography, hepatobiliary scintigraphy, MRCP, and endoscopic or percutaneous cholangiography.
Drainage of the bile duct is crucial in treatment of a biliary leakage to allow the leakage to be closed; this can be achieved by either endoscopic stenting, sphincterotomy, nasobiliary drainage, or percutaneous drainage. The optimal therapeutic regimen mainly depends on the localization of the defect and locally available techniques.
Because closure of a choledochoduodenal fistula may take several months, it was decided to treat the patient in this report by internal endoscopic stenting. However, in the case of failure or nonoptimal results of endoscopic procedures, leakages should be either surgically revised or hepaticojejunostomy be performed.