Assessment of acute pulmonary vascular reactivity in portopulmonary hypertension†
See Editorial on Page 1498
Abstract
The role of acute pulmonary vasodilator testing in portopulmonary hypertension (PoPH), a current contraindication for orthotopic liver transplantation (OLT), has not been thoroughly elucidated. The purpose of this work was to analyze the results of acute vasodilator testing with inhaled nitric oxide (NO), to compare them with intravenous epoprostenol (PGI2), and to investigate the acute effects of the oral vasodilator isosorbide-5-mononitrate (Is-5-MN), in patients with PoPH. A total of 19 patients with PoPH (male/female = 9/10) were studied. Pulmonary hemodynamic measurements were performed at baseline and during NO inhalation (40 ppm); additionally, 15 patients were tested with PGI2 (2–12 μg/kg/minute) and 8 were tested with Is-5-MN (20–40 mg). Inhaled NO reduced pulmonary artery pressure (PAP) and pulmonary vascular resistance (PVR) by 5.7% and 11.0%, respectively. PGI2 elicited greater reductions in PAP (11.8%) and PVR (−24.0%), and produced a 28% drop in systemic vascular resistance (SVR) and a 17% increase in the cardiac index (CI). Is-5-MN reduced PAP by 25.6% and PVR by 21.5%, without systemic changes. There was good agreement between the response to PGI2 and Is-5-MN: 6 patients of the whole series (32%) decreased PAP >20% from baseline, reaching a final value ≤35 mmHg, the current limit for OLT. In conclusion, acute vasodilator testing has a relevant role in PoPH, as it identifies one-third of patients able to reach a more favorable hemodynamic situation, which can be determinant for their management. For vasodilator testing, PGI2 is more suitable than NO in PoPH. Is-5-MN exerts a selective effect on pulmonary circulation in patients who had already responded to PGI2. Liver Transpl 13:1506–1514, 2007. © 2007 AASLD.
Portopulmonary hypertension (PoPH), the association of pulmonary hypertension with portal hypertension, is present in about 4% of patients candidates to orthotopic liver transplantation (OLT).1, 2 Its prognosis is worse than other forms of pulmonary arterial hypertension (PAH), death being similarly caused by hepatic or pulmonary problems.3 Currently, the presence of PoPH with a mean pulmonary artery pressure (PAP) exceeding 35 mmHg represents a relative contraindication for liver transplantation (LT),3 while a value ≥45 mmHg is an absolute contraindication; there is, however, no consensus on the way to treat it.
The treatment algorithm in idiopathic PAH is based on the response to acute vasodilator testing:4 patients showing a significant vasodilator response may benefit from treatment with Ca-channel blockers5-7 and have a favorable long-term prognosis.6, 8
In PoPH the situation is less clear. The role of acute pulmonary vasodilator testing has not been thoroughly assessed in spite of its potential interest for screening patients for OLT and developing a therapeutic strategy. As for the vasodilators to be used in the acute testing, previous studies have yielded discrepant results. Inhaled nitric oxide (NO) has shown either lack of effect9 or a minor vasodilating action.10, 11 By contrast, intravenous epoprostenol (PGI2) has shown a significant vasodilator response in 5 out of 14 tested patients.12 To what extent the discrepancy might be related to the probing agent is unknown, since they have not been tested in the same patients. On the other hand, the extent of response is a critical issue as current guidelines recommend not to perform OLT if mean PAP exceeds 35 mmHg due to increased postoperative mortality.13, 14
Furthermore, it is relevant to understand to what extent the acute response to NO or PGI2 might be predictive of the effect of an oral vasodilator. Several drugs are in fact available but may have detrimental effect on the concomitant hepatic circulation: Ca-channel blockers may increase the hepatic vein portal gradient15-17 and sildenafil can worsen portal hypertension.18, 19 The experience with endothelin receptor blockers is still limited,20, 21 although its potential hepatotoxicity may preclude its use in this group of patients.22
The aim of the present investigation was to evaluate the acute hemodynamic response to inhaled NO and intravenous PGI2 in the same patients. Based on previous experience23 we hypothesized that patients showing a significant acute pulmonary vasodilator response would also respond to oral isosorbide 5-mononitrate (Is-5-MN), which has a safer profile in portal hypertension,24, 25 and, accordingly, we have in addition investigated the acute effects of oral Is-5-MN in a subset of patients.
Abbreviations
PoPH, portopulmonary hypertension; (O)LT, (orthotopic) liver transplantation; NO, nitric oxide; PGI2, epoprostenol; Is-5-MN, isosorbide-5-mononitrate; PAP, pulmonary artery pressure; PVR, pulmonary vascular resistance; SVR, systemic vascular resistance; PAH, pulmonary arterial hypertension; CI, cardiac index.
PATIENTS AND METHODS
Patients
We analyzed the results of acute vasodilator testing in 19 patients (10 men, 9 women; age, 49.8 ± 11.7 yr) with portal hypertension, who underwent right heart catheterization for the diagnosis and staging of pulmonary hypertension. All of them had a previous echocardiogram showing increased systolic PAP (>40 mmHg) and were diagnosed of PoPH according to current criteria.3, 4 A total of 18 patients had cirrhosis and 1 congenital hepatic fibrosis. The majority of patients were in class II or III of the modified New York Heart Association classification adopted by the World Health Organization.4 The study was approved by the internal review board and all patients gave written informed consent before the study.
Procedures
All vasodilator drugs had been discontinued for at least 48 hours before the study. Right heart catheterization was performed by using a 7F triple-lumen flow-directed thermodilution catheter (Baxter, Irvine, CA) as previously reported.7 Cardiac output was determined in triplicate by the thermodilution technique (M1012A; Hewlett-Packard, Boeblingen, Germany). Cardiac index (CI), and pulmonary (PVR), and systemic vascular resistance (SVR) were computed. Arterial blood gases, pH, oxyhemoglobin saturation, and hemoglobin concentration were measured in arterial and mixed-venous blood (Ciba-Corning 800, Medfield, MA).
Acute Vasoreactivity Testing
After a duplicate set of baseline measurements, taken more than 20 minutes apart, the response to inhaled NO was studied. Patients breathed a mixture of NO (10, 20, and 40 parts per million [ppm]) in air from a Douglas bag using an unidirectional valve (Hans Rudolph, Kansas City, MO) for 20 minutes, as previously described.7, 26 Hemodynamic measurements were performed at the end of each inhalation period and the concentration of NO was increased progressively until a significant response was achieved.
At the end of NO administration a 30-minute washout period was allowed before again recording a baseline and proceeding to the following test.
PGI2 (epoprostenol, a synthetic prostacyclin; Flolan, Glaxo-Wellcome, Madrid, Spain), was administered intravenously. The infusion rate was started at 2 μg/kg/minute and increased stepwise by 2 μg/kg/minute increments every 15 minutes, up to a maximum dose of 12 μg/kg/minute. The infusion was terminated before reaching the highest rate in case a significant response had already been achieved or the patient developed severe hypotension or untoward side effects.
At the end of 30 minutes of washout and after verifying that a basal setting was regained, a subset of 8 patients underwent a third trial with Is-5-MN, given orally at the dose of 10 mg for 1 hour, then increasing to 20 and 40 mg at hourly intervals. The majority of the patients had shown vasodilator responses in the previous tests.
In any of the 3 pharmacologic trials the drug was discontinued if a positive response was reached.
Assessment of Response
Definition of positive response to the acute vasodilator challenge has varied through time. In the current consensus guidelines,4, 27, 28 the definition is based on observations made in patients with idiopathic PAH6 and differs slightly from those specific for patients with PoPH.3 Accordingly, we have evaluated our results using 2 response criteria: 1) the so-called Venice criteria (fall in mean PAP of at least 10 mmHg to ≤40 mmHg, with an increased or unchanged CI; 427, 28;and 2) the criteria proposed by the European Respiratory Society Task Force on pulmonary-hepatic vascular disorders for patients with PoPH (decrease in both PAP and PVR ≥ 20%, with no change or increase in CI.3
Statistical Analysis
All results are expressed as mean ± standard deviation or median and 95% confidence interval. Changes of hemodynamic parameters from baseline produced by each acute vasodilator trial were assessed by Wilcoxon's test. The statistical significance of mean changes obtained with NO, PGI2, and Is-5-MN were compared using a Student's t-test. Correlations between variables were assessed with the Pearson's 2-tailed test. All calculations were performed using the SPSS statistical package (SPSS Inc., Chicago, IL) and a P value <0.05 was considered significant in all cases.
RESULTS
Patients with cirrhosis taking part in the present investigation had mild to severe pulmonary hypertension. Mean PAP was 41.9 ± 13.7 mmHg (range, 25–72 mmHg; Table 1) and PVR was 576 ± 286 dyn · second·cm−5 (range, 302–1290 dyn · second · cm−5). CI was 2.91 ± 0.84 L/minute/m2 (ranging from 1.6 to 5.0 L/minute/m2), slightly increased as compared to idiopathic PAH, but still lower than that commonly seen in the hyperdynamic circulatory state of cirrhotic patients with portal hypertension. Clinically, the majority of patients had moderate to severe dyspnea (according to the New York Heart Association/World Health Organization functional scoring, 2 patients were in class I, 7 patients in class II, 7 in class III, and the remaining 3 patients in class IV).
| Gender (male/female) | 10/9 |
| Age (yr) | 52 ± 12 (17–70) |
| Etiology of cirrhosis* | |
| Viral (HBV/HCV) | 3/11 |
| Alcohol | 8 |
| HVPG (mmHg; n = 11) | 16 ± 3.1 (4–22†) |
| MELD score | 15 ± 2.5 (5–26) |
| Portosystemic shunt | |
| TIPSS | 3 |
| Surgical | 5 |
| Ascites | 5 |
| WHO functional class | |
| I-II | 9 |
| III-IV | 10 |
| Baseline hemodynamics | |
| PAP (mmHg) | 41.9 ± 13.7 (25–72) |
| PAOP (mmHg) | 7.1 ± 5.8 (0–15) |
| QT (L/minute) | 5.14 ± 1.53 (2.4–8.1) |
| CI (L/minute/m2) | 2.91 ± 0.84 (1.6–5.0) |
| SV (mL) | 73.8 ± 20.6 (55–112) |
| PAWP (mmHg) | 7.1 ± 4.5 (0–15) |
| PVR (dyn · second · cm−5) | 576 ± 286 (302–1,290) |
| RAP (mmHg) | 5.8 ± 4.7 (0–14) |
| SVR (dyn · second · cm−5) | 1,326 ± 541 (424–2,430) |
| PaO2 (mmHg) | 63 ± 16 (42–94) |
| AaPO2 (mmHg) | 38 ± 14 (13–50) |
| PvO2 (mmHg) | 37 ± 4 (28–44) |
| SvO2 (mmHg) | 73 ± 6 (54–79) |
- NOTE: Values are given as mean ± standard deviation, and range is indicated in brackets. HVPG was measured in 13 of 19 patients for diagnostic purposes and in 6 of 19 patients, catheterization was performed for both diagnostic and therapeutic intents, e.g., control of TIPSS or surgical porto-caval anastomosis. The MELD score was calculated on the UNOS website.
- Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; HVPG, hepatic vein pressure gradient; MELD, Model for End-Stage Liver Disease; TIPSS, transjugular intrahepatic portosystemic stent; PAOP, pulmonary artery occlusion pressure; QT, cardiac output; SV, stroke volume; PAWP, pulmonary artery wedge pressure; RAP, right atrial pressure; PaO2, arterial oxygen partial pressure; AaPO2, alveolar to arterial oxygen tension gradient; PvO2, partial oxygen pressure in mixed-venous blood; SvO2, oxygen saturation in mixed-venous blood; UNOS, United Network for Organ Sharing.
- * Etiology of cirrhosis was mixed (viral and alcoholic) in few cases.
- † The lowest value in the range was recorded in a patient with a TIPSS since 5 yr of age.
The whole group (n = 19) underwent NO testing. Two patients (11%) fulfilled the European Respiratory Society pulmonary-hepatic vascular disorders criteria for a positive response, but they did not reach the Venice criteria, because the decrease in PAP was >20% but less than 10 mmHg (Fig. 1). The maximal response was observed at 40 ppm of inhaled NO in all but 1 patient who showed a positive response at 20 ppm.
Individual changes in PAP (mmHg), CI (L/minute/m2), and PVR (dyn · second · cm−5) under the 3 different testing conditions: inhaled NO, intravenous PGI2, and Is-5-MN. The statistical significance of changes from the pretest values was calculated with Wilcoxon's test.
Overall, pulmonary hemodynamic changes induced by NO were of small magnitude, although statistically significant (Fig. 1; Table 2). The mean PAP decreased to 40.0 ± 15.4 mmHg (P < 0.005; median change −6%), the CI rose to 3.06 ± 0.84 L/minute/m2 (P < 0.005; median change +6%), and the PVR decreased to 520 ± 297 dyn · second · cm−5 (P < 0.01; median change −11%).
| NO (n = 19) | PGI2 (n = 15) | Is-5-MN (n = 8) | ||||
|---|---|---|---|---|---|---|
| Median | 95% confidence interval | Median | 95% confidence interval | Median | 95% confidence interval | |
| HR beats/minute (%) | −2(−2.9) | −6.4 to 1.7 (−0.1 to 0.0) | −7 (−8.3) | −18.7 to 4.7 (−29.1 to 7.2) | 0 (0) | −1.7 to 3.1 (−2.2 to 3.4) |
| CI L/minute/m2 (%) | 0.13 (5.7) | 0.07 to 0.20 (2.7 to 8.6) | 0.57 (16.8) | 0.42 to 0.93 (13.1 to 28.6) | −0.08 (−0.7) | −0.43 to 0.19 (−7.9 to 11.5) |
| PAP mmHg (%) | −2.0 (−5.7) | −3.8 to −0.2 (−10.3 to 1.0) | −4.0 (−11.8) | −8.0 to −3.4 (−19.7 to −7.5) | −11.0 (−25.6) | −15.3 to −5.9 (−34.7 to −2.1) |
| PVR dyn · second · cm−5 (%) | −73 (−11.0) | −92.6 to −21.5 (−20.4 to −4.1) | −137 (−24.0) | −200 to −113 (−30.8 to −20.8) | −91 (−21.5) | −155 to −38 (−28.7 to −8.2) |
| RAP mmHg (%) | 1 (0.1) | −0.2 to 1.1 (−3.3 to 38.5) | −1.0 (*) | −1.4 to 0.9 | 0.0 (*) | −1.4 to 1.6 |
| SAP mmHg (%) | −3.5 (−4.3) | −7.0 to 0.9 (−0.1 to 0.0) | −12.5 (−15.2) | −24.7 to −9.2 (−27.8 to −10.9) | −10.5 (−12.1) | 3.2 to 14.0 (3.6 to 15.9) |
| SVR dyn · second · cm−5 (%) | −12 (−2.3) | −135 to 41 (−28.7 to 8.6) | −393 (28.2) | −481 to −313 (−35.5 to −23.2) | 40 (3.0) | −96 to 248 (−11.9 to 16.8) |
| PVR/SVR ratio (%) | −0.05 (−18.0) | −0.15 to 0.02 (−26.9 to −4.0) | 0.01 (2.5) | −0.04to 0.08 (−9.4 to 30.1) | −0.05 (−14.5) | −0.14to −0.01 (−28.6 to −1.87) |
| PaO2 mmHg (%) | 2.6 (3.2) | 0.2 to 4.4 (0.1 to 6.2) | −1.7 (3.3) | −11.3 to 6.5 (−17.1 to 7.8) | 2.4 (3.4) | −3.7 to 23.3 (−10.8 to 47.9) |
| AaPO2 mmHg (%) | 4.9 (9.2) | 0.7 to 6.8 (2.3 to 27.2) | 3.3 (8.5) | −5.1 to 14.7 (−24.5 to 43.4) | 1.0 (2.3) | −8.8 to 5.8 (−26.2 to 14.8) |
| PvO2 mmHg (%) | 0.0 (0.0) | −0.7 to 1.2 (−2.0 to 3.7) | 0.4 (1.3) | −1.7 to 2.6 (−5.5 to 7.9) | −1.6 (−4.6) | −4.2 to 3.8 (−12.3 to 13.4) |
| SvO2 mmHg (%) | −0.9 (−1.2) | −1.8 to 0.4 (−2.7 to 0.7) | 3.4 (4.4) | −1.3 to 5.5 (−2.1 to 8.3) | −3.7 (−5.5) | −7.6 to 5.6 (−11.8 to 10.8) |
- NOTE: Results are given as the absolute and percent median difference from the pretest value and 95% confidence interval.
- Abbreviations: HR, heart rate; RAP, right atrial pressure; SAP, mean systemic arterial pressure; PaO2, arterial oxygen partial pressure; AaPO2, alveolar to arterial oxygen tension gradient; PvO2, oxygen partial pressure in mixed-venous blood; SvO2, oxygen saturation in mixed-venous blood.
- * This value could not be calculated because the right atrial pressure was 0 in several cases.
No statistically significant changes were recorded in SVR (from 1326 ± 541 to 1374 ± 478 dyn · second · cm−5), whereas the ratio between PVR and SVR (Fig. 2) decreased from 0.48 ± 0.26 at baseline to 0.41 ± 0.27 (P < 0.05) after NO inhalation, indicating selective pulmonary vasodilation.
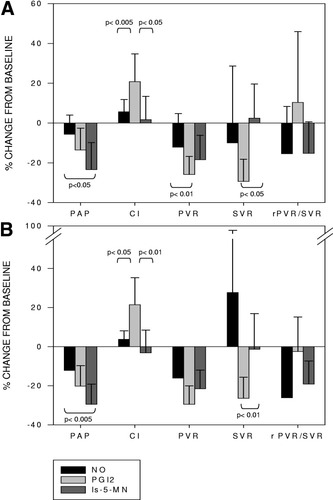
Comparison of the 3 tests of acute pulmonary vasoreactivity. In the top panel (A) the comparison is made in the whole population studied: NO (n = 19); PGI2 (n =15); and Is-5-MN (n = 8). In the bottom panel (B) the analysis is restricted to the 7 patients who underwent all 3 tests. Data are shown as mean percent change from baseline (± standard deviation [SD]). Comparisons between the vasodilatory tests were performed by Student's t-test. rPVR/SVR, ratio of PVR to SVR.
Median changes and 95% confidence intervals from the pretest values of hemodynamic and blood gas measurements are summarized in Table 2.
A total of 15 patients underwent vasodilator testing with PGI2 after an adequate washout period (30 to 40 minutes). Five patients (33%) fulfilled the European Respiratory Society pulmonary-hepatic vascular disorders criteria of a positive response and 2 of them (13%) also met the Venice criteria; the individual changes in PAP, CI, and PVR are illustrated in Figure 1. The pretest mean PAP was 43.0 ± 12.9 mmHg and decreased to 38.0 ± 12.5 (P < 0.01; median change −12%) after PGI2. The CI rose in all patients from 2.81 ± 0.59 to 3.48 ± 0.95 L/minute/m2 (P < 0.001; median change +17%). The calculated PVR and SVR dropped significantly in the whole group, from 640 ± 305 to 483 ± 248 dyn · second · cm−5 (P <0.001; median change −24%) and from 1379 ± 437 to 999 ± 394 dyn · second · cm−5 (P < 0.05; median change −28%), respectively. No changes were observed in the ratio of PVR to SVR (0.49 ± 0.27 at baseline, 0.51 ± 0.24 under PGI2). The reduction in SVR correlated with that in systemic arterial pressure (r = 0.64, P < 0.05).
The maximal decline of PAP and PVR was observed at the dose of 12 μg/kg/minute PGI2 in 12 patients; in 2 the minimum value had already been achieved at 10 μg/kg/minute, and in 1 patient PGI2 was discontinued after 8 μg/kg/minute because of a severe drop in systemic arterial pressure (PVR had decreased 11%).
After an adequate washout from PGI2 discontinuation (30-40 minutes), 8 patients underwent oral vasodilator testing with Is-5-MN. One patient responded to inhaled NO, 4 to PGI2, 1 to both NO and PGI2, and 2 were nonresponders. Individual changes in PAP, CI, and PVR induced by Is-5-MN are illustrated in Figure 1; PAP at baseline was 40.0 ± 7.1 mmHg and decreased in all patients to a mean of 29.0 ± 7.4 (P < 0.05). There was no significant change in the mean CI (from 2.83 ± 0.81 at baseline to 2.71 ± 0.82 L/minute/m2), although a single patient had a 22% decrease. PVR decreased significantly from 551 ± 184 to 454 ± 176 dyn · second·cm−5 (P < 0.05), whereas no change was observed in SVR (1,383 ± 430 to 1,307 ± 295 dyn · second · cm−5). As a consequence, the ratio of PVR to SVR also decreased significantly (P < 0.05; Table 2), indicating preferential pulmonary vasodilation. All patients reached the final dose of 40 mg Is-5-MN. After the acute administration of Is-5-MN the vasodilator response in this subset of patients could be considered significant in 6 (75%), according to the European Respiratory Society pulmonary-hepatic vascular disorders criteria, and in 5 (63%), according to the Venice criteria (Fig. 1).
No significant changes were recorded in arterial blood pH and body temperature, compared to baseline values, throughout the procedure.
We compared the extent of changes produced by NO, PGI2, and Is-5-MN by analyzing the percent difference from the pretest values (Fig. 2A). The basal recordings taken before NO, PGI2, and Is-5-MN were thoroughly overlapping. The decreases in PAP induced by PGI2 and Is-5-MN were greater than that induced by NO (Fig. 2). The changes in PAP induced by PGI2 and NO did not differ significantly (Table 2; Fig. 2A), although with PGI2 the decrease was greater and there was a greater proportion of patients reaching the criteria of PAP decrease ≥20% (33%) than with NO (11%). Interestingly, the greatest decrease in PAP was produced by Is-5-MN, although this was in a selected subset of patients.
The main effect of PGI2 was a significant decrease in SVR, yielding a corresponding rise in CI. Interestingly, the magnitude of the increase in CI induced by PGI2 correlated with the baseline value (Fig. 3). The changes in SVR and CI with NO and Is-5-MN were of small magnitude, significantly lower than with PGI2 (Table 2; Fig. 2A), and greatly overlapping. The decrease of PVR with PGI2 was more pronounced than with NO (P < 0.01), and did not differ significantly from that produced by Is-5-MN. The ratio of PVR to SVR decreased under both NO and Is-5-MN, whereas the trend was in the opposite direction with PGI2.
Plot of the change in CI induced by PGI2 in relation to the baseline value. There was a significant correlation between both variables (r = 0.66, P < 0.01). This phenomenon substantiates a systemic action of PGI2 and indicates potential for further increase in CI even in the presence of an hyperdynamic circulation.
The same analysis performed on the subset of patients who underwent vasoreactivity testing with the 3 drugs (n = 7) yielded similar results (Fig. 2B).
A comparison of the effects on PAP induced by NO and PGI2 (n = 15) was performed by plotting the changes with 1 drug against the other (Fig. 4). The effect of PGI2 on PAP was more pronounced than with NO, as shown by the majority of points lying below the identity line. With PGI2, 2 patients had a decrease >10 mmHg, and 1 additional patient was close to this value (41.0 to 31.5 mmHg); 5 patients altogether reached a final PAP ≤ 35 mmHg.
Comparison of the acute changes produced by NO and PGI2 in the same patients. A total of 15 patients who had already been tested with NO (x-axis) underwent testing with epoprostenol (y-axis); the mmHg change with each test was plotted for the individual patient. PGI2 exerted a greater effect on PAP than NO, as most of the points lay below the identity line: 2 patients receiving PGI2 had a decrease of PAP ≥ 10 mmHg, fulfilling the Venice criteria. Two other patients with no response to NO had a decrease in PAP with PGI2 just below the threshold of 10 mmHg; another patient had a partial response to both NO and PGI2.
An appraisal of the changes induced by PGI2 and Is-5-MN in the same patients (n = 7; Fig. 5) points to several issues. The modifications produced by PGI2 and Is-5-MN were in the same direction and, interestingly, patients responding to PGI2 also responded to Is-5-MN. What is more relevant is that overall, 6 patients out of 7 ended up with a PAP ≤ 35 mmHg. In addition, the action on PAP of Is-5-MN was more consistent than that of PGI2 and was also observed in 2 patients who did not respond to this test.
Plot of PAP before and after testing with PGI2 and Is-5-MN (n = 7). Lines show individual changes from baseline (open symbol) to the value reached with both vasodilators (closed symbol). A total of 6 patients reached a more favorable hemodynamic setting with PAP ≤ 35 mmHg (dashed lines). Changes were in the same direction in all subjects; the magnitude of changes was similar except in 2 patients who reacted poorly to PGI2 but showed a profound decrease in PAP with Is-5-MN.
DISCUSSION
The major findings of the present investigation were that a sizeable amount of patients with PoPH react to pulmonary vasodilator testing, that PGI2 elicited a greater response than inhaled NO, and that Is-5-MN exerts a conspicuous vasodilator effect on the pulmonary circulation.
It is rather clear that patients with PoPH behave quite differently from patients with other forms of PAH: they have at baseline a distinctive hemodynamic profile29 and respond in their own manner to the acute vasodilator testing.
Effects of Inhaled NO
In our series, the response to inhaled NO, although it was statistically significant, was not relevant in terms of the magnitude of reduction of PAP (2 mmHg on average) and/or PVR.
Only 2 patients showed a decrease in PAP >20%, although it was less than 10 mmHg, thus questioning on one hand, its clinical relevance, and, on the other hand, when the response can be judged as positive. Yet it must be considered that the current consensus guidelines on the response criteria have been established on the basis of the long-term response to Ca-channel blockers in idiopathic PAH,6 and it is not known whether or not these criteria are also appropriate for PoPH or in the setting of screening for the eligibility for LT.
The present results with NO are not different from other trials in PoPH. If we put our data on changes in PAP induced by NO side-by-side with those of other groups reporting apparently conflicting results,9, 10 there is a broad overlap of data, and the apparent discrepancy of results depends on the threshold decrease in PAP that had been preset to define a positive response.
Compared with patients with idiopathic PAH5, 30 the action of NO in PoPH is less significant and might be related to the distinctive hemodynamic setting of cirrhosis.
In idiopathic PAH, screening with inhaled NO more consistently reflects changes in pulmonary vascular tone,7 due to its pulmonary selectivity31, 32 without any inotropic effect.33 In PoPH the lack of response to NO9 might be related to the high GMP-mediated pulmonary vasodilatation induced by increased levels of NO in the supra-hepatic vein of cirrhotic patients (GMP is a nucleotide composed of guanine, ribose, and one phosphate group that is formed during protein synthesis).34, 35 This way of thinking also explains why NO is still effective during the transplant procedure in reversing the acute pulmonary vasoconstriction after the perfusion of the lung by cold blood from the donor organ.11, 36
Effect of PGI2
The vasodilator effect of PGI2, besides being quantitatively more sizeable than that of NO on both PAP and PVR, was more prevalent, as 32% of the patients showed a decrease in PAP ≥20% from baseline. Interestingly, the final PAP was less than 40 mmHg in all patients responding to PGI2. This vasodilatory effect was noticeably associated with the drop of systemic arterial pressure and SVR, thus reflecting the unselective action of PGI2.
As observed in the studies on PAH,32, 33 the predominant pharmacological action of prostacyclin, through which it lowers PAP, is on SVR and CI. In cirrhotic patients with PoPH there are, however, some peculiarities, due to an established hyperdynamic circulation (reduced systemic resistance and elevated CI), which persists though the development of PoPH.29 Interestingly, in our series PGI2 yielded still further systemic vasodilation, despite the background vasodilatation, as previously observed.37 Indeed, the increase in CI correlated with its baseline value (Fig. 3), as if an enlarged compliance allowed greater fluid mass circulation and the action of PGI2 was not affected by, or at least was not mediated by, the same mechanisms that produce vasodilation in cirrhosis. Whether the hemodynamic changes produced by PGI2 may be safely maintained for a long time in cirrhotic patients is questionable: a consequence of the rise in CI is a further increase in hepatic blood flow, potentially worsening portal hypertension,37-39 as suggested by experimental40 and clinical reports.41 For acute vasodilator testing, however, PGI2 seems quite safe and no changes were recorded in right atrial pressure.
In conclusion, the comparison between these 2 vasodilators suggests that, at variance with idiopathic PAH, inhaled NO is not appropriate for acute vasodilator testing in PoPH and PGI2 is preferable.
Isosorbide-5-Mononitrate
The convenience of performing pulmonary vasoreactivity tests in PoPH is illustrated by the acute response to the oral vasodilator Is-5-MN. Among the 8 patients who submitted to this test, 6 showed a decrease in PAP ≥20%, and in 5 this decrease was ≥10 mmHg. In all them, the final PAP was less than 40 mmHg. Interestingly, the action of Is-5-MN had a sort of pulmonary selectivity with a significant decrease of PVR/SVR, with SVR remaining unchanged, similar to inhaled NO.
The action of Is-5-MN is through the release of NO and its acute effect contrasts with the poor action of inhaled NO. The inability of inhaled NO to satisfactorily decrease PVR might be related to the probable saturation of the NO-effector system or to an abnormal alveolar-capillary diffusion,42, 43 in addition to the anatomical remodeling of lung vessels present in pulmonary hypertension. We speculate that NO from the donor Is-5-MN, by contrast, is delivered to the vessel wall from the luminal side, with greater availability to vascular smooth muscle cells.
Yet in this subgroup of patients there was some selection bias, as the majority of them had responded significantly to either NO or PGI2, although in the same patient Is-5-MN resulted in a larger decrease of PAP.
The usefulness of acute vasodilator tests in PoPH has been questioned, as some studies have shown minimal vasodilation.30 Yet our results suggest the opposite: there is a number of patients with PoPH who show a significant pulmonary vasodilator response when tested with PGI2, and that most of them also respond to an oral vasodilator like Is-5-MN. It is possible that in the recently reported, French national registry30 the vasodilator employed was NO, which according to our findings elicits a poor response in PoPH.
Furthermore, in our study, patients not only showed potential for treatment with an oral drug, but also their hemodynamic profile varied to an extent that their candidacy for LT could be reconsidered. In other words, in 6 patients (32% of the whole series) the PAP decreased more than 20%, from the baseline value, reaching a final PAP of ≤35 mmHg (see also Fig. 5). Since current guidelines3 advise not to proceed to OLT in patients with a mean PAP >35 mmHg, we consider that this decision should be taken only after acute vasodilator testing with a drug that is appropriate in the setting of PoPH, namely PGI2. Furthermore, a positive response to PGI2 might identify patients suitable for acute or chronic trial with Is-5-MN, which elicits a rather selective pulmonary vasodilator response. Previous experience suggests potential satisfactory outcome with Is-5-MN in the treatment of PoPH23 and no harm in patients with portal hypertension.24, 25 Whether or not this applies to long-term treatment deserves further investigation.
Acknowledgements
We are indebted to Dr. J.C. Garcia-Pagàn for reviewing and commenting on the manuscript. G.L. Ricci is on leave from the University “La Sapienza,” supported by MIUR-Fondi Ateneo 8111.69.7 and 8111.4.9