Validation of cardiovascular risk scores in a liver transplant population†
See Editorial on Page 352
Abstract
Increased prevalence of cardiovascular risk factors has been acknowledged in liver transplant recipients, and an increased incidence of cardiovascular events has been suspected. Individual risk determination, however, has not yet been established. Outpatient charts of 438 primary liver transplants have been reviewed, and suspected cardiovascular risk factors were correlated with cardiovascular events observed during a follow-up period of 10 yr. Receiver operation characteristics curve (ROC) analysis was performed to validate established cardiovascular risk scores. For calibration, the Hosmer-Lemeshow test was performed. A total of 303 of 438 patients were available for risk factor analysis at 6 months and demonstrated complete follow-up data (175 male, 128 female). A total of 40 of those 303 patients experienced fatal or nonfatal cardiovascular events (13.2%). In univariate analysis, age (P < 0.001), gender (P = 0.002), body mass index (P = 0.018), cholesterol (P = 0.044), creatinine (P = 0.006), diabetes mellitus (P = 0.017), glucose (0.006), and systolic blood pressure (P = 0.043), but not cyclosporine A (P = 0.743), tacrolimus (P = 0.870), or steroid medication (P = 0.991), were significantly associated with cardiovascular events. Multivariate analysis, however, identified only age, gender, and cholesterol as independent predictors. In ROC analysis, corresponding areas under the curve for Systematic Coronary Risk Evaluation Project (SCORE), Prospective Cardiovascular Münster Study (PROCAM), and Framingham risk scores (FRSs) were calculated with 0.800, 0.778, and 0.707, respectively. Calibration demonstrated an improved goodness of fit for PROCAM compared to SCORE risk calculations. In conclusion, SCORE and PROCAM proved to be valuable in discriminating our liver transplant recipients for their individual risk of cardiovascular events. Furthermore, calibrated PROCAM risk estimates are required to calculate the number of patients needed to treat in the setup of prospective intervention trials. Liver Transpl 12:394–401, 2006. © 2006 AASLD.
Besides de novo tumors and renal dysfunction, cardiovascular diseases are a source of major concern in long-term follow-up after liver transplantation.1 High prevalence of cardiovascular risk factors in liver transplant recipients has been widely acknowledged, though the incidence of cardiovascular events compared to standard populations remains controversial.2-4 In our own series, the number of cardiovascular events correlated well with the increased prevalence of cardiovascular risk factors.5 In long-term follow-up, however, death secondary to cardiovascular or cerebrovascular disease is among the 3 most common causes for late hepatic graft loss.6 To determine the individual risk of cardiovascular events, risk scores have been established in general populations. In liver transplant recipients, cardiovascular risk scores were previously used to compare risk profiles with data from standard populations2, 4 or to compare standardized event rates.5 The validity of cardiovascular risk scores in such selected populations, however, has not yet been established. In renal transplant recipients, for example, the Framingham Heart Study score did not accurately predict the individual cardiovascular risk.7 The high prevalence of nontraditional risk factors in the renal transplant population, which have not been considered in the Framingham risk equation, may lead to an underestimation of cardiovascular events.7, 8 Also, the validity of the Framingham risk equation, derived from a North American population, in European patients has been challenged in general.9-12
In this study, we identify independent variables predicting cardiovascular events in our liver transplant population to determine the impact of traditional risk factors. Then 3 established cardiovascular risk scores, derived from European and North American populations, will be evaluated for their ability to separate high-risk from low-risk subjects (validation), and validated scores will be calibrated to determine the individual cardiovascular risk in our liver transplant recipients.
Abbreviations
ROC, receiver operation characteristics curve; SCORE, Systematic Coronary Risk Evaluation Project; PROCAM, Prospective Cardiovascular Münster Study; FRS, Framingham risk score; AUC, area under the curve.
PATIENTS AND METHODS
Patients
Retrospectively, outpatient charts of all 438 primary liver transplants performed between September 1988 and April 1994 have been reviewed. At 6 months posttransplantation, a prospectively scheduled checkup took place and variables suspected to influence cardiovascular risk have been analyzed in this study. Cardiovascular events that occurred during a follow-up period of 10 yr were recorded. Altogether, 135 of 438 patients were excluded from analysis. Thirty-seven patients died before census (8.5%), 26 patients required retransplantation during follow-up, and 72 patients were either lost to follow-up (n = 33), did not present to the outpatient department at 6 months (n = 33), or were infants (n = 6). Changes in medication were left to the discretion of the physician in charge in the outpatient department (R.N.). None of the patients received statin treatment.
Definition of Events
Myocardial infarction confirmed by electrocardiogram or enzyme elevation, and development of coronary heart disease with typical clinical symptoms and confirmed by stress electrocardiogram or coronary angiography were considered coronary events. In addition to coronary events, cardiovascular events summarized cerebral ischemia (infarction, transient ischemic attack, prolonged reversible ischemic neurologic deficit) and peripheral arterial occlusive disease.
Variables
Data obtained at 6 months posttransplantation in 303 liver transplant recipients were age, gender, smoking status, family history of cardiovascular disease, arterial blood pressure, height, weight, medication and serum levels of creatinine, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, and glucose after a fasting period of at least 12 hours. Definition of diabetes and arterial hypertension adopted World Health Organization criteria.13, 14 In brief, a systolic blood pressure over 139 mmHg, a diastolic blood pressure over 89 mmHg, or antihypertensive treatment was considered arterial hypertension. A blood glucose of more than 126 mg/dL and antidiabetic treatment were defined as diabetes mellitus.
Cardiovascular Risk Scores
Three established cardiovascular risk scores have been applied to our liver transplant recipients at 6 months posttransplantation.
The Framingham risk score (FRS) was calculated by use of the algorithm previously described.15 Variables considered in the FRS were gender, age, total cholesterol, high-density lipoprotein cholesterol, systolic blood pressure, and smoking status. The age limit ranged from 30 to 74 yr. The FRS predicts the 10-yr risk of fatal or nonfatal coronary events.
The German Prospective Cardiovascular Münster Study (PROCAM) also predicts the 10-yr risk of fatal or nonfatal coronary events. The score was calculated as previously described.16 Variables considered were gender, age, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides, systolic blood pressure, smoking status, diabetes mellitus, and family history of coronary heart disease. The age limits were 35 to 65 yr in male patients and 45 to 65 yr in female patients.
The European Systematic Coronary Risk Evaluation Project (SCORE) score derived from combined data sets of European prospective studies and predicts the 10-yr risk of fatal cardiovascular events. The algorithm for SCORE calculation has also been previously described.17 Variables entered into the SCORE calculation were gender, age, total cholesterol, systolic blood pressure, and smoking status. The age limits were 40 to 65 yr in male and female patients.
Statistics
Data were expressed as median and range or mean ± standard error of mean, unless noted otherwise. Continuous variables with Gaussian distributions were compared by Student's unpaired t-test. Categorical variables were compared by the χ2 test. Continuous variables with a non-Gaussian distribution were compared by Mann-Whitney U-test. Multivariate logistic regression modeling with stepwise backward or forward covariable selection was performed to determine the association between cardiovascular or coronary events and suspected cardiovascular risk factors. Variables with a significant impact in univariate analysis (P < 0.05) were entered in the regression models. Receiver operation characteristics (ROC) analysis was performed to determine the ability of each of 3 established cardiovascular risk scores to discriminate between low-risk and high-risk patients from our liver transplant population. The area under the curve (AUC) for coronary events was calculated, and the standard error as well as the P value were given. An AUC of 1 indicates a perfect discrimination capability of a given test, while an AUC of 0.5 indicates a discrimination by chance alone. For calibration of each risk score, the Hosmer-Lemeshow test was performed. A high χ2 value along with a high P value indicates a good model fit. Additionally, patients eligible for the respective risk score have been divided into quintiles according to their estimated risk of events. For each quintile, the ratio of observed events over estimated events (sum of individual risk calculations) was calculated. The weighed mean of calculated ratios was considered the overall risk ratio, and 95% confidence intervals were given. All calculations were done using the SPSS software package (version 12.0 for Windows, SPSS Inc., Chicago, IL). A P value of <0.05 was considered statistically significant.
RESULTS
Patient Characteristics
Of 303 patients eligible for analysis of cardiovascular risk factors at 6 months posttransplantation, 175 were male (57.8%) and 128 were female (42.2%). The median age at census equaled 48 yr (16-66 yr). During 10 yr of follow-up, 40 patients (13.2%) experienced cardiovascular events, including 24 patients with coronary events (7.9%, Table 1). Altogether, 69 fatalities were observed (22.8%), with 4 incidents related to cardiovascular events (myocardial infarction in all cases).
| Time after LT (months) | Gender | Age (yr) | Cardiovascular event | SCORE (% 10-yr risk) | PROCAM (% 10-yr risk) | |
|---|---|---|---|---|---|---|
| Fatal | 19 | M | 49 | MI | 6.15 | 13.20 |
| 66 | M | 47 | MI | 3.75 | 6.10 | |
| 119 | F | 56 | MI | 3.73 | n.a. | |
| 121 | M | 37 | MI | 0.40 | 1.60 | |
| Nonfatal | 8 | F | 41 | CI | 0.11 | n.a. |
| 10 | M | 56 | MI | 1.51 | 2.30 | |
| 10 | M | 52 | CHD | 11.62 | 5.70 | |
| 11 | M | 65 | CI | 8.00 | 13.20 | |
| 12 | F | 50 | CI | 0.53 | n.a. | |
| 13 | M | 45 | MI | 1.32 | 7.00 | |
| 18 | F | 56 | pAOD | 1.46 | 4.90 | |
| 20 | M | 44 | CI | 1.58 | n.a. | |
| 24 | M | 55 | CHD | 3.52 | 21.70 | |
| 26 | M | 35 | CHD | 0.17 | n.a. | |
| 32 | M | 46 | CHD | 3.26 | 19.60 | |
| 37 | M | 57 | MI | 3.88 | n.a. | |
| 39 | M | 50 | CHD | 5.31 | 16.80 | |
| 44 | F | 64 | TIA | 3.07 | n.a. | |
| 49 | F | 62 | TIA | 2.99 | 4.20 | |
| 63 | M | 60 | AA | 5.79 | 12.80 | |
| 70 | M | 55 | CHD | n.a. | n.a. | |
| 74 | M | 47 | CHD | 0.98 | 8.80 | |
| 75 | M | 59 | CI | 3.81 | 5.70 | |
| 78 | M | 35 | MI | 0.84 | 2.80 | |
| 83 | M | 59 | CHD | 5.53 | 5.70 | |
| 84 | M | 50 | CI | 1.48 | 1.10 | |
| 85 | M | 63 | CHD | 6.91 | n.a. | |
| 109 | M | 56 | AA | 3.59 | n.a. | |
| 111 | M | 60 | MI | 22.67 | 30.00 | |
| 113 | M | 43 | CHD | 1.36 | 2.80 | |
| 115 | M | 52 | CHD | 4.67 | 17.50 | |
| 115 | M | 47 | CHD | 3.95 | 10.70 | |
| 116 | M | 53 | CI | 2.13 | 5.10 | |
| 119 | M | 59 | TIA | 8.89 | 4.80 | |
| 120 | M | 46 | CHD | 1.60 | n.a. | |
| 121 | M | 57 | MI | 5.49 | n.a. | |
| 121 | M | 53 | CHD | 2.59 | 8.00 | |
| 121 | M | 62 | CI | 9.37 | 30.00 | |
| 122 | M | 54 | CI | 3.21 | 13.20 | |
| 125 | M | 52 | pAOD | 3.52 | 8.80 |
- NOTE: During 10 yr of follow-up, 40 cardiovascular events were observed in 303 adult survivors after liver transplantation (LT). Fatal and nonfatal events, time of occurrence after LT, gender, and age are given. Where applicable, PROCAM and SCORE estimates of the individual 10-yr risk of coronary events, based on demographic data and laboratory findings only, are also given.
- Abbreviations: MI, myocardial infarction; CI, cerebral infarction; CHD, coronary heart disease; TIA, transient ischemic attack; AA, aortic aneurysm; pAOD, peripheral arterial occlusive disease; n.a., not applicable.
Cardiovascular Risk Factors
Patients who experienced cardiovascular events were significantly older than patients without such events (52.5 (35-66) yr vs. 47 (16-66) yr; P < 0.001). Comparing patients with and without coronary events, however, age was similar (49.5 (35-66) yr vs. 48 (16-66) yr; P = 0.106) in both groups. Male patients were at higher risk for cardiovascular (22.3 vs. 8.6%; P = 0.002) as well as coronary (14.3 vs. 2.3%; P < 0.001) events compared to female patients. The body mass index in groups of patients developing cardiovascular or coronary events was higher than in all other patients (cardiovascular events: 24.8 (17.0-38.4) kg/m2 vs. 23.1 (16.4−40.4) kg/m2; P = 0.018; coronary events: 25.3 (19.4-38.4) kg/m2 vs. 23.4 (16.4-40.4) kg/m2; P = 0.014). Impaired lipid metabolism, expressed in higher cholesterol levels was found in patients with cardiovascular events (cardiovascular events: 240.5 (122-376) mg/dL vs. 229 (86-452) mg/dL; P = 0.044; coronary events: 241 (122-376) mg/dL vs. 229 (86-452) mg/dL; P = 0.084), while patients experiencing coronary events presented with increased values of triglycerides (cardiovascular events: 168 (72-816) mg/dL vs. 163 (53-716) mg/dL; P = 0.102; coronary events: 188 (86-816) mg/dL vs. 162 (53-716) mg/dL; P = 0.024). Also, mean creatinine concentrations were higher in patients presenting cardiovascular (1.3 ± 0.06 mg/dL vs. 1.1 ± 0.02 mg/dL; P = 0.006) or coronary (1.4 ± 0.08 mg/dL vs. 1.1 ± 0.02 mg/dL; P = 0.003) events than in those patients without such events. Patients with diabetes mellitus were at higher risk for cardiovascular events than nondiabetics (25 vs. 13.5%; P = 0.017). Correspondingly, blood glucose was higher in patients developing cardiovascular events than in all other patients (104.5 (65-430) mg/dL vs. 94 (58-289) mg/dL; P = 0.006). In patients experiencing coronary events, however, neither diabetes mellitus (15.7 vs. 7.6%; P = 0.105) nor glucose concentration (101.5 (65-264) mg/dL vs. 95 (58-430) mg/dL; P = 0.108) demonstrated any impact. Interestingly, the presence of arterial hypertension did not influence occurrence of cardiovascular (19.1 vs. 10.6%; P = 0.065) or coronary (10.1 vs. 7.5%; P = 0.470) events. Systolic blood pressure, however, was significantly higher in patients experiencing one or the other event (cardiovascular: 140 (105-200) mmHg vs. 130 (90-200) mmHg; P = 0.043; coronary: 140 (110-190) mmHg vs. 130 (90-200) mmHg; P = 0.047) than in patients without events. Treatment with either cyclosporine A or tacrolimus had no impact on the occurrence of cardiovascular (16 vs. 17%; P = 0.825) or coronary (10 vs. 7%; P = 0.392) events. Also, the daily dosage of the respective calcineurin inhibitors did not differ between patients experiencing cardiovascular or coronary events during follow-up (tacrolimus: cardiovascular: 6.7 ± 0.66 mg vs. 6.8 ± 0.26 mg; P = 0.920; coronary: 6.7 ± 0.84 mg vs. 6.8 ± 0.25 mg; P = 0.959; ciclosporine A: cardiovascular: 343.8 ± 18.36 mg vs. 339.4 ± 8.09 mg; P = 0.831; coronary: 350.5 ± 25.85 mg vs. 339.0 ± 7.71 mg; P = 0.641). Equally, the dosage of steroids was similar in patients with cardiovascular (9.7 ± 0.54 mg vs. 12.2 ± 1.63 mg; P = 0.486) or coronary (9.3 ± 0.59 mg vs. 12 ± 1.5 mg; P = 0.569) events, compared to those without such events.
Multivariate Analysis
The above-mentioned variables with a significant impact on cardiovascular events in univariate testing were entered into multivariate logistic regression models. In forward stepwise variable selection, only age, gender, and cholesterol level at 6 months posttransplantation have been identified to significantly influence the incidence of cardiovascular events (Table 2). Backward variable selection confirmed those findings. Applying both models to coronary events alone, forward stepwise variable selection identified gender, body mass index, and creatinine concentration as independent predictors. Backward variable selection additionally identified triglyceride levels with an impact on the incidence of coronary events.
| Independent variable | Risk of cardiovascular event | P value | |
|---|---|---|---|
| Odds ratio | 95% CI | ||
| Age (yr) | 1.063 | 1.025-1.104 | 0.001 |
| Gender (male) | 2.854 | 1.339-6.086 | 0.007 |
| Cholesterol (mg/dL) | 1.006 | 1.000-1.011 | 0.039 |
- NOTE: Multivariate binary logistic regression modeling was performed to identify independent risk factors for cardiovascular events in 303 adult liver transplant recipients. All variables with a significant impact in univariate analysis were entered. Stepwise backward covariable selection was applied. The odds ratio, the 95% confidence interval (95% CI), and the P value for each independent variable are given.
Cardiovascular Risk Scores: Discrimination
Ninety-three patients were eligible (age limits) and provided complete sets of data (total cholesterol, high-density lipoprotein cholesterol, systolic blood pressure, smoking status) for Framingham score calculation. Comparing FRS estimates and observed coronary events in ROC analysis, the AUC calculated with 0.707 (standard error = 0.061; P = 0.017). Figure 1, however, demonstrates a low discrimination capability for patients with high-risk scores.
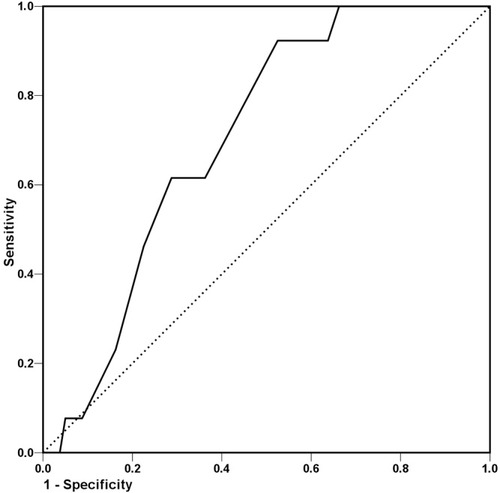
FRS discrimination. ROC analysis was performed to determine the ability of the FRS to discriminate between low-risk and high-risk patients from the liver transplant population. The AUC calculated with 0.707. The figure, however, demonstrates low discrimination capability for patients with high-risk scores (lower left part of the curve). The diagonal depicts an AUC of 0.5 and indicates discrimination by chance alone.
For PROCAM evaluation, only 67 patients were eligible due to restrictive inclusion criteria (age limits, smoking status, family history, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides, systolic blood pressure, diabetes mellitus). The AUC calculated with 0.778 (standard error = 0.067; P = 0.004). Figure 2 depicts the corresponding graph, demonstrating an improved discrimination between high-risk and low-risk patients.
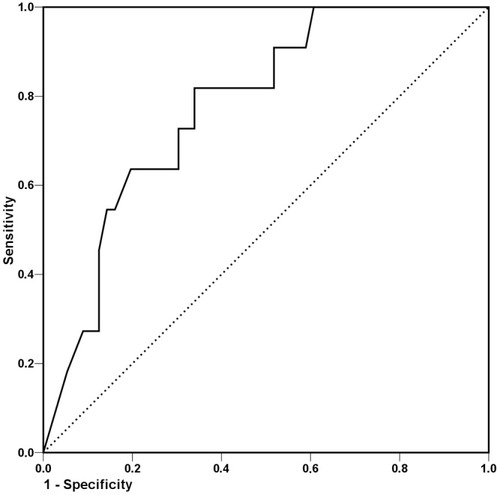
PROCAM discrimination. ROC analysis was performed to determine the ability of the PROCAM score to discriminate between low-risk and high-risk patients from the liver transplant population. The AUC calculated with 0.778. The figure demonstrates good discrimination capability. The diagonal depicts an AUC of 0.5 and indicates discrimination by chance alone.
Due to less restrictive inclusion criteria (age limit, total cholesterol, systolic blood pressure, smoking status), 126 patients were eligible for SCORE analysis. The corresponding AUC for coronary events calculated with 0.800 (standard error = 0.052; P < 0.001), demonstrating an excellent discrimination between high- and low-risk patients (Fig. 3).
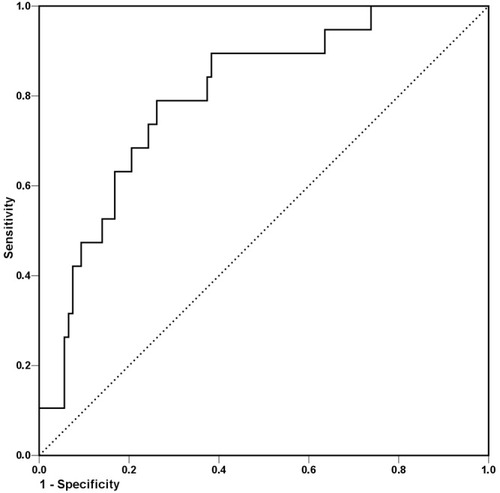
European SCORE discrimination. ROC analysis was performed to determine the ability of the European SCORE score to discriminate between low-risk and high-risk patients from the liver transplant population. The AUC calculated with 0.800. The figure demonstrates excellent discrimination capability. The diagonal depicts an AUC of 0.5 and indicates discrimination by chance alone.
PROCAM and SCORE: Calibration
As only 1 fatal coronary event occurred in patients eligible for SCORE evaluation, the Hosmer-Lemeshow test has been performed to calibrate for fatal and nonfatal coronary events. χ2 has been computed with 9.1 at a P value of 0.333, indicating an acceptable goodness of fit. Graphical analysis, however, demonstrated a strong underestimation of coronary events in low- and very high risk patients (2nd and 5th quintiles, Fig. 4).
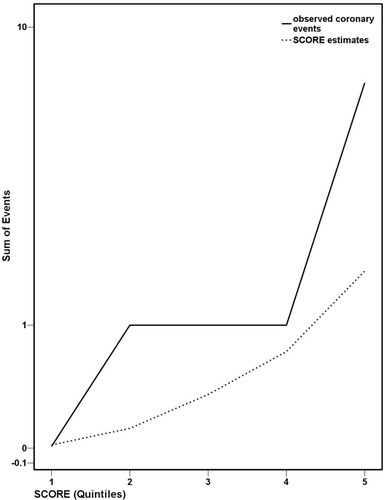
European SCORE calibration. Patients eligible for the European SCORE have been divided into quintiles according to their estimated risk of events. For each quintile, numbers of observed and estimated events (sum of individual risk calculations) were calculated. Graphical analysis demonstrates a strong underestimation of coronary events in low- and very high risk patients (2nd and 5th quintiles).
PROCAM score evaluation demonstrated an improved goodness of fit (χ2 = 6.9; P = 0.546), and the overall risk ratio calculated with 0.887 (95% confidence interval = 0.241-1.532), indicating a risk estimation slightly higher than the risk observed in our population. Graphical analysis demonstrated that overestimation occurred in very low and low-risk patients only (1st and 2nd quintiles, Fig. 5).
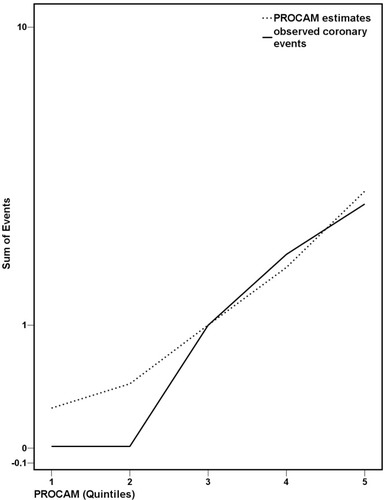
PROCAM calibration. Patients eligible for the PROCAM have been divided into quintiles according to their estimated risk of events. For each quintile, numbers of observed and estimated events (sum of individual risk calculations) were calculated. Graphical analysis demonstrates that overestimation occurred in very low and low-risk patients only (1st and 2nd quintiles).
DISCUSSION
Although the application of cardiovascular risk scores in liver transplant recipients has previously been described,2, 4 validity in such selected patient populations has not yet been established. In our own liver transplant population at 6 months posttransplantation, PROCAM and SCORE provided an excellent measure to discriminate between patients at high or low risk for coronary events. Furthermore, calibration of PROCAM-estimated event rates demonstrated a strong correlation with the number of observed coronary events.
Analysis of suspected cardiovascular risk factors in our liver transplant population confirmed the well-established impact of age, gender, systolic blood pressure, diabetes, body weight, and impaired lipid metabolism on the risk of cardiovascular events in subsequent years. Arterial hypertension, defined as elevated blood pressure or antihypertensive treatment, had no impact on cardiovascular event rates, thus indicating that successful lowering of systolic blood pressure may be beneficial in preventing cardiovascular events. The choice of calcineurin inhibitor or prednisolone dosage at 6 months posttransplantation, however, had no significant impact. Although described cardiovascular risk profiles have been in favor of tacrolimus compared to cyclosporine A,18-26 we previously were able to demonstrate that differences were compensated in long-term follow-up.5 Therefore, the application of general population-derived cardiovascular risk scores in liver transplant recipients seemed permissible.
As in European renal transplant recipients,7 the North American-derived FRS also failed to accurately identify high-risk liver transplant recipients in our study population. European-derived PROCAM16 and SCORE,17 however, discriminated well between high- and low-risk patients after liver transplantation. In general, the accuracy of FRS to predict coronary events in European populations has been considered controversial.27, 28 Whether the low discrimination capability of FRS relates to a differing ethnic origin of risk scores,29 rather than transplantation-associated factors, remains unclear.
Risk score calibration demonstrated an acceptable goodness of fit for SCORE to predict coronary events in our liver transplant population. The endpoints of the SCORE project, however, were fatal events only.17 Accordingly, estimated numbers of events were considerably lower in very high risk patients than observed numbers of nonfatal events. Overall, the number of fatal events in our study population was low, which might be due to a high health alert and close surveillance, leading to early detection of coronary heart disease. Therefore, fatal events may not be an appropriate measure in such selected populations.
PROCAM risk calculation presented an excellent calibration with our liver transplant population. Only in low-risk individuals did the estimated number of coronary events exceed the number of events actually observed. The overall risk ratio calculated with 0.887.
In conclusion, PROCAM coronary risk estimates provide a valid tool to identify individual liver transplant recipients at high risk for coronary events as early as 6 months posttransplantation. Based on published guidelines,30 threshold triggers may be applied to initiate lifestyle changes, prophylactic drug therapies, or changes of immunosuppressive regimens for the prevention of primary or recurrent cardiovascular disease in liver transplant recipients. Also, repeated PROCAM risk calculations may be facilitated to control for successful intervention efforts. Furthermore, calibrated PROCAM risk estimates are required to calculate the number of patients needed to treat in the setup of prospective intervention trials. Prior to application in different liver transplant populations, however, similar validation studies are required.