Costal Cartilage Considerations: Novel Use of Handheld Ultrasound Device in Rhinoplasty
Editor's Note: This Manuscript was accepted for publication on May 08, 2023.
Presented as a poster at the Triological Society 2022 Combined Sections Meeting, Coronado, CA on January 10th, 2022.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Graphical Abstract
INTRODUCTION
Primary and secondary rhinoplasty frequently require structural augmentation of the nasal framework to provide adequate airway support and also achieve aesthetically desirable results. At times, this requires the use of graft material. Although septal remains the ideal material of choice, conchal and costal cartilage are also used. Autologous costal cartilage is considered by many as the ideal source of cartilage for revision rhinoplasty where other reservoirs are often depleted. However, calcification of costal rib cartilage can be problematic, as it can be difficult to harvest, cut, and fashion.1 Although the prevalence of costal cartilage calcification increases with age, it is not negligible in younger populations.2 Identifying calcified graft material and thereby avoiding harvesting of a heavily ossified rib in favor of another rib or use of allograft is important. Other studies have shown that preoperative computed tomography (CT) scans provide insight into the presence and patterns of calcification.3, 4 However, CT scans expose patients to radiation, albeit modestly, and are an additional cost. For these reasons, there is a need for an inexpensive, efficient, and easy-to-use means for the surgical team to evaluate costal cartilage quality in the perioperative period.
Point-of-care ultrasonography (POCUS) refers to the use of ultrasound at the patient's bedside by clinicians other than a radiologist or cardiologist.5 In recent years, there has been increased practice of POCUS and subsequently, an increased demand for ultrasound devices that complement this practice.5 In response, recent advancements have made handheld ultrasound devices (HUD) even more compact, affordable, and easy to operate.5 To our current knowledge, there is limited literature on HUD in facial plastic surgery and rhinoplasty. With this study, we hope to show that HUD can be utilized by individuals with minimal training as a convenient, inexpensive, and effective means of perioperative evaluation of costal cartilage quality for rhinoplasty.
METHODS
This study was conducted in accordance with institutional review board approval (IRB #20152490). The charts of patients who underwent revision rhinoplasty and had perioperative HUD were reviewed. HUD images were compared with pre-operative CT images or intra-operative images of harvested costal cartilage rib graft when available.
HUD Training and Examination
Perioperative examinations with the HUD were conducted by members of the surgical team with minimal to moderate HUD training and experience (D.M.H., K.R.P., K.H., and B.R.P.). Three of these US operators were medical students although one was a facial plastic surgery fellow. Experience with US devices ranged from approximately 3 to 30 h of formal HUD training across the operators performing US examination in this study. Operators were trained in general ultrasound anatomy and physiology. For our study, operators were shown representative transverse and longitudinal ultrasound images of rib cartilage from a previous study that also included ossification patterns and also practiced obtaining control images on each other. Training sessions were less than 20 min.
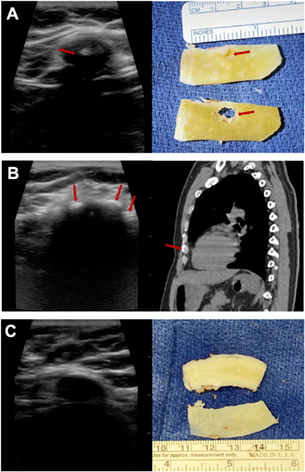
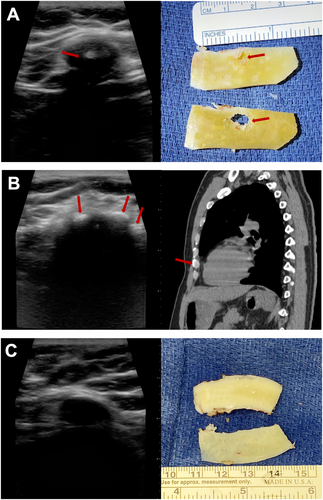
These examinations were performed with a portable ultrasound device (iQ+, Butterfly Network, Guilford, CT) paired with a commercial tablet device (4th Generation iPad Pro, Apple, Cupertino, CA) as seen in Figure 1. The HUD utilized a smartphone/tablet application-based interface that allows the user to select between 22 tissue-type presets across six different imaging modes: B-mode, M-mode, Color Doppler, Power Doppler, Pulsed Wave Doppler, Biplane, and Fetal Heart Sounds. For this study, we selected the Musculoskeletal (MSK)-Soft Tissue preset that utilizes B-mode for ultrasound imaging. Perioperatively, the patient's fifth, sixth, or seventh ribs were identified via palpation and anatomical landmarks. Each rib was imaged transversely via the HUD, starting laterally and sweeping medially along the rib to the costochondral junction. Upon HUD examination, the costochondral junction was clearly visible; the costal cartilage appeared as a hypoechoic region with a more hyperechoic boundary surrounding the cartilage peripherally as shown in the representative images in Figure 2C. Calcifications are hyperechoic areas with posterior acoustic shadowing located on the central (Figure 2A) or peripheral (Figure 2B) areas of the rib cartilage. Video obtained during HUD examination was recorded in the patient's chart. Chart review included evaluation of ossification presence and correlation with preoperative CT and/or images of gross pathology when available. This HUD evaluation method is highlighted in Supplemental Video 1 which can be used in a comprehensive instructional resource for those looking to learn this method (Audio 1).

Surgical Procedure
The ribs were palpated and counted, with either the fifth, sixth, or seventh rib selected as the rib graft harvest site. A 2 cm incision was created directly over the rib selected for harvest in males. For females, the incision site was marked at the inframammary fold. The incisions were then made and subsequently, the skin and subcutaneous layers were dissected to access the muscle fascia. Fascia was divided, muscles bluntly separated, and the rib was exposed for dissection. The perichondrium was carefully dissected off the rib, and the cartilaginous rib was cut on both ends and then subsequently harvested. The rib was then placed on the sterile operating room table and carefully cut, photographed in cross-section, and then prepared for subsequent use as graft material.
RESULTS
After minimal training, all four of the HUD operators were able to successfully perform ultrasound and identify both the presence or absence of calcification in costal rib cartilage for all 10 patients. Of the 10 patients, nine had calcification that was identified through ultrasound and was then correlated with gross pathology and/or prior CT scans. Three of these patients had peripheral calcification, five had central calcification, and one had both peripheral and central calcification patterns present. Only one patient had no calcification indicated on ultrasound which was correlated with gross pathology (Figure 2C).
DISCUSSION
The presence and extent of rib cartilage calcification have historically been evaluated with preoperative CT scans and standard ultrasound, or with the interrogation of the rib quality using a needle translated across the rib surface percutaneously.3, 4 However, both modalities have limitations. Some patients have pre-existing CT scans obtained for unrelated purposes, and these ought to be reviewed. Many surgeons order CT scans for patients that they deem more likely to have heavily ossified costal cartilage, and in general this is more common in older patients. This can be expensive, time-consuming, and can unnecessarily expose patients to ionizing radiation, albeit modest. In a study by Bozzato et al., standard US was validated as an effective means of evaluating the costal margin.4 However, compared to HUD, standard US devices are far more expensive and may require extensive training to develop expertise.
In this study, we found that the Butterfly iQ+ HUD can be used to effectively evaluate the costal cartilage quality of patients preoperatively, helping the surgeon identify and select ideal options for tissue harvest. HUD readily detects calcification and provides information on spatial distribution. As mentioned, a major advantage of this proposed method is the low cost. The Butterfly iQ+ ultrasound device is priced at $2,399 with annual subscription costs ranging from $199/year at the most basic to $420/year for the most advanced; this is far more inexpensive compared to standard US devices. There are also many devices at an even more economical price point, but the Butterfly and devices like it are being used and issued to medical students on admission at many medical schools.
This application-based HUD was paired with either a tablet device or smartphone device, adding to its' ease of use and economy, along with compact size. Like most tablet/smartphone devices or apps, the software is intuitive and easy to use. Clinicians with minimal to moderate expertise with ultrasonography are able to successfully ultrasound rib cartilage and evaluate images for calcification presence and patterns as validated with CT scans and/or gross pathology.
In summary, we have found that HUD can be used as an economical, convenient, and easy-to-use method for evaluating the presence and patterns of calcification on rib cartilage prior to surgery. Our HUD findings correlated with CT scan/gross pathology results.