Modified Olfactory Training Is an Effective Treatment Method for COVID-19 Induced Parosmia
Editor's Note: This Manuscript was accepted for publication on February 28, 2022.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Abstract
Objectives
Coronavirus disease (COVID-19) infection often causes olfactory dysfunction and parosmia may occur in some patients with olfactory dysfunction. In this study, we retrospectively investigated the effectiveness of modified olfactory training (MOT) for the treatment of COVID-19-induced parosmia.
Study Design
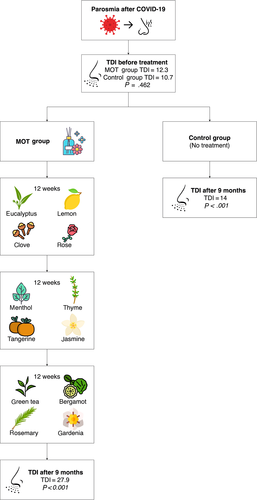
This study presents results of MOT performed with 12 odors for 36 weeks in patients with olfactory dysfunction following COVID-19 infection. A total of 75 participants were included in the study (mean age 33 years, range 16–60 years).
Methods
The patients were separated into two groups: 1) Treatment group consisted of parosmia patients who received MOT with three sets of four different odors sequentially. 2) Control group consisted of parosmia patients who did not perform any olfactory training. Both groups were matched for age and sex distribution of participants. TDI scores were compared at the time of application and at the end of the 9th month by the Sniffin' Sticks Test. The results of the 0th and 9th months were recorded by applying the parosmia assessment scale to both groups. The results were analyzed statistically, and p < 0.05 was considered significant.
Results
When the treatment group and the control group were compared, a significant improvement was observed in both groups at the third, sixth, and ninth month, however the improvement in the treatment group was found to be better than in the control group (P < .001). Extending the treatment from 6 to 9 months in the treatment group was found to be effective in mitigating parosmia complaints and improving discrimination scores (P < .001).
Conclusion
This study has shown that modified olfactory training is effective in the treatment of parosmia following COVID-19 infection.
Level of Evidence
3 Laryngoscope, 132:1433–1438, 2022
INTRODUCTION
One of the characteristic symptoms of the coronavirus disease (COVID-19) infection, which emerged in Wuhan, China in 2019 and was given pandemic status by the WHO in March 2020, is olfactory dysfunction and is encountered in approximately 60% of the cases, although varying reports are present in different series.1, 2 Parosmia is among the qualitative olfactory dysfunctions and is defined as the misperception of odors (such as perception as rotten or burnt odor).3 Viral upper respiratory tract infections, head trauma, idiopathic causes, sinonasal, and neurodegenerative diseases are included in the etiology of parosmia, which often develops within weeks following anosmia and/or hyposmia.4, 5 Parosmia, which has been reported to develop after COVID-19 disease, greatly affects the quality of life of patients. Parosmia might develop as a late complication of post-viral infection and is thought to be a sign of recovery in olfactory functions following anosmia.6, 7 Classical olfactory training (COT), which was first reported by Hummel et al. for the treatment of anosmia, was also demonstrated in the treatment of parosmia by Liu et al. to determine its effectiveness.8, 9 However, there is no research yet on the treatment of post-COVID-19 parosmia.
In this study, we investigated the effectiveness of treatment by modified olfactory training (MOT) in patients who developed post-COVID-19 parosmia.
MATERIALS and METHODS
Participants
Patients referred to the otorhinolaryngology clinic of Acibadem Taksim Hospital between April 2020 and July 2021 with complaints of anosmia, hyposmia, and parosmia following COVID-19 infection were included in the study. The study was approved by the Medical Ethics Committee of Acibadem Mehmet Ali Aydinlar University (2021–20/17). All studies were conducted in accordance with the Declaration of Helsinki regarding biomedical studies involving human subjects, and written informed consent was obtained from all participants prior to the study.
Study Design
Parosmia patients who volunteered for the study and met study criteria were separated into two age and gender matching groups. Both these groups consisted of patients who had anosmia anamnesis following COVID-19 infection. The first group consisted of 38 patients who received MOT and the mean time of parosmia onset was found to be 2.5 months after COVID-19 infection. It was determined that these patients referred to our clinic after 1 to 6 months following COVID-19 infection. At the time of admission, parosmia assessment scale and Sniffin’ Sticks test were applied to patients and TDI (threshold, discrimination, and identification) scores were determined. Following 3, 6, and 9 months of MOT, the Sniffin’ Sticks test and parosmia assessment scale were re-applied. The second group consisted of 37 patients who had parosmia onset between 1 and 6 months after COVID-19 infection and who did not want to participate in Mot treatment. The Sniffin’ Sticks test and parosmia assessment scale were applied to these patients at admission and at the ninth month of follow-up.
Parosmia diagnosis was given to patients by an experienced otolaryngologist after a detailed history, application of parosmia evaluation scale, and nasal endoscopy (Table I).
| 1 Point | 0 Points | |
|---|---|---|
| Frequency of occurrence | Daily | Otherwise |
| Intensity | Very strong | Otherwise |
| Social effects | Yes | No |
- The summary score represents the degree of the disorder.
Modified Olfactory Training
Olfactory rehabilitation was performed for 36 weeks using 12 different scents with the MOT method described by Altundag et al.10 Olfactory training consisted of smelling of the scents for 10 seconds alternately by leaving 10 seconds intervals between different scents. The training was applied for 5 minutes twice a day. Patients were advised to perform scent therapies before breakfast in the morning and before going to bed in the evening. The therapy began with scents of eucalyptus, lemon, clove, and rose twice a day for the first 12 weeks. For the next 12 weeks, the scents of menthol, thyme, tangerine, and jasmine were used. During the last 12 weeks, scents of green tea, bergamot, rosemary, and gardenia were used.10
Olfactory Test
The psychophysical testing of olfactory function was performed using the validated Sniffin’ Sticks (Burghart, Wedel) test, for which odorants were presented in commercially available felt-tip pens.11, 12 First, the pen's cap was removed by the experimenter for approximately 3 seconds for odor presentation, and then the tip of the pen was placed about 1 to 2 cm in front of the nostrils. The test consisted of one threshold and two suprathreshold subtests, namely a test for thresholds of pulseless electrical activity (PEA), a test for odor discrimination (16 triplets with two different odors), and one for odor identification (16 common odors, presented in a four-alternative, forced-choice procedure). The maximum score of each subtest was 16, resulting in a maximum composite score of 48 (TDI [threshold, discrimination, and identification] score).13 Normosmia is described for TDI composite scores of more than 30.3, with a cutoff between functional anosmia and hyposmia at 16.5.14
Parosmia Assessment Scale
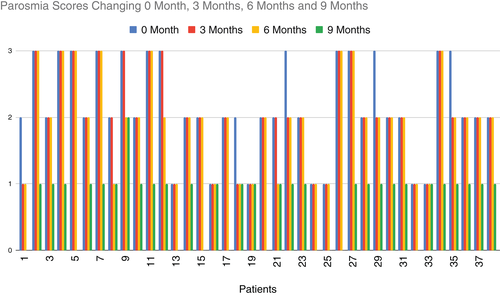
Parosmia was quantified in 3 degrees (0–1 point) with these factors: frequency of occurrence: daily = 1 point, otherwise = 0 points, intensity: very strong = 1 point, otherwise = 0 points, social effects (e.g., weight loss, significant change of habits): yes = 1 point, no = 0 points. The total score represents the degree of the disorder (Table I). All patients were asked to answer this test at the time of admission and at the end of the 9th month.15, 16
Statistical Analysis
Statistical analyses were performed using SPSS 21.0 (SPSS Inc., Chicago, IL). Differences between groups were evaluated using analysis of variance (ANOVA) or Chi-square test when appropriate. Post hoc Bonferroni tests were also performed to identify differences between groups. To investigate olfactory function in relation to the continuous variables measured in this study, data were presented in a multivariate ANOVA using the general linear model. Correlation analyses were calculated according to the Pearson test and the level of significance was determined as 0.05.
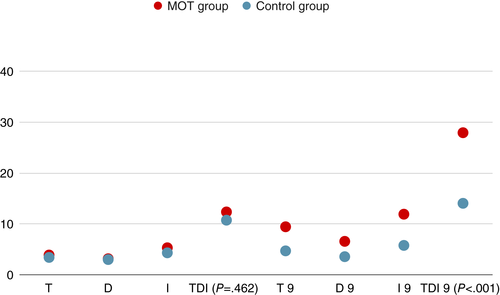
RESULTS
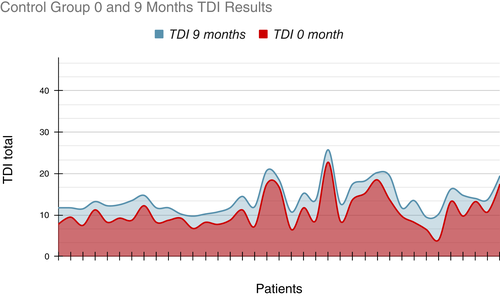
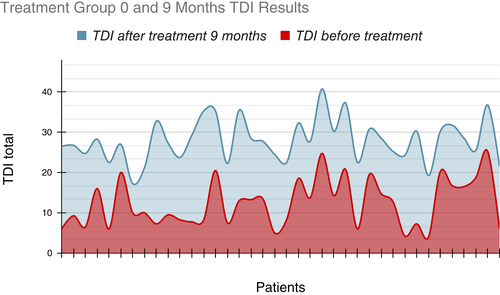
This study included 75 patients with a mean age of 33 years ranging between 16 and 60 years. The treatment group performed MOT using 12 different scents (n = 38; mean age 31.7 years; 31 women, 7 men). In the treatment group, where the mean disease duration was 13.4 months, the mean time of onset of parosmia was 2.3 months following the end of general symptoms of COVID-19 (Table II). MOT groups initial mean TDI scores was calculated as 12.3 (T:3.9 D:3.1 I:5.3), the third month was 16.7 (T:5.4 D:3.6 I:7.7), while it was 21.4 at the sixth month (T:7.5 D:4.2 I:9.7), and 27.9 at the ninth month (T:9.4 D:6.6 I:11.9). (These differences were statistically significant, P < .001). The patients at the control group did not receive any rehabilitation therapy (n = 37; mean age 34.3 years; 21 women, 16 men). In the control group, it was observed that the mean duration of the disease was 13.4 months with parosmia onset starting on average after 2.2 months following the end of general symptoms of COVID-19. The control groups initial mean TDI score was 10.7 (T:3.4 D:3 I:4.3) and after the ninth month was 14 (T:4.7 D:3.5 I:5.8). The difference between the TDI scores at admission and at the ninth month in control group was statistically significant (P < .001) (Table III). No significant difference was observed in the initial TDI scores of the treated and untreated groups (P = .462). However, the TDI score of the treatment group at the ninth month was higher than the control group and this difference was statistically significant (P < .001) (Fig. 1). When the initial parosmia assessment scores of the treated and untreated groups were compared, no significant difference was observed between the two groups (P = .620). At the end of 9 months, a significant decrease was observed in parosmia scores in both groups (P = .001). The improvement in the treatment group was significantly better (P = .001).
| Age (years) | ||||
| MOT | 31.7 | P: .5 | ||
| Control | 34.3 | |||
| Gender | ||||
| MOT | n | % | ||
| M | 7 | 18.4 | P: .025 | |
| F | 31 | 81.6 | ||
| Control | ||||
| M | 16 | 43.2 | ||
| F | 21 | 56.8 | ||
| OoPAC | (months) | |||
| MOT | 2.3 | |||
| Control | 2.2 |
- MOT = modified olfactory training; OoPAC = onset of parosmia after COVID.
| N | 0 Month | 9 Months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| T | D | I | TDI | T | D | I | TDI | ||
| MOT | 38 | 3,9 | 3,1 | 5,3 | 12,3 | 9,4 | 6,6 | 11,9 | 27,9 |
| CG | 37 | 3,4 | 3 | 4,3 | 10,7 | 4,7 | 3,5 | 5,8 | 14 |
| P | .462 | <.001 | |||||||
- D = discrimination; I = identification; MOT = modified olfactory training; T = thresholds.
DISCUSSION
Parosmia, which is included in post-infectious olfactory dysfunction, is a condition that should be differentiated from cacosmia, in which odors are perceived differently and non-existent odors are perceived poorly. Patients can define parosmia very clearly through food. Some studies have shown that fragrance substances in certain foods (coffee, eggs, onions, garlic) can trigger attacks of parosmia. Because these fragrances have lower thresholds than other fragrances, they may be more likely to trigger parosmia.15, 17 Post-infectious olfactory dysfunction (PIOD) is a rather common disorder that usually resolves spontaneously. Although many treatment methods have been investigated, COT and MOT are reported to be the most effective treatment modalities in the treatment of PIOD. Moreover, the study by Altundag et al. suggests better symptomatic improvement and increased TDI scores in MOT compared to COT.8, 10 Since COVID-19 infection was declared a pandemic and one major finding related to it is olfactory dysfunction, many studies have been carried out for the treatment of post-COVID-19 olfactory loss. On the other hand, the diagnosis and treatment of parosmia, which may develop after COVID-19 infection and significantly affect the quality of life of patients, have not been studied widely.5, 6, 18 Liu et al. showed that olfactory rehabilitation in PIOD, post-traumatic olfactory disease and idiopathic olfactory disease significantly increased the suprathresholds (identification and discrimination). Unlike anosmia, a significant correlation was found between symptoms and suprathresholds (identification-discrimination) in parosmia, because the major complaint of the patients is the perception of odors differently than they actually are.9 The study of Altundag et al. compared the efficacy of COT and MOT in the treatment of post-infectious olfactory disorder. The extension of MOT period from 12 to 24 weeks was found to be more effective for improvement of olfactory function compared to COT; however, no significant difference was found when the therapy was extended to 36 weeks.10 In a study by Whitcroft et al. in which they compared the etiology of anosmia/hyposmia and Sniffin’ Sticks test findings, it was shown that threshold and discrimination in identification were better protected in hyposmia and anosmia due to postviral infection. Another remarkable point in the same study is that it was shown that discrimination scores decrease mostly in Parkinson's disease.19 In this study, we saw that discrimination scores decreased significantly, just like in Parkinson's disease. The decrease in discrimination scores caused by parosmia, which is thought to occur due to neural miss-match during the recovery period after anosmia, may actually indicate that anosmia will turn into parosmia. The decrease in discrimination scores in anosmia patients may be useful in demonstrating the prognosis.
Also, we found that there was a significant increase in threshold and identification scores at the sixth month, the increase in discrimination scores was moderate, and there was no significant mitigation of parosmia complaints in our patients. However, at the end of the ninth month, discrimination scores increased and parosmia complaints of the patients were significantly mitigated (Fig. 2). This result suggests that longer periods of MOT should be applied to improve parosmia compared to anosmia. MOT of 9 months facilitated the adaptation of the patients and increased the discrimination scores of the patients, enabling them to perceive more odors correctly. Prolonged MOT duration may further increase discrimination scores.
There is no proven treatment method for parosmia after COVID-19 infection. The treatment decision between the groups was not made by the physicians and was left to the patient's choice. While some of the patients accepted this treatment, some of them did not want to do it because they found it quite complex and troublesome. What caught our attention was that patients with food-related parosmia were more likely to choose treatment, but we did not evaluate this statistically. The main limitation of this study was that the treatment and control groups were not chosen randomly and left to the patient's preference.
The inclusion of volunteers with parosmia who did not opt in for olfactory rehabilitation in this study is important in terms of demonstrating the efficacy of olfactory rehabilitation (Fig. 3). While some improvement can be observed at the end of the ninth month in the control group, the improvement in the treatment group is significantly better (Figs. 4 and 5).
CONCLUSION
This study presents MOT as an effective treatment modality for post-COVID-19 parosmia. Compared to the treatment of anosmia and hyposmia, the longer duration of olfactory training is the distinctive aspect of this study. Despite the increase in threshold and identification scores in the parosmia patients, symptomatic improvement was not achieved for a while. However, after six months, symptomatic improvement was evident with the improvement in discrimination scores. Moreover, this study may guide new studies on the effectiveness of olfactory rehabilitation in the treatment of parosmia induced by other types of infections rather than COVID-19.