Three-Month Complication Rate of Ultrasound-Guided Soft Tissue Surgical Procedures Across Six Sports Medicine Clinics
We would like to acknowledge the following individuals who contributed to data collection and organization at their respective institutions: Kuntal Chowdhary, MD (Pittsburgh), Stephanie C. Clark, DO, MS (Mayo Clinic), Connor M Fulz, MD (Pittsburgh), Karina Gonzalez Carta, MD (Mayo Clinic), Giorgio Negron, MD (Emory), Jorday Orr, MD (Swedish), Paul Ricci, LAT (Emory), Chelsea Richardson, LAT (Emory), Patrick J. Shaeffer, MD (Mayo Clinic), Lauren Vernese, DO (Swedish).
Abstract
Objectives
To 1) determine the types and frequency of complications within 3 months following ultrasound-guided surgical procedures, and 2) identify any patient demographics, co-morbidities, or procedural characteristics that were associated with an increased risk of complications.
Methods
A retrospective chart review was performed at six Sports Medicine clinics across the United States. The Clavien-Dindo classification was used to categorize procedural complications on a 5-point scale from 1, representing any deviation in post-procedure care without requiring pharmacological or invasive treatment to 5, representing death. Generalized Estimating Equations for binomial outcomes with a logit link were used to estimate the overall and procedure-specific 3-month complication rates.
Results
Among 1902 patients, 8.1% (n = 154) had diabetes and 6.3% (n = 119) were current smokers. The analysis included 2,369 procedures, which were performed in either the upper extremity (44.1%, n = 1045) or lower extremity (55.2%, n = 1308) regions. The most common procedure was ultrasound-guided tenotomy (69.9%, n = 1655). Additional procedures included, trigger finger release (13.1%, n = 310), tendon scraping (8.0%, n = 189), carpal tunnel release (5.4%, n = 128), soft tissue release (2.1%, n = 50), and compartment fasciotomy (1.6%, n = 37). Overall, there was a complication rate of 1.2% (n = 29 complications; 95% CI: 0.8–1.7%). Individual procedures had complication rates that ranged from 0 to 2.7%. There were 13 Grade I complications in 13 patients, 12 Grade II complications in 10 patients, 4 Grade III complications in 4 patients, and 0 Grade IV or V complications. No associations between complication risk and any patient demographics (age, sex, BMI), co-morbidities (diabetes, smoker), or procedure characteristics (type, region) were identified.
Conclusion
This retrospective review provides an evidence-based estimate supporting the low level of risk associated with ultrasound-guided surgical procedures for patients from a variety of geographical settings who are seeking care at private and academic-affiliated clinics.
Abbreviations
-
- USG
-
- ultrasound-guided
-
- DVT
-
- deep vein thrombosis
-
- USGT
-
- ultrasound-guided tenotomy
-
- IRB
-
- Institutional Review Board
-
- GEE
-
- Generalized Estimating Equations
-
- CI
-
- confidence intervals
Soft tissue injuries and conditions represent a significant burden to active and working populations. Trigger finger, carpal tunnel syndrome, and plantar fasciitis, each have a prevalence of 1–4% in the general population and contribute to significant work-related disability.1-3 Soft tissue injury rates are even higher among high-performance athletes. The prevalence of Achilles tendinopathy in ultramarathon runners is ~19%, while patellar tendinopathy affects roughly 45% of professional volleyball players.4, 5 When soft tissue injuries and conditions are recalcitrant to standard conservative care invasive interventions are often considered. Given the relative anatomically superficial nature of the aforementioned conditions and recent advancements in ultrasonography, ultrasound-guided (USG) interventions have increasingly been developed to treat conditions affecting these structures. While initially used primarily for guided injection therapy, more recently USG surgical techniques have been described, including tenotomy and debridement, soft tissue release, and fasciotomy.6-18
USG surgical techniques offer several advantages over open or arthroscopic/endoscopic operative procedures. The precision of ultrasound guidance allows for a less invasive approach which is amendable to being performed using only local anesthesia, thus reducing the risks associated with general or regional anesthesia required for more traditional operative procedures.19 Reduction in operative time likely further decreases risk.20 Moreover, there is reduced cost, since less resources and time are required to perform an USG surgery in an outpatient clinical setting compared with a procedure performed in an operating room.6, 18 Individuals with comorbidities, such as obesity, diabetes, and smoking history, who may otherwise not be candidates for traditional surgical approaches, may also benefit from a less invasive USG approach. With the significantly reduced incision size, minimal soft tissue disruption, and lack of general anesthesia, USG surgery can often be considered despite these co-morbid conditions. While USG surgery has the potential to provide significant benefit to a wide range of patients, the risks of these newer techniques have not been thoroughly evaluated in a large, diverse sample of patients.
Compared with upper extremity USG surgeries, lower extremity USG surgeries may be at a higher risk for deep vein thrombosis (DVT). Two case series have reported severe complications of DVT and tendon rupture following USG tenotomy (USGT) for Achilles tendinopathy.21, 22 In contrast, several studies on USGT for elbow tendinopathy have reported no complications.18, 23-29 Additional complications reported in the literature include superficial wound infections,6, 30, 31 wound rupture,30 hematoma,32, 33 and nerve injury.32, 34 The sample sizes reported are small (n = 2–182) and/or occurred at a single geographical location, which limits ability to capture the full range of possible complications and generalizability of frequency estimates.6, 18, 21-37 A large sample of patients, from multiple physicians, over multiple geographical locations, is needed to more accurately assess the frequency and types of risks associated with USG surgical procedures.
The objectives of this study were to 1) determine the types and frequency of complications within 3 months following USG surgical procedures in a large, geographically-diverse sample, and 2) identify any patient demographics, co-morbidities, or procedural characteristics that were associated with an increased risk of complications across a heterogenous sample of USG surgical procedures. We hypothesized that USG surgical procedures would have a low complication rate and that patients with diabetes, history of smoking, previous steroid injections, and/or lower extremity injuries would have a higher risk of complications.
Methods
A multi-site retrospective review was performed of patients who underwent an USG surgical procedure, with or without concomitant injections, at six Sports Medicine Clinics in the United States between January 2011 and April 2020. Collaborating clinical sites included both academic institutions (N = 4) and private practices (N = 2) as well as a range of geographical regions including the West (N = 1), Midwest (N = 3), South (N = 1), and East (N = 1). All procedures were completed by fellowship trained Sports Medicine Physicians with primary training in Physical Medicine & Rehabilitation or Family Medicine. A total of 11 different physicians performed the procedures across the six sites. The follow-up time points were chosen based on standard of care with routine follow-up visits at 2-, 6-, and 12-weeks after the procedure. A research assistant at each site reviewed the electronic patient records for any complications that occurred within 3-months of the procedure. A researcher and research assistant at the coordinating site reviewed de-identified data from all sites to ensure standardized categorization of complication type and severity. The inclusion criteria of the study were any patient who had an USGT, soft tissue release (including trigger finger and carpal tunnel release), compartment fasciotomy, or tendon scraping over a 9-year period. The exclusion criterion was a lack of any known follow up. The study was approved under a single Institutional Review Board (IRB) to oversee sharing of de-identified data from the collaborating sites to the coordinating site.
Ultrasound-Guided Surgical Techniques
USG surgical procedures included were grouped into four general categories: 1) USGT, 2) Soft tissue release, 3) Compartment fasciotomy, and 4) Tendon scraping. These procedures were chosen based on their common use in clinical practice, the ability to be performed in an outpatient setting, and the minimally-invasive approach of these USG surgical techniques. Given the retrospective multisite nature of the study, procedural techniques were not standardized. However, techniques generally followed previously published approaches while allowing for variation based on individual patient pathoanatomy and physician preference. General technical principles are discussed below.
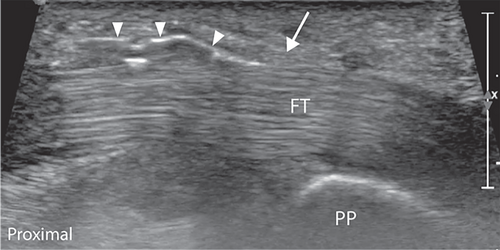
Ultrasound-Guided Tenotomy
Tenotomy is broadly defined as cutting tendon tissue, either completely or incompletely, using a needle, scalpel, or other device.38 Debridement is removal of necrotic or degenerative tissue from a given tissue of the body.38 Various techniques for ultrasound-guided tenotomy (USGT) have been reported in the literature. For this study we did not include those procedures performed with simple needle fenestration alone. All procedures included the use of single or multiple small (~5 mm) incisions for introduction of the cutting device. Debridement of the pathologic tendon tissue was performed in addition to the tenotomy.6, 8, 15, 18, 26 Although multiple devices are currently available to accomplish this procedure, all included USGT procedures were performed with the Tenex Health system (Trice Medical, Malvern, PA). Figure 1 demonstrates a typical USGT procedure performed at the common extensor tendon of the elbow.

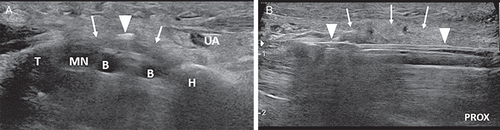
Soft Tissue Release
A soft tissue release involves the cutting of retinacular tissue responsible for stenosis using a needle, scalpel, or other device.38 Trigger finger release specifically involves cutting of the pulley and associated tendon sheath at site of stenosis.38 The majority of soft tissue releases were performed for trigger finger (Figure 2.) followed by carpal tunnel syndrome (Figure 3). Fewer releases were performed in other body regions, but a similar general technique was used (Figure 4).
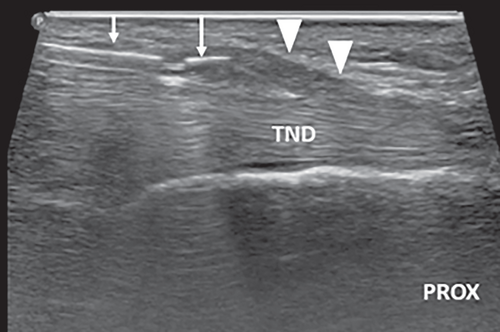
Compartment Fasciotomy (Lower Leg)
Fasciotomy as a treatment for chronic exertional compartment syndrome involves the cutting of the muscular fascia of the involved compartment using a needle, scalpel, or other device.38 Included procedures were performed either using a styletted needle technique or a V-shaped meniscotome.9, 13 Figure 5 demonstrates the meniscotome technique.
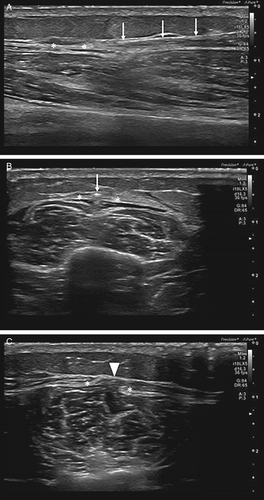
Tendon Scraping
Tendon scraping is the process of abrading the surface of a tendon or paratenon with a needle, scalpel, or other device, with the goal of separating the tendon from neovessels, neonerves, and/or adjacent soft tissues.10, 31, 38, 39 Included indications were Achilles and patellar tendinopathy. The use of high volume (saline) injection in addition to scraping was performed in some cases, but high volume injection alone was not included in this study.
Complications
The Clavien–Dindo classification was used to classify procedural complications. This classification system defines three types of negative outcomes, 1) complications (Table 1), 2) failure to cure, and 3) sequela.40 Complications are divided into a 5-point scale based on the level of treatment required to address the complication. This approach minimizes the subjectivity and potential for down-grading complications and has been shown to be reproducible across multiple centers.41
| Grade | Description of Category | Included Complications |
|---|---|---|
| I | Any deviation from the normal post-procedure course without the need for pharmacological treatment or invasive intervention. Treatments can include therapeutic exercise, ice, or bracing. | Nerve symptoms (no change in care, resolved with time), hematoma, capsulitis, partial tendon tear (treated with boot) |
| II | Requiring pharmacological treatment. | Nerve injury (gabapentin), infection (resolved with antibiotics), allergic reaction, deep vein thrombosis |
| III | Requiring an invasive procedure | Compartment syndrome, infection (requiring irrigation) |
| IV | Life-threatening complication requiring IC/ICU management | NA |
| V | Death of a patient | NA |
Data Collection
Patient characteristics (age, sex, BMI, co-morbidities of diabetes, and current smoker) and procedure-specific factors (type of procedure, level of sterile technique, and injury area) were collected. Complications within 3 months of the procedure were categorized by type: infection requiring antibiotics, tendon rupture, nerve injury, allergic reaction, DVT, compartment syndrome, capsulitis, hematoma, and other.
Statistical Analysis
Descriptive statistics were calculated for continuous data as mean (standard deviation) and for categorical data as percentage (frequency). Generalized Estimating Equations (GEE) for binomial outcomes with a logit link were used to estimate the overall and procedure-specific 3-month complication rates along with their 95% confidence intervals (CI). The GEE models accounted for correlations within site and individuals with multiple procedures. Univariable GEE models were also used to examine if patient demographics (age, sex, BMI), co-morbidities (diabetes, smoker), or region of the procedure (upper vs lower extremity) were associated with an increased risk for complications. Odds ratios and 95% confidence intervals are provided. SAS version 9.4 (SAS Institutes, Cary, NC) was used for all analyses and an alpha level of significance was set at 0.05.
Results
Patient Characteristics
A total of 2500 procedures were performed on 2033 unique patients. Patients without any known follow-up were excluded from analysis (n = 131), resulting in a total of 1902 patients and 2369 procedures for analysis. Patients were typically middle aged (mean = 50.9 years, standard deviation = 14.6), women (57.1%), and overweight to obese (BMI: 29.4 ± 6.3 kg/m2). For co-morbidities, 8.1% (n = 154) had diabetes and 6.3% (n = 119) were current smokers.
Procedure
The most common procedure was USGT (69.9%, n = 1655). Additional procedures included, trigger finger release (13.1%, n = 310), tendon scraping (8.0%, n = 189), carpal tunnel release (5.4%, n = 128), soft tissue release (2.1%, n = 50), and compartment fasciotomy (1.6%, n = 37).
Over 1000 procedures were performed in either the upper extremity (44.1%, n = 1045) or lower extremity (55.2%, n = 1308) regions. The most common regions were the elbow (21.0%, n = 497), Achilles tendon (18.7%, n = 441), plantar fascia (17.5%, n = 414), fingers (13.3%, n = 314). Procedures were also performed in the patellar tendon (9.0%, n = 213), carpal tunnel (5.4%, n = 128), gluteal tendon (4.1%, n = 96), rotator cuff (3.6%, n = 84), hamstring (1.7%, n = 40), lower leg compartment (1.6%, n = 37), quadriceps tendon (1.0%, n = 24), Iliotibial band (ITB) (0.8%, n = 20), first dorsal wrist compartment (0.6%, n = 14), proximal long head biceps tendon (0.3%, n = 8), Hoffa's fat pad (0.3%, n = 7), or other lower extremity with <5 procedures per region (0.7%, n = 16).
The most common form of sterile technique (74.6%, n = 1768) included the use of sterile gloves, disinfectant scrub, sterile gel, and sterile transducer cover. Other less common sterile techniques included: Sterile gloves, disinfectant scrub, sterile gel, sterile transducer cover, gown, cap, face mask (17.2%, n = 408); Sterile gloves, disinfectant scrub, sterile gel, and transducer disinfection without sterile transducer cover (4.2%, n = 99); Sterile gloves, sterile gel, sterile gown, sterile transducer cover (3.6%, n = 85); Sterile gloves, disinfectant scrub, non-sterile gel, transducer disinfection without transducer cover (0.3%, n = 6); and Sterile gloves, disinfectant scrub, sterile gel, face mask, and transducer disinfection without sterile transducer cover (0.1%, n = 3).
Complications
Among 2369 USG surgical procedures there was a complication rate of 1.2% (n = 29 complications; 95% CI: 0.8–1.7%). There were 13 Grade I complications in 13 patients, 12 Grade II complications in 10 patients, and 4 Grade III complications in 4 patients (Table 2). Complications included nerve injury (n = 6), infection (n = 7), DVT (n = 2), gout flare (n = 2), partial tendon tear (n = 1), allergic reaction (n = 1), compartment syndrome (n = 1), adhesive capsulitis, (n = 1), hematoma (n = 1), and other (n = 7). Grade I complications occurred in the upper (n = 5) and lower (n = 8) extremity regions. Grade II complications occurred in the upper (n = 5) and lower (n = 5) extremity regions. Grade III complications occurred in the upper (n = 3) and lower (n = 1) extremity regions. No difference was identified in complication rates between upper and lower extremity procedures (OR: 0.99; 95% CI: 0.46–2.15; P-value = .99). Each procedure had complication rates that ranged from 0 to 2.7% (Table 3). No associations were identified between complication risk and any patient demographics (age, sex, BMI) or co-morbidities (diabetes, smoker) (Table 4).
| Region | Age, Sex, BMI (kg/m2) | Co-Morbidities | Previous Steroid Injections (no) | Sterile Technique | Complication: Time From Procedure to Complication in Weeks and Description |
|---|---|---|---|---|---|
| Grade I | |||||
| USGT | |||||
| Elbow, common extensor tendon | 70, M, 26.4 | Hyperlipidemia, BPH | ≥3 | B | 2, Other (swelling and pain). |
| Elbow, common extensor tendon | 38, F, 30.7 | Smoker | ≥3 | A | 12, Nerve injury (burning pain at lateral elbow). |
| Elbow, common extensor tendon | 51, F, 25.3 | NA | 0 | A | 12, Nerve injury (pain and intermittent numbness of fingers). |
| Gluteal tendon | 72, M, 22.9 | Diabetic | ≥3 | A | 2, Adhesive capsulitis. |
| Patellar tendon | 54, M, 31.9 | Gout | 2 | A | 2, Gout flare. |
| Achilles tendon insertion | 55, M, 22.9 | NA | NR | C | 4, Infection. |
| Achilles tendon insertion | 71, M, 25.8 | NA | 0 | A | 0.4, Pseudogout flare. |
| Plantar fascia | 51, M, 33.5 | Diabetic, former smoker anxiety, depression, HTN, HLD, OSA, thyroid disease | 1 | A | 0, Nerve Injury (numbness along right medial calcaneal branch without pain). |
| Plantar fascia | 48, F, 23.2 | Anxiety | 2 | A | 3, Nerve Injury (superficial peroneal neuritis). |
| Carpal tunnel release | |||||
| Carpal tunnel | 75, F, 26.7 | NA | ≥3 | B | 1, Infection (cellulitis). |
| Carpal tunnel | 53, M, 39.4 | NA | 1 | B | 2.5, Hematoma. |
| Compartment fasciotomy | |||||
| Lower leg compartment | 17, M, 20.7 | NA | 0 | A | 1, Nerve Injury (numbness for 1 week following procedure). |
| Tendon scraping | |||||
| Achilles midportion | 14, F, 25.5 | NA | 0 | A | 1, Other (bruising around ankle and foot). |
| Grade II | |||||
| USGT | |||||
| Elbow, common extensor tendon | 52, F, 19.4 | Breast cancer and chemotherapy 7 years earlier | 2 | A | 3, Other (increased pain at incision site). |
| Elbow, common extensor tendon | 50, F, 32.2 | Cocaine use, former smoker, HTN, chronic pain | 0 | A | 0.3, Allergy (adhesive). |
| Elbow, common extensor tendon | 48, F, 28.9 | NA | 1 | A | 12, Nerve injury (burning pain at lateral elbow). |
| Patellar tendon | 29, M, 25.8 | NA | 0 | A | 8, Other (pain). |
| Patellar tendon | 40, M, 26.0 | NA | 0 | B | 1, DVT. |
| Plantar fascia | 56, M, 27.6 | NA | 0 | B | 6, DVT. |
| Achilles tendon, insertion | 46, M, 41.0 | Hypertension | 1 | B | 2, Infection (superficial). |
| USGT and tendon scraping completed simultaneously. Patient with two grade II complications | |||||
| Achilles tendon midportion, unilateral | 53, F, NR | Seizures, ankylosing spondylitis, type 1 DM and renal cell carcinoma s/p nephrectomy | 0 | B | 1.5, Other (pleuritis). 2, Partial tendon tear. |
| Carpal tunnel release | |||||
| Carpal tunnel, bilateral | 35, F, 34.3 | NA | 1 | A | 6, Other (pain). |
| Carpal tunnel | 75, F, 26.7 | NA | ≥3 | B | 1, Infection (superficial). |
| Grade III | |||||
| USGT | |||||
| Elbow, common extensor tendon | 39, F, 33.0 | PTSD, peripheral neuropathy, chemo for breast cancer, hypothyroid, depression, anxiety, Former Smoker | 0 | A | 0.1, Compartment syndrome. |
| Popliteus tendon | 70, M, 28.7 | NA | 1 | A | 8, Infection (Deep/Prosthetic knee joint). |
| Carpal tunnel release | |||||
| Carpal tunnel | 56, F, 23.1 | Diabetes | 0 | B | 1.5, Infection (Deep). |
| Soft tissue release | |||||
| Middle finger | 63, F, 23.4 | Smoking | 0 | A | 3, Infection (Deep). |
- Note: Sterile technique A = Sterile gloves, area scrubbed, sterile gel, sterile transducer cover; Sterile technique B = Sterile gloves, area scrubbed, sterile gel, sterile transducer cover, gown, cap, face mask; Sterile technique C = Sterile gloves, area scrubbed, sterile gel, and transducer disinfection without sterile transducer cover.
| Procedure | USGT | Carpal Tunnel Release | Tendon Scraping | Compartment Fasciotomy | Soft Tissue Release |
|---|---|---|---|---|---|
| % (95% CI), no. | 1.3% (0.7–1.8), 21/1655 | 2.3% (0.0–5.0), 3/128 | 1.6% (0.0–3.4), 3/189 | 2.7% (0.0–7.9), 1/37 | 0.3% (0.0–0.8), 1/360 |
| Infection | 3 | 2 | 0 | 0 | 1 |
| Partial tear | 1 | 0 | 1 | 0 | 0 |
| Nerve injury | 4 | 0 | 0 | 1 | 0 |
| Allergic reaction | 1 | 0 | 0 | 0 | 0 |
| Deep vein thrombosis | 2 | 0 | 1 | 0 | 0 |
| Compartment syndrome | 1 | 0 | 0 | 0 | 0 |
| Adhesive capsulitis | 1 | 0 | 0 | 0 | 0 |
| Hematoma | 0 | 1 | 0 | 0 | 0 |
| Gout flare | 2 | 0 | 0 | 0 | 0 |
| Other | 6 | 0 | 1 | 0 | 0 |
| Variable | Odds Ratio (95% CI) | P-value |
|---|---|---|
| Sex (men = 0) | 0.94 (0.44–2.01) | .87 |
| Age (years) | 0.99 (0.97–1.02) | .70 |
| BMI (kg/m2) | 1.00 (0.99–1.01) | .99 |
| Diabetes | 2.16 (0.72–6.50) | .17 |
| Smoker | 1.73 (0.53–5.73) | .37 |
Comorbidities and Complication Rates
Within the sample 8.1% (154/1902) of patients had diabetes. Among the 154 patients who had diabetes, 4 patients had a total of five complications (nerve injury, adhesive capsulitis, partial tendon tear, pleurisy, infection). The complication rate was 2.3% (5/204 procedures with two complications occurring in one patient; 95% CI: 0.09–6.2%) for USG surgical procedures in patients with diabetes. Within the sample 6.3% (119/1902) of patients were smokers. Among the 146 patients who were smokers, 3 patients had a total of three complications (2 infections, 1 nerve injury). The complication rate was 2.1% (3/146; 95% CI: 0.7–6.2%) for USG surgical procedures in patients who were smokers.
Additional Procedures or Operations Within 3 Months
Out of the 2369 procedures, 18 (0.8%) required an additional procedure within 3 months. This included a repeat USG surgical procedure due to persistent symptoms (n = 12), the initial procedure having to be aborted due to individual anatomical variations (n = 2), and a subsequent open procedure (n = 4).
Discussion
The objectives of this study were to determine the rate of complications within 3 months following USG surgical procedures and to identify any risk factors associated with a higher complication rate. Consistent with our hypothesis, the 2369 procedures examined in this study had a low complication rate of 1.2% (95% CI: 0.8–1.7%). We failed to detect any patient demographic, co-morbidities, or procedure characteristics that were associated with an increased risk of complications.
The complication rates of the USG surgical procedures examined in this study ranged from 0 to 2.7% depending on the procedure. These rates are comparable to other procedures specific to the upper extremities, including a systematic review that reported complication rates of 2% for open and arthroscopic surgical treatment of lateral epicondylitis and 0% for percutaneous procedures.42 Similarly, endoscopic and open procedures for carpal tunnel release both had low complication rates of 0.2 and 0.5%, respectively.43 In contrast, in the lower extremities, USG surgical procedures may have a notably lower complication rate than traditional surgical techniques. Specifically, the rate of complications with open surgical debridement for Achilles tendinopathy ranges from 6 to over 30%.44-49 The complication rate for plantar fasciotomy surgery has been reported to range from 4.0 to 4.4%.50, 51 Similarly, a review of endoscopic plantar fascia release reported a complication rate of 6.0%, including paresthesias or numbness, soft tissue healing, and superficial infections.52 The overall low complication rate together with a similar number of complications occurring with procedures performed on upper and lower extremities support the safety of USG surgical procedures.
It should also be noted that these procedures were performed by Sports Medicine Physicians in various clinical settings outside of the traditional operating theatre. This data supports the trend of shifting to less invasive surgery in the outpatient setting. USG surgical procedures are cost-effective, well-accepted by patients, and do not appear to sacrifice patient safety. Due to the requisite expertise in ultrasound imaging required to effectively perform these surgical procedures, Sports Medicine Physicians are well placed to safely perform these surgeries in the office setting. Many Sports Medicine fellowships now include these advanced techniques as part of their standard procedural training.53
Strengths and Limitations
The primary strength of this study is generalizability. A large number of patients of varying demographics and comorbidities were included. This represents a real world population from all United States geographical regions for these common musculoskeletal disorders. Furthermore, procedures were performed by multiple physicians with varying techniques and spanning major academic medical centers to private practice settings. Of note, all of the collaborating physicians had a similar level of training on the use of USG surgical procedures either during their fellowship in Sports Medicine or through continuing education courses and had considerable experience with ultrasound guided procedures. Therefore, a limitation is that these findings may not generalize to physicians who have a lower level of training or experience in the use of USG surgical procedures.
A key limitation is that the study is retrospective and depended on patients returning for routine follow-up to be included in the analysis. As a result, 5.2% of cases identified were excluded from analysis due to lack of follow-up. This study includes several different USG surgical procedures that were performed across different regions of the body with different levels of sterile technique. Although we did not correlate any patient or procedural characteristics at higher risk of complication associated with these procedures, no a priori sample size calculation was conducted, and a larger sample size might be needed to detect potential risk factors. Another limitation is that we did not capture the success rate of patients who achieved improvement in symptoms following the procedure. While the current study serves as a first step in determining the safety of ultrasound guided surgical procedures, future research is needed to determine the effectiveness of these techniques using a prospective design with key clinical outcomes assessed before and after the procedure.
Conclusions
This retrospective review of 2369 procedures in 1902 patients, representing variation in demographics, geographical settings, and clinical practices, supports the safety of USG surgical procedures. This is the first large, multisite study that included a variety of USG surgical procedures and captured the complication rate, which ranged from 0 to 2.7% depending on the procedure. Together, USGT, soft tissue release, lower leg compartment fasciotomy, and tendon scraping had a low complication rate of 1.2% (95% CI: 0.8–1.7%). While this dataset is reassuring regarding the safety of USG surgical procedures in the treatment of musculoskeletal conditions, future studies are needed to better assess effectiveness, patient satisfaction, and cost in comparison with traditional surgical techniques.
Open Research
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




