Factors Associated With Prolonged Operative Times in Laparoscopic Right Hemicolectomy and Its Association With Short-Term Outcomes
ABSTRACT
Background
This study aimed to investigate factors associated with prolonged operative time in laparoscopic right hemicolectomy for colon cancer.
Methods
This was a retrospective review of patients with colon cancer who underwent laparoscopic right hemicolectomy between 2011 and 2021. Linear and binary logistic regression analyses were performed to determine factors associated with prolonged operative time. The association between longer operative times and complications and hospital stay was assessed.
Results
One hundred and ninety-seven patients (52.3% female; mean age: 68.8 ± 14.1 years) were included. Factors independently associated with operative time were male sex (β = 17.3, 95% CI: 2, 32.5; p = 0.026) and extended hemicolectomy (β = 67.7, 95% CI: 27.6, 107.9; p = 0.001). American Society of Anesthesiologists (ASA) IV classification had a borderline significant association with operative time (β = 100.4, 95% CI: −2.05, 202.9; p = 0.055). Male sex (r = 0.158; p = 0.026), body mass index (r = 0.205; p = 0.004), ASA classification (r = 0.232; p = 0.001), extended hemicolectomy (r = 0.256; p < 0.001), and intracorporeal vessel control (r = 0.161; p = 0.025) had significant positive correlation with operative times. Patients with operative times ≥ 160 min had significantly longer hospital stays (5 vs. 4 days; p = 0.043) and similar complication rates to patients with shorter operative times.
Conclusions
Male sex, advanced ASA classification, and extended hemicolectomy were independently and significantly associated with longer operative times in laparoscopic right hemicolectomy. Longer operative times were associated with longer hospital stays and similar complication rates.
1 Introduction
Surgery is the standard treatment for locally advanced colon cancer without distant spread. Conventional surgery that involves a laparotomy can be followed by delayed recovery and a high incidence of short and long-term complications. With the advent of minimally invasive surgery, laparoscopic colectomy has gradually replaced open surgery as the standard of care in many hospitals [1, 2]. Laparoscopic colectomy confers several benefits as compared to open surgery. Collective evidence shows that laparoscopic surgery for colorectal cancer is associated with decreased blood loss, shorter hospital stays, and lower rates of postoperative complications and mortality as compared to laparotomy [3]. Moreover, while some surgeons expressed concern about the oncologic safety of laparoscopic surgery in achieving adequate resection of cancer, the collective evidence again shows that laparoscopic colectomy for cancer is oncologically safe and confers similar overall and disease-free survival to open surgery [4].
The safety and benefits of minimally invasive surgery regarding smaller abdominal incisions, less pain, and accelerated recovery are well documented, rendering minimally invasive surgery as part of the enhanced recovery after surgery (ERAS) protocol [5]. However, some limitations of laparoscopic surgery for colon cancer have been identified and include limited motion of straight instruments, two-dimensional imaging, and poor ergonomics for the surgeon [6]. The abovementioned factors may contribute to increased operative times of laparoscopic surgery for colon cancer. A meta-analysis based on publications more than 5 years ago [3] found laparoscopic surgery for colon cancer to be associated with a longer operative time of 40 min compared to open surgery. The increase in operative times in laparoscopic colectomy may be variable as they may be extended for up to 50 min in challenging tumor locations such as splenic flexure cancer [7] and, conversely, operative times may be prolonged to a lesser extent (up to 23 min) in laparoscopic right hemicolectomy as compared to the open approach [8].
Learning about factors associated with prolonged operative times in laparoscopic right hemicolectomy is assumed to help surgeons modify their surgical technique and implement additional measures to avoid exceedingly long operative times that may slow the turnover of cases and affect outcomes. Therefore, the present study aimed to investigate the factors associated with prolonged operative times in laparoscopic right hemicolectomy for colon cancer.
2 Patients and Methods
2.1 Study Design and Setting
This study was a retrospective cohort review of a prospectively maintained IRB-approved (FLA 21-071) database of patients with colon cancer who underwent laparoscopic right hemicolectomy at the Department of Colorectal Surgery, Cleveland Clinic Florida (2011–2021). The study was conducted in compliance with the latest amendment of the Declaration of Helsinki statement for medical research involving human subjects and was reported following the guideline of the Strengthening the Reporting of Observational (STROBE) Studies.
2.2 Selection Criteria
Adult patients of either sex who underwent a successfully completed laparoscopic right hemicolectomy for colon cancer were consecutively included. Patients in whom data on the operative time were missing, patients who underwent an open or robotic-assisted right hemicolectomy or had a reactive conversion, defined as the need for an intraoperative shift from laparoscopy to open surgery either because of an intra-operative complication or an extension of an incision because of operative difficulty, were excluded.
2.3 Management Strategy
Five colorectal surgery attendings performed pure laparoscopic or hand-assisted laparoscopic right hemicolectomy. All patients received mechanical bowel preparation and oral antibiotics before surgery except those operated on in an emergency setting. Using a three-port stepwise technique, mobilization of the colon was laparoscopically completed and an extracorporeal, antiperistaltic, stapled ileocolic anastomoses was created. The choice of surgical approach, selection of the length and height of the GIA stapler, and the type of vessel control were at the discretion of the attending surgeon. The resected specimens were extracted via a small midline incision.
2.4 Data Points
-
Patients' characteristics: age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) classification, diabetes mellitus, and tumor location.
-
The approach and extent of colectomy. Extended colectomy involved resection of parts of the right side of the transverse colon, beyond the hepatic flexure, and ligation of the main stem of the middle colic artery.
-
Length and height of GIA stapler, apical enterotomy closure, and type of vessel control.
-
Operative time, hospital stay, complications, number of harvested lymph nodes, length of resected colon, and resection status.
-
Postoperative complications and disease recurrence.
2.5 Study Outcomes
The primary outcome of the study was the operative time and factors associated with its increase. The secondary outcome was the association between prolonged operative time and short-term outcomes.
2.6 Statistical Analysis
The study entailed a multiple linear regression analysis to determine the significant factors associated with long operative times. A receiver operating characteristics (ROC) curve was used to determine the cutoff for the operative time associated with increased postoperative complications. Patients who had operative times longer than the cutoff were defined as cases and were compared in a binary logistic regression analysis to controls who had shorter operative times.
Statistical analyses were performed using EZR™ (version 1.55) [9], R software (version 4.1.2), and SPSS™ version 23 (IBM crop). Continuous data were expressed as mean and standard deviation when normally distributed or otherwise as the median and interquartile range. Categorical data were expressed in the form of numbers and absolute proportions. Student t-test or Mann–Whitney U test was used to process continuous variables and the Fisher exact test or χ2 test was used for processing categorical data. Factors that had a p value < 0.1 in the simple linear regression analysis were selected to enter a multiple linear regression analysis. Multicollinearity between the predictors included in the model was assessed using the variance inflation factor (VIF); a VIF > 10 implied significant multicollinearity [10]. The correlation between continuous variables was assessed using Pearson correlation coefficient whereas the Spearman rank correlation test was used to assess the correlation between continuous and categorical variables. p Values less than 0.05 were considered statistically significant. A large language model (ChatGPT 3.5, https://chat.openai.com/chat) was used to write an R code for an online calculator that estimates the predicted operative time of laparoscopic right hemicolectomy considering the significant factors identified in the simple linear regression analysis. The R code is available in the Supporting Information S1: File 1. The parameters used for the calculation of the estimated operative time were sex, BMI, ASA classification, tumor location, extent of hemicolectomy, and type of vessel control (intra- vs. extracorporeal).
3 Results
3.1 Patients' Characteristics
After the exclusion of patients with missing operative time data (n = 73), 197 patients with a mean age of 68.8 ± 14.1 years and a mean BMI of 26.9 ± 5.25 kg/m2 were included. Patients were 103 (52.3%) female and 94 (47.7%) male and the majority (97.9%) had ASA II–III classification. Pure laparoscopic colectomy was done in 96.4% of patients, whereas 3.6% underwent a hand-assisted laparoscopic colectomy. Emergency surgery and extended colectomy were performed in 4.6% and 6.6% of patients, respectively. Vascular control was achieved intracorporeally in 67 (34.5%) patients and extracorporeally in 127 (65.5%). The median operative time for the entire cohort was 150 [IQR: 120, 180] min. Complications were recorded in 26.9% of patients 66% were Clavien-Dindo ≥ II. Reoperation was needed in 1.6% of patients (Table 1).
| Factor | Group | Overall |
|---|---|---|
| Mean age in years (SD) | 68.8 (14.12) | |
| Sex (%) | Male | 94 (47.7) |
| Female | 103 (52.3) | |
| Mean BMI in kg/m2 (SD) | 26.9 (5.25) | |
| ASA (%) | 1 | 2 (1.0) |
| 2 | 100 (51.5) | |
| 3 | 90 (46.4) | |
| 4 | 2 (1.0) | |
| TNM stage (%) | I | 65 (33.5) |
| II | 71 (36.6) | |
| III | 58 (29.9) | |
| Surgical approach (%) | Laparoscopic | 185 (96.4) |
| Hand-assisted | 7 (3.6) | |
| Type of surgery (%) | Elective | 187 (95.4) |
| Emergency | 9 (4.6) | |
| Extent of colectomy (%) | Standard | 184 (93.4) |
| Extended | 13 (6.6) | |
| Median operation time in minutes (IQR) | 150 (120, 180) | |
| Complications (%) | No | 144 (73.1) |
| Yes | 53 (26.9) | |
| Reoperation (%) | No | 189 (98.4) |
| Yes | 3 (1.6) | |
- Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index; IQR, interquartile range; SD, standard deviation.
3.2 Factors Associated With Operative Time
3.2.1 Linear Regression
Simple linear regression analysis revealed a significant association among operative time and sex, BMI, ASA classification, tumor location, extent of colectomy, and type of vascular control. Multiple linear regression analysis showed that the significant factors that were independently associated with operative time were male sex (β = 17.3, 95% CI: 2, 32.5, p = 0.026) and extended colectomy (β = 67.7, 95% CI: 27.6, 107.9, p = 0.001). ASA IV classification (β = 100.4, 95% CI: −2.05, 202.9, p = 0.055) had a borderline significant association with operative time. There was no evidence of multicollinearity as the VIF ranged between 1.07 and 1.99 for all examined factors (Table 2).
| Factor | Linear regression | Multiple linear regression | Correlation | VIF | |||||
|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p value | β | 95% CI | p value | r | p value | ||
| Age | 0.26 | −0.31, 0.82 | 0.347 | — | — | — | — | — | — |
| Male sex | 17.1 | 1.36, 32.84 | 0.033 | 17.26 | 2, 32.51 | 0.027 | 0.158 | 0.026 | 1.07 |
| Body mass index | 2.2 | 0.71, 3.69 | 0.004 | 1.30 | −0.23, 2.84 | 0.096 | 0.205 | 0.004 | 1.07 |
| ASA classification | |||||||||
| I | Ref | — | — | — | — | — | 0.232 | 0.001 | 1.19 |
| II | 16.22 | −61.61. 94 | 0.681 | −2.83 | −76.4, 70.7 | 0.940 | |||
| III | 38.23 | −39.7, 116.1 | 0.334 | 10.28 | −64.03, 84.6 | 0.785 | |||
| IV | 105 | −3.98, 213.9 | 0.059 | 100.4 | −2.05, 202.9 | 0.055 | |||
| Tumor location | |||||||||
| Cecum | Ref | — | — | — | — | — | 0.121 | 0.091 | 1.99 |
| Ascending colon | −16.65 | −35.9, 2.6 | 0.089 | −15.9 | −34.44, 2.5 | 0.091 | |||
| Hepatic flexure | 10.84 | −12.9, 34.7 | 0.371 | 3.03 | −19.67, 25.7 | 0.792 | |||
| Transverse colon | 29.78 | 1.7, 57.9 | 0.038 | −6.4 | −40.9, 28.1 | 0.715 | |||
| Appendix | −12.38 | −46.7, 21.9 | 0.478 | −8.3 | −42.2, 25.5 | 0.628 | |||
| Ileocecal valve | 36.78 | −27.4, 101 | 0.260 | 46.6 | −14, 107.1 | 0.131 | |||
| TNM stage | |||||||||
| I | Ref | — | — | — | — | — | — | — | — |
| II | 2.52 | −16.7, 21.75 | 0.795 | — | — | — | — | — | — |
| III | −9.73 | −29.9, 10.5 | 0.343 | — | — | — | — | — | — |
| Hand-assisted | 17.71 | −25.5, 60.91 | 0.419 | — | — | — | — | — | — |
| Extended colectomy | 67.38 | 36.8, 97.97 | < 0.001 | 67.72 | 27.6, 107.9 | 0.001 | 0.256 | < 0.001 | 1.75 |
| Emergency colectomy | 11.5 | −26.6, 49.65 | 0.553 | — | — | — | — | — | — |
| Intracorporeal vascular control | 15.7 | −1.13, 32.5 | 0.067 | 11.9 | −4.1, 27.9 | 0.144 | 0.161 | 0.025 | 1.07 |
| Reinforcing apical enterotomy | 10.87 | −7.12, 28.87 | 0.235 | — | — | — | — | — | — |
| Intraoperative complications | 31.9 | −47.4, 111.2 | 0.429 | — | — | — | — | — | — |
- Note: Bold text in p value columns indicates statistical significance.
- Abbreviations: ASA, American Society of Anesthesiologists; CI, confidence interval; VIF, variance inflation factor.
The online calculator showed that altering modifiable factors associated with operative times can significantly change the predicted operative time. As shown in Figure S1, the estimated operative time for a male patient with a BMI of 40 kg/m2 and ASA IV with hepatic flexure cancer, undergoing extended right hemicolectomy with intracorporeal vessel control is 304 min. Optimizing the patient by weight reduction, improving the medical and functional status to become ASA II class, and performing extracorporeal vessel control were expected to shorten the operative time by 116 min.
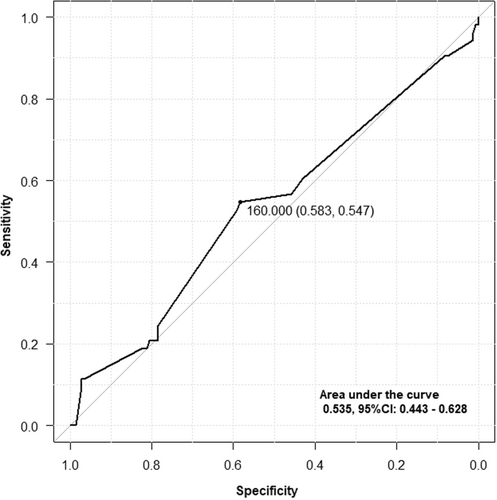
3.2.2 Logistic Regression
Using a ROC curve analysis, a cutoff of 160 min defined the operative time beyond which the incidence of complications increased (Figure 1). The cohort was then divided into two groups (< and ≥ 160 min) according to the operative time cutoff. Consistent with the linear regression analysis, the binary logistic regression analysis showed that patients with operative times ≥ 160 min were more often male (57.3% vs. 39.8%, p = 0.016), had higher BMI (mean: 27.8 vs. 26.1 kg/m2, p = 0.032), more often had ASA III classification (56.3% vs. 38.3%, p = 0.005), and more often underwent extended colectomy (12.4% vs. 1.9%, p = 0.004). In addition, patients with operative times ≥ 160 min presented less often with ascending colon cancers and more often with transverse colon cancers (p = 0.035) (Table 3). Stepwise logistic regression showed that male sex (OR: 2.14, 95% CI: 1.14–4, p = 0.017) and extended hemicolectomy (OR: 1.24, 95% CI: 1.52–100, p = 0.018) were independently associated with operative times longer than 160 min. The AUC of the model was 0.719 (95% CI: 0.647–0.791), indicating a good discriminatory ability of the model used.
| Group | < 160 min (n = 108) | ≥ 160 min (n = 89) | p value |
|---|---|---|---|
| Mean age in years (SD) | 68.15 (14.76) | 69.60 (13.32) | 0.477 |
| Sex (%) | |||
| Male | 43 (39.8) | 51 (57.3) | 0.016 |
| Female | 65 (60.2) | 38 (42.7) | |
| Mean BMI in kg/m2 (SD) | 26.1 (5.0) | 27.8 (5.4) | 0.032 |
| ASA classification (%) | |||
| 1 | 2 (1.9) | 0 (0.0) | 0.005 |
| 2 | 64 (59.8) | 36 (41.4) | |
| 3 | 41 (38.3) | 49 (56.3) | |
| 4 | 0 (0.0) | 2 (2.3) | |
| Tumor Location (%) | |||
| Cecum | 32 (29.6) | 27 (31.0) | 0.035 |
| Ascending colon | 47 (43.5) | 22 (25.3) | |
| Hepatic flexure | 15 (13.9) | 17 (19.5) | |
| Transverse colon | 6 (5.6) | 14 (16.1) | |
| Appendix | 7 (6.5) | 5 (5.7) | |
| Ileocecal valve | 1 (0.9) | 2 (2.3) | |
| TNM stage (%) | |||
| I | 36 (34.3) | 29 (32.6) | 0.067 |
| II | 32 (30.5) | 39 (43.8) | |
| III | 37 (35.2) | 21 (23.6) | |
| Surgical approach (%) | |||
| Laparoscopic | 102 (97.1) | 83 (95.4) | 0.703 |
| Hand-assisted | 3 (2.9) | 4 (4.6) | |
| Type of surgery (%) | |||
| Elective | 104 (96.3) | 83 (94.3) | 0.519 |
| Emergency | 4 (3.7) | 5 (5.7) | |
| Extent of colectomy (%) | |||
| Standard | 106 (98.1) | 78 (87.6) | 0.004 |
| Extended | 2 (1.9) | 11 (12.4) | |
| Type of vascular control | |||
| Extracorporeal | 42 (40.0) | 25 (28.1) | 0.094 |
| Intracorporeal | 63 (60.0) | 64 (71.9) | |
| Reinforcing apical enterotomy (%) | |||
| No | 31 (29.5) | 22 (25.6) | 0.627 |
| Yes | 74 (70.5) | 64 (74.4) | |
- Note: Bold text in p value columns indicates statistical significance.
- Abbreviations: BMI, body mass index; SD, standard deviation.
3.3 Factors Correlated With Operative Time
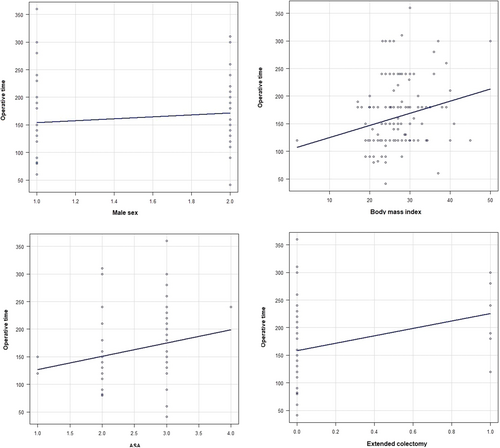
The following factors had a significant positive correlation with operative times: male sex (r = 0.158, p = 0.026), BMI (r = 0.205, p = 0.004), ASA classification (r = 0.232, p = 0.001), extended hemicolectomy (r = 0.256, p < 0.001), and intracorporeal vessel control (r = 0.161, p = 0.025) (Table 2; Figure 2).
3.4 Association Between Operative Time and Outcomes
Operative time had a weak significant positive correlation with estimated blood loss (r = 0.173, p = 0.015), and no significant correlation with hospital stay, total complications, anastomotic leak, ileus, surgical site infection, reoperation, or harvested lymph node number. Patients with operative times ≥ 160 min had significantly longer hospital stays (5 vs. 4 days, p = 0.043) than patients with operative times < 160 min. Otherwise, longer operative times were not significantly associated with overall, major, or individual complications or reoperation (Table 4).
| Factor | Group | Logistic regression | Correlation | |||
|---|---|---|---|---|---|---|
| < 160 min (n = 108) | > 160 min (n = 89) | p value | r | p value | ||
| Complications | Reference | OR: 1.7 (95% CI: 0.9, 3.2) | 0.104 | 0.055 | 0.439 | |
| Complications CD ≥ II | Reference | OR: 1.5 (95% CI: 0.48, 4.7) | 0.488 | 0.164 | 0.24 | |
| Odds of ileus (95% CI) | Reference | OR: 2.2 (95% CI: 0.9, 5.4) | 0.073 | 0.092 | 0.201 | |
| Anastomotic leak | Reference | OR: 0.6 (95% CI: 0.05, 6.7) | 0.676 | −0.049 | 0.498 | |
| Surgical site infection | Reference | OR: 2.1 (95% CI: 0.5, 9.1) | 0.317 | 0.057 | 0.424 | |
| Reoperation | Reference | OR: 0.6 (95% CI: 0.05, 6.7) | 0.678 | −0.049 | 0.493 | |
| Estimated blood loss > 300 ml | Reference | OR: 3.9 (95% CI: 0.8, 20.2) | 0.097 | 0.173 | 0.015 | |
| Median hospital stay in days [IQR] | 4 [3, 6] | 5 [4, 6.25] | 0.043 | −0.03 | 0.675 | |
| Median number of harvested nodes [IQR] | 25 [18.75, 36] | 27 [21, 35] | 0.506 | 0.03 | 0.674 | |
- Note: Bold text in p value columns indicates statistical significance.
- Abbreviations: BMI, body mass index; IQR, interquartile range; OR, odds ratio.
4 Discussion
The present study found male sex, higher ASA classification, increased BMI, and extended hemicolectomy correlated and associated with increased operative times in laparoscopic right hemicolectomy. Longer operative times were not associated with adverse outcomes, except for greater blood loss and extended hospital stay.
Prolonged operative times, while expected in challenging cases, may be associated with negative outcomes. A meta-analysis revealed that the incidence of postoperative complications may increase by 14% for every 30-min increase in operative times [11]. The adverse effect of prolonged operative times may also extend to the surgical team, who may experience fatigue and become more prone to technical errors [12], and to the hospital since a slower turnover of the operating rooms may reduce efficiency and compromise value [13].
Given the consequences of prolonged operative times, we opted to assess the factors associated with longer operative times in right hemicolectomy. The median operating time in our cohort was 150 min, which was 9% less than that (165 min) reported in a systematic review of laparoscopic right hemicolectomy [14]. Factors associated with prolonged operative times can be classified into patient-related and technique-related. Factors related to patients' characteristics were sex, ASA classification, and BMI whereas technical factors involved the extent of resection and the type of vascular control.
Male patients and patients with advanced ASA classes were more likely to have prolonged operative times. Compared to patients with ASA I, patients with ASA IV were more likely to have their operative times prolonged by an average of 100 min. Approximately 60% of patients who had an operative time > 160 min had an ASA III classification. ASA class ≥ 3 was found to be an independent predictor of prolonged operative times in other major surgeries, such as pancreatoduodenectomy [15]. The extended operative times in patients with advanced comorbidities are probably attributable to the additional times taken during the induction and recovery from anesthesia which can be longer than in patients with otherwise no medical comorbidities [16]. Another demographic factor that contributed to longer operative times was male sex. Male patients had longer operative times by an average of 17 min compared to female patients. This observation is perhaps explained by the increased technical difficulty in male patients which may as well predispose to an increased risk of complications in laparoscopic colorectal surgery and longer operative times [17].
BMI was also recognized as an important predictor of extended operative times. Laparoscopic surgery can be technically demanding in patients with obesity. We estimated that for every unit increase in BMI beyond the ideal BMI, the operative time might increase by approximately one and a half minutes. The association of obesity with prolonged operative times in major colorectal surgery has been previously reported [18-20]. The visceral adiposity and thickness of the abdominal wall in patients with obesity may contribute to an increased technical difficulty in laparoscopic colorectal surgery and thus prolonged operative times [21].
In addition to patient characteristics, some aspects of the technique of right hemicolectomy may contribute to increased operative times. Extending resections to include parts of the transverse colon may increase operative times, probably because of the need for additional dissection and mobilization of the colon and ligation of the middle colic vessels. While extended resections may be indicated in hepatic flexure cancers, they are associated with similar rates of local-regional recurrence to standard right hemicolectomy, yet with longer operative times and increased odds of complications [22]. Furthermore, the type of vascular control may affect operative times. Intracorporeal vessel control was associated with longer operative times in simple but not multiple linear regression analysis. Garoufalia et al. [23] reported that intracorporeal vessel control was associated with longer operative times compared to extracorporeal control. Conversely, hand-assisted colectomy and reinforcing the apical enterotomy did not significantly affect the operative times.
Finally, extended operative times were not associated with any major adverse effects on the outcomes of right hemi-colectomy. The exception was a 1-day increase in hospital stay when operative times exceeded 160 min. It has been shown that longer operative times are significantly associated with longer hospital stays in other procedures [24]. The weak association between estimated blood loss and long operative time may be attributed to the increased complexity of the operation since challenging dissections are associated with an increase in both estimated blood loss and operative times.
The present study helps elucidate factors associated with longer operative times in laparoscopic right hemicolectomy. Some of these variables, including technical, may be modifiable. Furthermore, some patient conditions may also be modifiable such as downgrading the ASA class by preoperative optimization of the patients and weight loss [25]. Our online calculator can potenetially help surgeons predict the estimated operative times for patients undergoing laparoscopic hemicolectomy and learn how to shorten the estimated time by optimizing the ASA class, reducing BMI, and/or altering the surgical technique. This tool, contingent validation on a prospective cohort of patients, can prove useful for planning surgery and improving turnover time. Learning that some patients are at high risk of having their surgery prolonged may help in preoperative planning by assessing the need for different intraoperative and postoperative resources [15].
The findings of the study should be cautiously interpreted considering its limitations including the single-center and retrospective nature which is associated with selection bias and may not be generalizable to other hospitals. The small number of patients and the exclusion of patients with missing data may also introduce some selection bias. No robotics procedures were included in the study and it would have been interesting to assess if robotic-assisted is an independent predictor of extended operative times.
5 Conclusions
Male sex, advanced ASA classification, and extended hemicolectomy were independently and significantly associated with operative times in laparoscopic right hemicolectomy. BMI and intracorporeal vessel control were positively correlated with operative time. Longer operative times were associated with longer hospital stays and similar complication rates.
Disclosure
Dr. Steven D. Wexner is a consultant for Baxter, Becton, Dickinson and Co, Glaxo Smith Kline, Intuitive Surgical, Livsmed, Medtronic, OstomyCure, Stryker, Takeda, Virtual Ports, is a member of the Data Safety Monitoring Board of JSR/WCG/ACI (chair), Polypoid (chair), and Boomerang and receives royalties from Intuitive Surgical, Karl Storz Endoscopy America Inc., and Unique Surgical Solutions, LLC. Dr. Sameh Hany Emile is a consultant for Becton, Dickinson, and Company. Drs. Nir Horesh, Zoe Garoufalia, Rachel Gefen, Justin Dourado, and Giovanna Dasilva do not report any financial disclosures.
Open Research
Data Availability Statement
Upon reasonable request from the first author.
References
Synopsis
This retrospective review of a prospective database of patients with colon cancer who underwent laparoscopic right hemicolectomy between 2011 and 2021 found that male sex, advanced ASA classification, and extended hemicolectomy were independently and significantly associated with operative times in laparoscopic right hemicolectomy. BMI and intracorporeal vessel control were positively correlated with operative time. Longer operative times were associated with longer hospital stays but did not increase complication rates.