Changes of acetabular anteversion according to pelvic tilt on sagittal plane under various acetabular inclinations
Abstract
Improper functional orientation of the acetabular cup can result in improper positions when dynamic pelvic positions are not considered. The purpose of this study was to evaluate changes on acetabular anteversion according to pelvic tilt under various acetabular inclinations. Two artificial pelvic models were selected for this study. Acetabular inclinations on the coronal plane were 25°, 32°, 50°, and 60°. Acetabular anteversion of all components were 15°. Changes of anteversion according to pelvic tilt were measured at angles of 0°, 10°, 20°, 30°, and 40°. Computer Navigation, PolyWare 3D pro, CT, and plain radiography were used to measure each angle. The anatomical anteversions against pelvic tilt were calculated using the following formulae: anatomical anteversion (°) = −14.48Χ + 90.18 (inclination angle 25°); anatomical anteversion (°) = −12.26Χ + 80.10 (inclination angle 32°); anatomical anteversion (°) = −7.468Χ + 61.13 (inclination angle 50°); and anatomical anteversion (°) = −5.328Χ + 44.84 (inclination angle 60°) (Χ: pelvic tilt angle). Radiographic anteversion against pelvic tilt were calculated using the following formulae: radiographic anteversion (°) = −9.50Χ + 57.09 (inclination angle 25°); radiographic anteversion (°) = −8.577Χ + 50.89 (inclination angle 32°); radiographic anteversion (°) = −6.794Χ + 45.73 (inclination angle 50°); radiographic anteversion (°) = −5.226Χ + 33.08 (inclination angle 60°). In conclusion, changes in anteversion according to pelvic tilt were lesser at higher degrees of acetabular inclination.
1 INTRODUCTION
Malposition of the acetabular component can cause hip joint instability and promote component wear rate.1-4 Inclination and anteversion of acetabular component in total hip arthroplasty (THA) are important factors in the orientation of the cup. The appropriate position of the acetabular component has been studied as a concept of safe zone investigating the possibility of dislocation by measuring postoperative cup position. From such a study, Lewinnek's safe zone was defined as 40 ± 10° of inclination and 15 ± 10 of anteversion.1 Pierchon et al,5 however, studied the dislocation in 38 THAs and concluded that positions of 11 of 38 cups in hips that had dislocated were placed inside Lewinnek's safe zone. This might be caused by several factors such as the influence of pelvic tilt and a sagittal deformity of the spine. The aging process may lead to an altered sagittal balance, resulting in anterior tilt (where the upper portion of the pelvis tips forward) and posterior tilt (upper portion of the pelvis tips backward).6, 7 Acetabular cup angle which is positioned in accordance with anatomic landmarks alone can also vary between standing and lying positions. Improper functional orientation of the acetabular cup can result in supine and standing positions if the reference is only the bony architecture while dynamic positions of the pelvis are not taken into account.6, 8 These can induce instability even in anatomically appropriately oriented acetabular component. A few studies have verified the effect of pelvis tilt on functional anteversion and inclination of the acetabular cup.9 The impact of pelvic tilt on functional radiographic anteversion is a relatively linear relationship for all values of anteversion when the inclination of the cup is constant. However, changes of acetabular anteversion according to pelvic tilt under various pelvic inclinations have not been reported yet. This study addresses two main questions (a) Which method is the most accurate in measuring real anterversion of the acetabular cup? (b) How does acetabular inclination influence changes of acetabular anteversion according to pelvic tilt? Under the hypothesis that a higher acetabular inclination angle would result in less difference in the acetabular angle according to pelvic tilt, we assessed the relationship between pelvic tilt and acetabular anteversion at various inclination angles. This resulted in acetabular anteversion that was tolerant to dynamic pelvic position.
2 METHODS
2.1 Preparing pelvic model
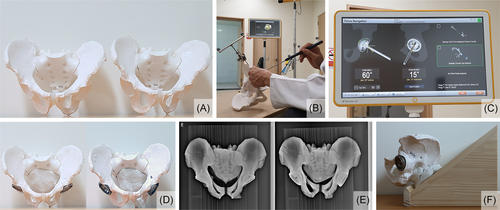
To obtain the effect of inclination angle on anteversion with shifting anterior-posterior pelvic tilt, two male pelvis models were prepared to simulate four hips with different inclination in neutral position (Figure 1A). Pelvic models were attached to backboard neutrally according to anterior pelvic plane. Four half-spherical acetabular cups were inserted into the two male pelvis models (four hips) with a Kick Brain Lab Navigation System (Brain LAB version 2.6, Feldkirchen, Germany) (Figure 1B,C). Four acetabular cups inserted with navigation guide at same anteversion angle (15°) had different inclination angles (25°, 32°, 50°, and 60°) (Figure 1D). Radiographic anteversion and inclination (Murray et al) were measured when undergoing cup fixation with navigation (Figure 1E). Each cup was fixed on pelvic model with two screws. Anteversion angle and inclination were verified again after cup screw fixation. To create sagittal pelvic flexion, we made wood blocks with fixed angles of 10°, 20°, 30°, and 40°. The slope angle is adjustable at 0°, 10°, 20°, 30°, and 40° in the pelvic model to simulate changes in sagittal pelvic tilt (Figure 1F). Adjustable slope that could adjust slope angle with 0°, 10°, 20°, 30°, 40° for the pelvic model was prepared to simulate shifting of sagittal pelvic tilt. We measured the symmetrical pelvic model in various range of angles, and by that, that we think we have minimized the error coming from coronal tilt or axial rotation.
2.2 Obtaining anatomic and radiographic anteversion data
Anatomical anteversion is defined in reference to the angle between a line connecting the lateral anterior and posterior margins of the acetabular component and the sagittal plane. Radiographic anteversion is defined as the angle between the acetabular axis and the coronal plane. Functional cup orientations refers to the position of the cup during functional gait. During gait, the vertical plane of the pelvis is the coronal axis that determines the acetabular orientation. Anteversion on computed tomography (CT) actually reflects anatomical anteversion, whereas anteversion on plain radiographs represents radiographic anteversion. The anatomical anteversion angles were measured by axial CT scans (Figure 2A) and radiographic anteversion angles were measured by Liaw method (Figure 2B). We used the Liaw method to measure the most accurate anterversion of the acetabular cup on the radiograph of each hip. We also used Lewinneck, Widmer, Hassan, and Ackland methods to measure and compare the anteversion of the hip of anteversion 15° and inclination 32° in navigation. Polyware 3D pro. was also used to measure the anteversion (Figure 2C). Version measurements were obtained utilizing two ways. Anatomic anteversion angles of four hips were acquired by CT scan in neutral anterior-posterior pelvic tilt by aligning pelvis with CT scanning axis. Pelvic models were mounted on the adjustable slope and anatomic anteversion angle of each hip was acquired at anterior tilt of 10°, 20°, 30°, and 40° and posterior tilt of 10°, 20°, 30°, 40°. Anteroposterior (AP) radiographs were taken in the supine position with the X-ray beam centered on the superior surface of the symphysis pubis at the same source-to-film distance. Plain AP radiographs of two pelvic models were acquired at neutral position with anterior tilt of 10°, 20°, 30°, 40° and posterior tilt of 10°, 20°, 30°, 40° to obtain radiographic anteversion. Radiologic anteversion of each hip was measured by Liaw method with pelvic AP radiograph.

3 Statistical analysis
All procedures were reviewed and measured by three investigators. Interobserver and intraobserver reliabilities were assessed using intraclass correlation coefficient. All statistical analyses were conducted using SPSS for Windows version 25.0 (SPSS Inc, Chicago, IL). Statistical significance was set at P < .05. The intraobserver and interobserver correlation coefficients for measurement of the acetabular component using the Liaw method were 0.945 (95% confidence interval [CI]: 0.899-0.989) and 0.932 (95% CI: 0.912-0.952), respectively. Intraobserver and interobserver correlation coefficients for measuring anatomic anteversion using CT scan were 0.967 (95% CI: 0.947-0.984) and 0.946 (95% CI: 0.929-0.963), respectively. We used a linear regression analysis to estimate the relationship between pelvic tilt and acetabular anteversion. The least-square method was used to generate formulae that allow for the prediction of acetabular anteversion when given pelvic tilt and acetabular inclination.
4 RESULTS
4.1 Which method is the most accurate in measuring real anteversion of the acetabular cup?
Measured inclinations of each cup which was inserted 25°, 32°, 50°, and 60° of inclination in navigation guide were 25.3°, 32.5°, 48.1°, and 58.8°, respectively. Value by Ackland was closer to navigated one. Values measured by Liaw, Lewinnek were closer to Polyware 3D pro. Anatomic anteversion measured in Axial CT scan was 28.7 ± 0.31°. The equation converting radiographic anteversion to anatomic anteversion was: AV(anatomic anteversion) = tan (tan (RV(radiographic anteversion))/sin (RI(radiologic inclination)). The value measured by Ackland was closer to that measured with CT (Table 1).
| Measuring method | Liaw | Lewinneck | Widmer | Hassan | Ackland | Polyware | CT (AV) |
|---|---|---|---|---|---|---|---|
| Measured anteversion | 13.8 | 13.2 | 21.26 | 11.17 | 14.55 | 13.5 | 28.7 |
| ±0.13 | ±0.09 | ±0.23 | ±0.27 | ±0.57 | ±0.63 | ||
| Converted value by Murray's equationa | 25.68 | 24.55 | 39.55 | 21.38 | 27.08 | 25.84 | ±0.23 |
- Abbreviation: AV, anatomic anteversion.
- a Inclination of cup which inserted at Inclination 32 in navigation Inclination measured on AP radiograph was 32.5° and inclination measured on Polyware 3D was 31.5°.
4.2 How does acetabular inclination influence changes of acetabular anteversion according to pelvic tilt?
4.2.1 Anatomic anteversion shifting according to anterior-posterior pelvic tilt
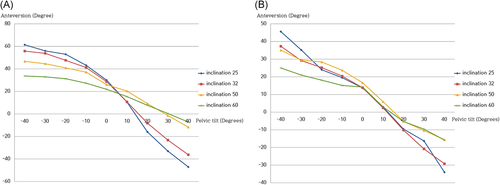
The anatomical anteversion angles were measured by axial CT scans, and anatomical anteversion according to different acetabular inclination and pelvic tilt are presented in Figure 3A and Table 2. In linear regression analysis, anatomical anteversions against anterior pelvic tilt formula were anatomical anteversion (°) = −14.48Χ + 90.18 (at 25° of inclination); anatomical anteversion (°) = −12.26Χ + 80.10 (at 32° of the inclination); anatomical anteversion (°) = −7.468Χ +61.13 (at 50° of the inclination); and anatomical anteversion (°) = −5.328Χ + 44.84 (at 60° of the inclination) (Χ: pelvic tilt angle). The slope was less in the angle of 60°.
| Inclination | ||||
|---|---|---|---|---|
| Pelvic tilt | 25 | 32 | 50 | 60 |
| Posterior 40° | 61.4 | 55.8 | 46.7 | 33.7 |
| Posterior 30° | 56.0 | 53.8 | 44.6 | 32.9 |
| Posterior 20° | 53.0 | 47.6 | 40.9 | 31.3 |
| Posterior 10° | 43.2 | 41.2 | 37.1 | 27.3 |
| 0° | 30.0 | 28.7 | 26.0 | 21.9 |
| Anterior 10° | 10.5 | 10.7 | 20.3 | 15.4 |
| Anterior 20° | −16.0 | −8.2 | 9.2 | 7.7 |
| Anterior 30° | −33.0 | −23.2 | −1.4 | 0.4 |
| Anterior 40° | −47.1 | −36.2 | −11.7 | −7.2 |
4.2.2 Radiographic anteversion shifting according to anterior-posterior pelvic tilt
Radiographic anteversion angles were measured by the Liaw method, and radiographic anteversion according to different acetabular inclination and pelvic tilt are presented in Figure 3B and Table 3. In linear regression analysis, radiographic anteversion against anterior pelvic tilt formula were radiographic anteversion (°) = −9.50Χ +57.09 (at 25° of inclination); radiographic anteversion (°) = −8.577Χ + 50.89 (at 32° of inclination); radiographic anteversion (°) = −6.794Χ + 45.73 (at 50° of inclination); radiographic anteversion (°) = −5.226Χ + 33.08 (at 60° of inclination) (Χ: pelvic tilt angle). The slope was less in the angle of 60°.
| Inclination | ||||
|---|---|---|---|---|
| Pelvic tilt | 25 | 32 | 50 | 60 |
| Posterior 40° | 45.6 | 37.3 | 35.1 | 25.0 |
| Posterior 30° | 35.2 | 29.2 | 29.5 | 21.0 |
| Posterior 20° | 24.0 | 25.2 | 28.4 | 18.1 |
| Posterior 10° | 19.5 | 20.4 | 23.7 | 15.1 |
| 0° | 13.7 | 13.8 | 16.6 | 14.2 |
| Anterior 10° | 2.9 | 2.4 | 5.9 | 3.0 |
| Anterior 20° | −9.6 | −10.2 | −5.2 | −5.3 |
| Anterior 30° | −16.3 | −20.8 | −10.4 | −9.6 |
| Anterior 40° | −34.0 | −29.2 | −15.6 | −15.8 |
5 DISCUSSION
Accurate placement and orientation of the acetabular component is crucial for the prevention of dislocation and component wear. The most commonly used method is radiographic analysis. CT has also demonstrated utility from an axial image of the pelvis.10-24 Anteversion on CT actually reflects anatomical anteversion, whereas anteversion on plain radiographs represents radiographic anteversion. However, the resultant values vary depending on imaging techniques and measurement parameters. Accurate and isotropic data need postoperative evaluation and outcome research. We used a navigation system (Brain LAB version 2.6), PolyWare 3D, plain radiograph's method, and CT for the measurement of acetabular version. Measured inclinations of each cup inserted 25°, 32°, 50°, and 60° of inclination in navigation guide were 25.3°, 32.5°, 48.1°, and 58.8°, respectively. The difference might be an allowable error between navigation and radiograph's measurements. Radiographic anteversions measured by Liaw, Ackland, and Polyware 3d pro were closer to navigated ones. In our study, anteversions measured by Liaw and Lewinneck method were similar to those measured with Polyware 3d pro. This result differs from Park's study that reported the Lewinnek's method was less accurate, with reference to the anteversions obtained from the PolyWare 3d pro.25 Anatomic anteversion measured in Axial CT scan was 28.7 ± 0.31. The value measured by Ackland was closer to the one measured with CT.
The effect of pelvic tilt on acetabular anteversion in THA has been widely recognized.26, 27 In the supine position, the pelvis tilts anteriorly, which decreases anteversion of the acetabular component. In standing position, the reverse happens and the anteversion is increased. In Lemback's study, of 619 hips measured, 8.6% had no anteroposterior pelvic tilt, 40.4% had posterior pelvic tilt of 1 to 9, 12.6% had posterior pelvic tilt of 10 to 25, 33.6% had anterior pelvic tilt of 1 to 9, and 4.8% had an anterior pelvic tilt of 10 to 20.28 This condition might happen in patients with altered spinal sagittal deformity due to the aging process or other causes. Lordosis of the lumbar spine leads to anterior tilt, whereas kyphotic spine leads to posterior tilt. This suggests that the acetabular cup positioned at the time of surgery can change and move because of pelvic rotation after THA.29-31 This is a reasonable explanation regarding why an anatomically oriented cup may be functionally proven to be wrongly oriented, thus favoring subsequent dislocations. Therefore, it is necessary to investigate the most tolerable acetabular version on changes of these dynamic conditions. Joseph et al9 have reported that the impact of pelvic tilt on functional radiographic anteversion has a relatively linear relationship with all values of anteversion, with a mean 0.74° increase in functional anteversion for each degree increase in tilt when the inclination of the cup is 40°. The functional anteversion for each degree increase in pelvic tilt will increase with an increase of static anteversion. In the present study, changes of acetabular anterversion under the various inclinations and constant static anteversion were investigated. In our study, the anatomical anteversion of a steep cup was more tolerable to pelvic tilt.
This study has several limitations. First, acetabular anteversion was constant in our study. Functional anteversion according to pelvic tilt increase with an increase of the static anteversion is already known. Second, the small sample size of our study may be a problem. However, to reproduce precise pelvic tilt angle, we used a custom-made wood block (Figure 1A) with slopes of 10°, 20°, 30°, and 40°. After placing the artificial pelvis on the woodblock, three physicians measured the values three times each. Observing trends of changes of acetabular anteversion according to pelvic tilt on the sagittal plane under several angles of the acetabular inclination can force to the conclusion of our study. Third, we did not study combined anteversion. A safe zone of combined anteversion of the stem and cup has been repetitively defined as 25° to 45°, lower in men but higher in women.15, 32-34 Acetabular version, however, is more sensitive in instabilitiy and impingement than femoral version. Fourth, our study recommends that higher inclination cup for the prevention of dislocation from changes of acetabular anteversion according to pelvic tilt on sagittal plane is appropriate in THAs of patients with spinal deformities on sagittal plane. Placing the acetabular component at higher inclination could lead to impingement, dislocation, and increased wear.1, 35-38 Recently, wear debates can be solved by improvement of the bearing surface. An artificial large head in THA may also overcome issues of impingement and dislocation. Lewinnek et al. have determined the safe zone based on a radiographic technique that positions the patient parallel to the anterior pelvic plane. Lots of dislocations developed in acetabular components that were placed inside Lewinnek's safe zone. The orientation within Lewinnek's safe zone of static cup may not play a major role in the dislocation after THA. An artificial large head as a bearing surface changes the component-to-component impingement into bone-to-bone impingement after THA. It also buffers debatable issues on impingement and dislocation. The definition of Lewinnek's safe zone has to be changed and reintroduced for an artificial large head.
Unpredictable real dynamic pelvic position due to soft tissue tension and contracture, and changes in the exact pelvic position due to soft tissue traction for surgical view may cause minor degrees of malposition of pelvis. This may cause difficulty in precisely inserting the acetabular cup into a planned degree. Also, postoperative pelvic tilt may differ due to several factors, including different soft tissue tension during dynamic positions such as standing, sitting, and lying. For these cases when acetabular anteversion is unpredictable, studies on positioning of the acetabular cup with forgiveness on pelvic anteroposterior tilt may be noteworthy.
Dislocation after THA is a serious complication that causes numerous problems. The fact that 1/3 of all dislocations occur at the Lewinnek safe zone may lead surgeons to doubt the accuracy of intraoperative cup positioning. Several factors, including soft tissue relaxation during anesthesia, accurate lateral decubitus positioning, pelvic tilt due to abnormal spinal sagittal balance, and differences in acetabular cup angle according to body posture, contribute to hip joint stability after THA. The acetabular cup angle, which is most tolerant to differences, may be significant. Our study suggests that a relatively higher inclination of acetabular cup is recommended for THA of patients with spinal deformities on sagittal plane. It is important for surgeons to be aware of this. The cutoff value of the acetabular inclination angle has not been studied in view on the dislocation after THA with an artificial large head as a bearing surface. It needs to be determined in future studies.
AUTHOR CONTRIBUTIONS
MRC designed the study and supervised the project. WKC and SHJ performed the experiments and simulations. SKS analysed the data. HCK and THK wrote the paper with input from all authors. All authors discussed the results and contributed to the final manuscript.