Slow–fast atrioventricular nodal reentrant tachycardia mimicking junctional tachycardia following atrial extrastimulation
Graphical Abstract
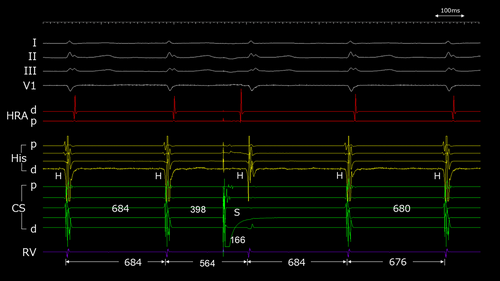
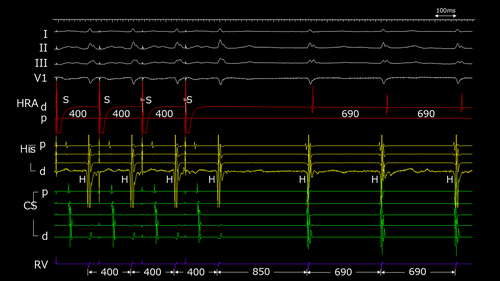
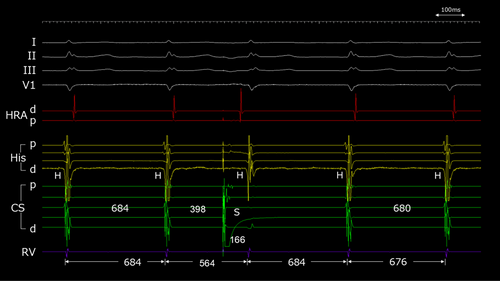
A 51-year-old woman with no comorbidities underwent electrophysiological study (EPS) because of symptomatic narrow QRS tachycardia. The tachycardia was regular with a relatively slow heart rate of around 100 beats per minute, characterized by P waves appearing simultaneously or fused with the QRS complexes. The baseline atrio-His (AH) and His-ventricular (HV) intervals were 70 and 51 ms, respectively. The anterograde atrioventricular (AV) conduction exhibited dual AV nodal physiology, while retrograde conduction was limited to the fast pathway. A narrow QRS complex tachycardia with a cycle length (CL) of 690 ms was induced by burst pacing from the high right atrium (HRA) with a pacing CL of 400 ms, without significant prolongation of the AH interval (Figure 1). The earliest atrial activation was recorded at the proximal His bundle electrodes, which almost coincided with the onset of the QRS complex. When an atrial extrastimulus was applied from the distal coronary sinus (CS) with a coupling interval of 398 ms during tachycardia with a CL of 684 ms, the subsequent ventriculo-ventricular (VV) interval shortened to 564 ms without terminating the tachycardia. The return cycle remained at 684 ms, which was identical to that of tachycardia CL (Figure 2). This finding suggested a diagnosis of junctional tachycardia (JT).
This case presented with a supraventricular tachycardia (SVT) with a short ventriculo-atrial (VA) interval at a heart rate of around 100 beats per minute, and generally, the differential diagnoses include junctional tachycardia (JT), atrioventricular nodal reentrant tachycardia (AVNRT), atrial tachycardia (AT), and atrioventricular reciprocating tachycardia (AVRT). Given the slow rate of the tachycardia, if it were not JT, there must have been very slow anterograde AV conduction during the tachycardia. The postpacing interval during right ventricular entrainment pacing was 173 ms longer than the tachycardia cycle length, and tachycardia was not reset by a single extrastimulus from the right ventricular apex during His refractoriness, ruling out AVRT and nodoventricular/nodofascicular orthodromic reciprocating tachycardia (not shown). Moreover, the tachycardia reinitiation pattern after entrainment pacing from the right ventricle followed an atrial-ventricular (A-V) pattern, which made atrial tachycardia unlikely. Therefore, slow–fast AVNRT or JT was considered in this case.
A premature atrial complex (PAC) delivered at different phases of the tachycardia cycle has been reported to be useful in differentiating slow–fast AVNRT from JT.1 If a PAC timed during the His refractoriness advances the next ventricular excitation, it indicates that the anterograde pathway is the slow pathway, and the diagnosis of AVNRT is confirmed. Conversely, if an earlier PAC advances His immediately after pacing without terminating the tachycardia, it indicates that the fast pathway is available for anterograde conduction and is not essential for maintaining tachycardia as a retrograde pathway, without excluding the possibility of JT. In this case, following an atrial premature stimulation, the QRS complex was advanced with an AV interval of 166 ms, indicating the presence of anterograde fast pathway conduction (Figure 1). While typical responses in slow–fast AVNRT often lead to tachycardia termination, since the tachycardia did not terminate in this case, the possibility of JT needs to be considered. Indeed, when the coupling interval of the atrial extrastimulus was shortened from the tachycardia CL and a PAC was delivered during His refractoriness, the ventricular excitation one beat after the PAC was advanced, which is the characteristic response observed in slow–fast AVNRT (Figure 3A). Interestingly, with further shortening of the coupling interval, both the immediate and the one-beat-later ventricular excitations were advanced, and the tachycardia persisted (Figure 3B). Although this phenomenon may be observed in JT, the coexistence of this response with the typical slow–fast AVNRT findings lacks mechanistic consistency.
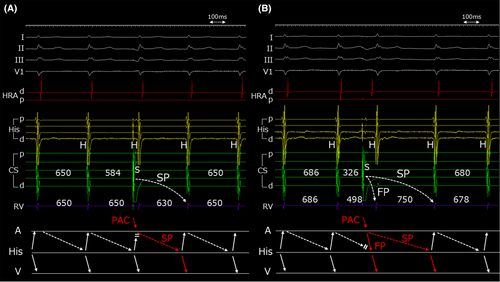
To investigate this case more thoroughly, a detailed inching through the intracardiac electrogram revealed that the tachycardia was induced by a double ventricular response (Figure 1). Furthermore, to clarify the relationship between atrial coupling intervals and the advancement of the VV interval, the ΔVV interval is plotted in Figure 4. Delta V1 represents the prematurity of ventricular excitation immediately after atrial stimulation, and Delta V2 is that of one beat after stimulation. Because of the differing decremental properties of the fast and slow pathways, there are instances, as seen in Figure 2 with a coupling interval of 398 ms, where the interval between the ventricular excitation immediately following the PAC through the fast pathway and the excitation one beat later through the slow pathway matches the tachycardia cycle length. This relationship is demonstrated by the intersection of the ΔV1 and ΔV2 lines. This could lead to a misdiagnosis of JT if not carefully interpreted. Therefore, it is crucial to continuously evaluate and progressively shorten the coupling intervals.
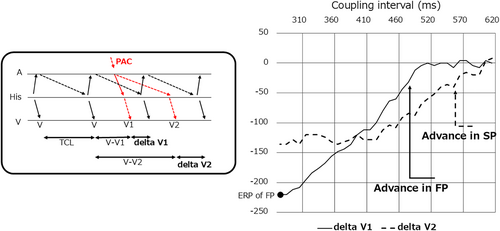
In this case, the prominent decremental property of the slow pathway may explain why the tachycardia did not terminate, even though the early PAC advanced the tachycardia via anterograde fast pathway conduction. This suggests that during the slow conduction through the slow pathway, the fast pathway was able to recover from its refractory period, thereby allowing the reentrant circuit to be maintained. Moreover, owing to the differing decremental conduction properties of the slow and fast pathways, the subsequent VV interval matched the tachycardia cycle length depending on the timing, making it difficult to differentiate from JT in some cases. Based on these findings, the patient was finally diagnosed with slow–fast AVNRT, and anatomical slow pathway ablation was performed. Following the procedure, tachycardia could no longer be induced.
ACKNOWLEDGMENTS
I express my deepest appreciation to my coauthors and the patient.
FUNDING INFORMATION
The authors received no specific funding for this work.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
PATIENT CONSENT STATEMENT
The patient gave written informed consent for the ablation procedures and approved the publication of case details and images in this report.
Open Research
DATA AVAILABILITY STATEMENT
Available upon reasonable request.