Impact of baseline-pool local impedance on lesion formation using a local impedance-sensing catheter: Lessons from a porcine experimental model
Abstract
Background
Impact of baseline-pool local impedance (BP-LI) on the lesion size remains unclear.
Methods
Lesion size in the porcine left ventricular myocardium was evaluated using the STABLEPOINT™ catheter across various ablation settings and BP-LIs (100, 140, and 180 ohms).
Results
A total of 184 lesions were created with different durations (15/30/60 s) at 30 watts or with different powers (30/40/50 W) for 15 s. Lesion depth became deeper (2.8/3.0/3.6 mm at 15 s; p = .007, 4.0/4.9/4.6 mm at 30 s; p = .004, and 5.9/5.5/5.2 mm at 60 s; p = .710) and lesion width wider (5.8/6.3/7.6 mm at 15 s; p = .002, 7.0/8.9/8.9 mm at 30 s; p < .001, and 10.5/9.4/10.5 mm at 60 s; p = .262) as the BP-LI increased under 30 W. Similarly, the lesion depth became significantly deeper (2.1/3.4/3.7 mm at 30 W; p < .001, 3.5/4.6/4.6 mm at 40 W; p < .001, and 4.1/4.7/5.2 mm at 50 W; p = .002) and lesion width broader (5.1/6.9/7.0 mm at 30 W; p < .001, 7.0/7.9/8.1 mm at 40 W; p = .004, and 7.7/8.2/9.6 mm at 50 W; p < .001, respectively) as the BP-LI increased with a 15-s ablation. The relationship between the LI drop and lesion size varied with the different BP-LIs. Adjusted %LI drops (absolute LI drop divided by the BP-LI) minimized the differences between the LI values and lesion formation among the three BP-LIs.
Conclusion
Lesion size decreased with lower BP-LI, and the relationship between the LI drops and lesion formation varied across the different BP-LIs. Adjusted %LI drops may serve as a more reliable parameter for predicting the lesion formation.
1 INTRODUCTION
Impedance is one of the essential parameters for estimating lesion formation during radiofrequency (RF) catheter ablation. Historically, the generator impedance (GI) has been utilized, although it is affected by several non-cardiac factors.1 Recently, catheters capable of measuring the local impedance (LI), such as the IntellaNav MiFi™ OI and STABLEPOINT™ catheters (Boston Scientific, Maple Grove, MN, USA), have been introduced. Those devices allow for predicting the lesion size through the changes in the LI.2-6 Further, the LI is also a surrogate marker of the catheter-tissue contact, which is beneficial when using the MiFi OI catheter that lacks a contact force (CF) sensing module. The tissue contact of the catheters can be inferred by the change in the LI from the baseline LI,7 and the lesion formation is speculated by the LI drop during RF applications.2-5 The baseline-pool LI (BP-LI), also referred to as the blood pool LI, affects all LI parameters; however, they differ among each patient because they are affected by several factors, such as blood impedance. In this study, we evaluated the impact of the BP-LIs on the lesion size and the relationship between the BP-LIs and lesion formation in a porcine experimental model.
2 METHODS
2.1 Experimental setup
We purchased freshly sacrificed (within 48 h) porcine left ventricles for the experiment. The experimental apparatus and setup details have been previously described in our previous publications.4, 8 Briefly, a saline water bath was prepared at 37°C using a thermostatic system (Thermo-Mate BF-400, Yamato Scientific Co., Ltd., Japan). Salt concentration was adjusted to replicate the pre-fixed baseline LI, mimicking blood pool LI. Since the BP-LI with saline could change during the entire experiment, the salt and water were added if needed, especially when influenced by the RF-irrigation with 0.9% saline. The saline solution was circulated at a flow rate of 5 L/min to stimulate blood flow. The STABLEPOINT™ catheter was aligned on the myocardial tissue at a vertical axis with a CF of 10 g.
2.2 Experimental protocol
We set the BP-LI at 100, 140, and 180 ohms. To evaluate the time-dependency and power-dependency, we performed two separate protocols: (1) a time-fixed protocol in which the RF duration was set at 15 s, and (2) a power-fixed protocol in which the RF power was set at 30 watts. At least 10 lesions were performed in each setting.
2.3 Evaluated parameters
The value of the LI drop during the RF application was evaluated. For the evaluation of the lesion size, the lesion depth (LD), maximum width (MW), and surface width (SW) were evaluated for each RF application.
2.4 Relationship between the LI drop and lesion size
According to the different BP-LIs, the relationships between the LI drop and lesion size were also evaluated, and regression analyses were performed.
2.5 Statistical analyses
Data are presented as the mean value ± standard deviation. Continuous variables were analyzed using an unpaired t-test or Kruskal-Wallis analysis when applicable. A two-sided p-value of <.05 was considered statistically significant. All analyses were conducted using JMP Pro 17.0 software (SAS Institute Inc., Cary, NC, USA).
3 RESULTS
3.1 Lesion formation under different BP-LIs
In this study, 184 RF lesions were created, as shown in Figure 1. A steam-pop phenomenon was observed in three sets of lesions with BP-LIs of 180 ohms (two lesions during a 60-s ablation with a 30 W power-fixed protocol and one during a 50 W ablation with the 15-s time-fixed protocol), and those were excluded from the lesion size measurements.
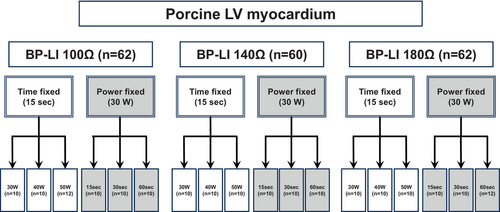
Figure 2 demonstrates a representative lesion formation. The left panel shows the sites where the lesion sizes were measured. The right panels display the lesions formed under different settings. More extensive lesions were observed with higher BP-LIs in both protocols.
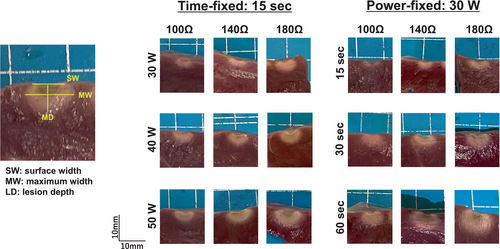
Figure 3 shows the summarized data of the lesion sizes for the time-fixed protocol. The LD (left), MW (middle), and SW (right) are shown. As the BP-LI increased during the 15-s ablation, the LD significantly increased (2.1 vs. 3.4 vs. 3.7 mm at 30 W; p < .001, 3.5 vs. 4.6 vs. 4.6 mm at 40 W; p < .001, and 4.1 vs. 4.7 vs. 5.2 mm at 50 W; p = .002) and the MW became broader (5.1 vs. 6.9 vs. 7.0 mm at 30 W; p < .001, 7.0 vs. 7.9 vs. 8.1 mm at 40 W; p = .004, and 7.7 vs. 8.2 vs. 9.6 mm at 50 W; p < .001, respectively).
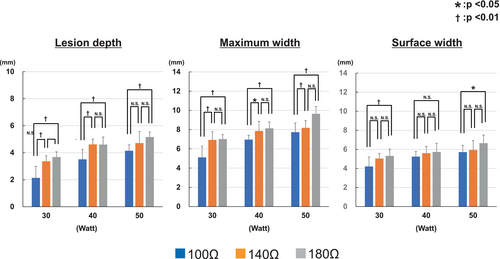
Figure 4 shows the summarized data for the power-fixed protocol, featuring the same parameters as in Figure 3. The LD increased with higher BP-LIs with a shorter ablation time (2.8 vs. 3.0 vs. 3.6 mm at 15 s; p = .007, 4.0 vs. 4.9 vs. 4.6 mm at 30 s; p = .004) but exhibited no significant differences for the 60-s RF applications (5.9 vs. 5.5 vs. 5.2 mm at 60 s; p = .710, with 100, 140, and 180 ohms, respectively). Similarly, the MW became wider with 15- and 30-s ablations as the BP-LI increased (5.8 vs. 6.3 vs. 7.6 mm at 15 s; p = .002, 7.0 vs. 8.9 vs. 8.9 mm at 30 s; p < .001), however the differences were not significant in the 60-s ablation (10.5 vs. 9.4 vs. 10.5 mm; p = .262, with 100, 140, and 180 ohms, respectively).
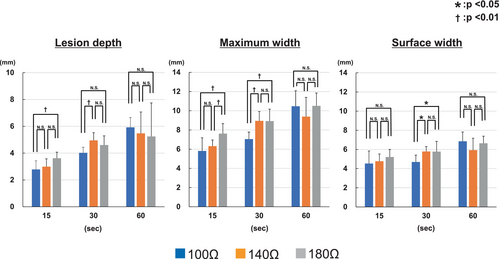
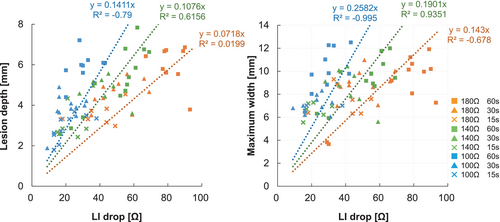
Figure 5 demonstrates the relationship between the lesion size (left: LD, right: MW) and LI drop during the RF applications in the time-fixed protocol. The values of the LI drop were distributed differently among the various BP-LI settings. The absolute values of LI drop were larger with the 180-ohm setting. A linear regression was plotted for each BP-LI group and exhibited high correlation coefficients (LD: R2 = .9619, .9533, .9213 in 180, 140, and 100 ohms, MW: R2 = .9524, .9402, .9176 in 180, 140, and 100 ohms, respectively). That analysis suggested that the relationship between the LI drop and lesion size varied depending on the BP-LI. For example, to achieve a lesion depth of 4 mm, an LI drop of 55.2 ohms would be required for the 180-ohm setting, compared to 21.6 ohms for the 100-ohm setting.
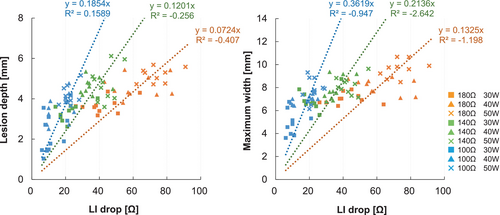
Figure 6 illustrates the relationship between the LI drop and lesion size (left: LD, right: MW) with the power-fixed protocol, which was similar to the findings in the time-fixed protocol (Figure 5). The regression lines for the LD and MW differed across the three BP-LI settings. To create a lesion with a depth of 4 mm, an LI drop of 55.7 ohms was necessary for the 180-ohm setting, while 28.3 ohms were needed for the 100-ohm setting.
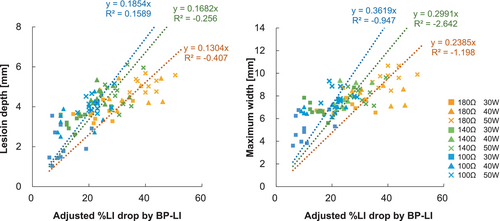
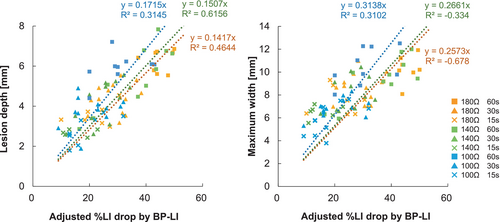
We additionally evaluated the relationship between the adjusted %LI drop and lesion size for the time- and power-fixed protocols. The adjusted %LI drop was calculated as the LI drop divided by each BP-LI. Figure 7 shows the relationship between the adjusted %LI drop and lesion size for the time-fixed protocol. Compared to the data in Figure 5, the difference in the slope of the linear regression analysis for each BP-LI became smaller for the LD and MW. Likewise, Figure 8 demonstrates the relationship between the adjusted %LI drop and lesion size for the power-fixed protocol. The slope of the linear regression analysis for this protocol also became more similar.
4 DISCUSSION
In this study, we evaluated the impact of the BP-LI on lesion formation using LI-sensing catheters and revealed the following findings. (1) The lesion size became smaller under lower BP-LI conditions for all three power settings with the 15-s time-fixed protocol. (2) Likewise, the lesion size became smaller under lower BP-LI conditions with the 30 W power-fixed protocol with a shorter ablation time. (3) However, the lesion size was comparable for all three BP-LIs with a longer ablation time for the power-fixed protocol. (4) The relationship between the LI drop and lesion size varied across the three different BP-LIs. (5) The adjusted %LI drop minimized the difference in those relationships, suggesting that adjusted %LI drops could be beneficial for predicting lesion formation using the LI parameters.
4.1 Importance of the impedance and its meaning
The impedance is a crucial parameter for creating lesions with RF catheter ablation.9 The GI has been utilized as a surrogate marker to assess the lesion creation.10 A decrease in the GI is associated with the RF lesion size, and an excessive decrease suggests excessive tissue heating, leading to a steam-pop phenomenon. A higher baseline GI is also a risk for steam-pops during RF applications because a higher impedance causes a more extensive lesion creation with higher resistive heating. However, the value of the change in the GI is relatively imprecise11; therefore, predicting the lesion size and those complications with only the GI change has been challenging.12
In this regard, the LI-sensing technology (DIRECTSENSE™: Boston Scientific, Maple Grove, MN) has emerged, enabling more precise detection of the impedance changes at the distal tip of the ablation catheter. This technology provides more “local” information. The LI also serves as a valuable alternative to the CF sensing module by increasing the LI when using the MiFi™ OI without the CF module.7
Several parameters are crucial for predicting an effective lesion formation based on the LI values.12 The BP-LI value impacts all LI parameters; however, it varies among patients. The GI is influenced by the tissue between the catheter tip and the body patch, including the blood, fat, and other organs. Conversely, the LI is highly influenced by the blood concentration because it is measured only between two electrodes where blood is present. Therefore, the BP-LI can vary based on the patient's blood concentration (i.e., hematocrit).
Theoretically, resistive heating occurs in areas with relatively high tissue resistance during RF applications.9 Even though the catheter tip that delivers the RF energy is in contact with the myocardium, the electrode surface is also covered in the surrounding blood. As the blood has a lower impedance than the myocardium, more RF current is delivered toward the side in contact with the blood. Therefore, if the blood impedance is lower than usual, the RF current delivered to the myocardium becomes less because it is shunted toward the side in contact with the blood. Concerning this issue, this study demonstrated the impact of the different BP-Lis when simulating the effect of the different blood concentrations on the lesion formation and revealed that a lower BP-LI (mimicking a lower hematocrit) was associated with a smaller lesion formation (Figures 3 and 4).
The actual lesion size increased with higher BP-LI both in the time-fixed (Figure 3) and power-fixed (Figure 4) protocols, although this increase was not significant in the 60-s power-fixed ablation (Figure 4, right-side bars in each graph). In general, lesion size tends to increase as ablation time extends; however, there is a plateau beyond which further enlargement of the lesion size is minimal. From this perspective, lesion formation under 180 ohms of BP-LI appeared to reach this plateau, while lesion size under 100 ohms of BP-LI continued to increase in a time-dependent manner, leading to the insignificant differences observed in the 60-s ablation. This suggests that BP-LI might also influence the time-dependent characteristics of lesion enlargement, such as the plateau points of lesion formation.
4.2 Lesion formation by catheter ablation and the impact of the LI
Regarding lesion formation, technological advances such as the contact force (CF) sensing,13 force-time-integral (FTI),14 ablation index15 (AI: CARTO system, Biosense Webster, CA), and lesion size index16 (LSI: EnSite system, Abbott, MN) have contributed to a more effective lesion creation and have improved the clinical outcomes.17 However, those parameters are “giver-side” parameters, meaning they do not include the information about the myocardium as the “taker-side.”
Regarding this issue, the LI could give us the tissue information. The value of the LI is affected by tissue resistance; therefore, the value of the LI differs when the catheter is in contact with either healthy myocardium or scar tissue. Moreover, the LI is highly dependent on the tissue temperature. During the RF application, the LI decreases as the tissue temperature rises; therefore, the LI drop could speculate an effective tissue temperature rise because tissue degeneration occurs when the tissue temperature rises above 50 degrees Celsius.18 We previously reported the relationship between the lesion size and LI drop with different settings3-5 and reported that a lower LI drop was associated with a gap formation during the pulmonary vein isolation.12 Further, previous reports have suggested that the LI drop is superior to the FTI in predicting the lesion size using the MiFi™ OI7 and STABLEPOINT™ catheters19; therefore, the LI drop is a unique parameter focusing on the local tissue information as a taker-side parameter rather than the ablation settings as giver-side parameters.
However, as discussed above, the LI parameters depend on the BP-LI. The value of the LI drop might change based on the BP-LI. Regarding this issue, the relationship between the LI drop and lesion size varied significantly across the different BP-LI conditions (see Figures 5 and 6). The absolute value of the LI drop alone could not predict the lesion size accurately. Therefore, caution should be taken when assessing the lesion formation only by the absolute LI drop. Regarding this point, we adjusted the data of the LI drop divided by the value of BP-LI and revealed that the difference in the relationship between the adjusted %LI drop and lesion formation among the three BP-LIs became smaller (Figures 7 and 8).
Takigawa et al. reported20 the incidence of pop phenomenon under the different BP-LI conditions in a similar experimental model. They evaluated the lesion formation based on varying power settings, CF, RF duration, and catheter angles. In contrast, we focused specifically on the impact of BP-LI using pre-set power and a 15 s-duration. The results were consistent despite some differences in the lesion formation, probably due to the difference in experimental models or the differences in CF in each experiment. From a biophysical perspective, lower BP-LI results in narrower and shallower lesions because energy currents tend to disperse more into the surrounding saline rather than being directed toward the myocardium. At the lower BP-LI, the RF current is more easily dispersed to the saline. Interestingly, lesions reported in their study were smaller in the horizontal axis, but larger in the vertical axis. The possible cause of different lesion creation between their study and ours could be the difference in CF between the two experiments. Higher CF may cause the catheter tip to be positioned deeper into the tissue, thereby increasing the contact surface area with the myocardium. Additionally, the irrigation holes on the side of the catheter may cool the lateral tissue, potentially leading to a smaller lesion in the horizontal axis and a larger lesion in the vertical axis. Therefore, CF might influence lesion dimensions even under the same BP-LIs. Another factor worth considering is the position of an indifferent ground patch/electrode. In our study, the dispersive patch was positioned at a distant location in the water bath. Although the exact position of the dispersive patch was not detailed in Takigawa's study, this could have influenced the direction of lesion formation in relation to the RF current directions. Furthermore, while the surface lesion area appeared larger at lower BP-LI, the total lesion volume was greater at higher BP-LI in their study. These findings suggest that the biophysical theory aligns with the results observed in our study.
Takigawa et al. also introduced an adjusted LI, using the LI data with catheter-tissue contact (LI value just before RF application, referred to as the initial LI). They concluded that adjusted LI drops by the initial LI were well-correlated with lesion size compared to actual LI drops. In this study, we used the BP-LI to adjust LI drop to estimate lesion sizes because the initial LI and LI rise by catheter contact were also affected by the BP-LI (Figure S1). The correlation coefficients were comparable between the two adjustment methods (Figures 7 and 8 vs. Figures S2 and S3). On closer examination, the LI drop adjusted by the BP-LI showed a wider range than those by the initial LI. In other words, the regression slope (or regression coefficient) was smaller in adjusted LI by BP-LI than by initial LI. Using the BP-LI for adjustment results in a smaller change in the estimated lesion size relative to the variation in LI drop, suggesting that this method may allow for more precise lesion size estimation. For instance, when the distribution of LI drop is shallow and lesion size distribution is also shallow, the R-squared values could be high. However, estimating lesion size would be challenging based solely on the LI drop, as small changes in the LI drop could correspond to a wide range of estimated lesion size. Conversely, when the LI drop values and lesion size data are more widely distributed with high R-squared value, lesion size estimation could be more facilitated, potentially enabling more detailed and precise lesion prediction, even with subtle LI changes. In either case, adjusted LI drop using BP-LI or Initial LI could correct deviations in lesion estimation caused by differences in baseline LI.
5 STUDY LIMITATIONS
Our investigation had several limitations. First, the RF applications were performed on the epicardium, not the endocardium, because we focused on precise lesion measurements. Further, the LI data would change with different catheter contact angles4; therefore, caution should be taken when comprehending that data in clinical settings. Since this study was conducted solely in vitro, the results might not align with those of the in vivo study. Furthermore, the experiments were performed in a saline water bath. They may not fully replicate human blood, even if the BP-Lis were consistent. In this study, we evaluated the lesion formation under a single CF value of (10 g) to specifically assess the impact of BP-LI on lesion formation. As a result, the potential effects of CF at varying BP-LI levels remain unknown. Finally, there were small number of steam-pops in this study, probably because of the lower RF power and shorter ablation time; therefore, the safety aspect could not be speculated.
6 CONCLUSION
The lesion size was significantly smaller with a lower BP-LI. The association between the value of the LI drop and lesion formation varied across the different BP-LIs. Adjusted %LI drops may serve as a more reliable parameter for predicting the lesion formation.
ACKNOWLEDGMENTS
We would like to thank Mr. Yoshiki Tasaki for his technical support for this experiment and also appreciate Mr. John Martin for helping with the English editing as a native speaker.
FUNDING INFORMATION
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
HF and HM received lecture fees from Boston Scientific Japan. The other authors have no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data are available upon the request from the corresponding author.




