A significant outbreak of respiratory human adenovirus infections among children aged 3−6 years in Hokkaido, Japan, in 2023
Abstract
Human adenovirus (HAdV) infections present diverse clinical manifestations upon infecting individuals, with respiratory infections predominating in children. We surveyed pediatric hospitalizations due to respiratory HAdV infections across 18 hospitals in Hokkaido Prefecture, Japan, from July 2019 to March 2024, recording 473 admissions. While hospitalizations remained below five cases per week from July 2019 to September 2023, a notable surge occurred in late October 2023, with weekly admissions peaking at 15−20 cases from November to December. There were dramatic shifts in the age distribution of hospitalized patients: during 2019−2021, 1-year-old infants and children aged 3−6 years represented 51.4%−54.8% and 4.1%−13.3%, respectively; however, in 2023−2024, while 1-year-old infants represented 19.0%−20.1%, the proportion of children aged 3−6 years increased to 46.2%−50.0%. Understanding the emergence of significant outbreaks of respiratory HAdV infections and the substantial changes in the age distribution of hospitalized cases necessitates further investigation into the circulating types of HAdV in Hokkaido Prefecture and changes in children's neutralizing antibody titers against HAdV.
1 INTRODUCTION
Human adenovirus (HAdV) infections present with various clinical manifestations, including pharyngoconjunctival fever (PCF), epidemic keratoconjunctivitis, pneumonia, gastroenteritis, myocarditis, and acute hepatitis, and affect individuals across all age groups.1, 2 Among these, the incidence of HAdV infections peaks in children aged 6 months to 5 years. Respiratory infections represent the most common manifestation of HAdV in children, accounting for at least 5%−10% of pediatric respiratory tract infections.3 Outbreaks of respiratory HAdV infections tend to occur in closed environments such as daycare centers for children and military facilities or universities for adults.4 HAdV is classified into numerous types, with specific types often associated with distinct clinical presentations.5 For instance, types 2, 3, 4, 7, and 11 HAdV are commonly implicated in cases of PCF, while types 40 and 41 are commonly associated with gastroenteritis.
Over 4 years have passed since the first confirmed case of COVID-19 in Wuhan, China, in December 2019. The year 2020 witnessed a substantial decline in various infectious diseases other than COVID-19 worldwide, attributed to stringent measures implemented to combat COVID-19.6, 7 In Hokkaido Prefecture, Japan, the first COVID-19 patient was identified on January 28, 2020,8 and the importance of non-pharmaceutical interventions, such as wearing masks, washing hands, disinfecting hands with alcohol, and maintaining a physical distance from others, was emphasized.9 Due to the increasing number of COVID-19 patients, both the national and Hokkaido governments repeatedly issued “State of Emergency” or “Semi-state of Emergency” requests. These requests urged people to refrain from unnecessary outings and gatherings and required businesses to shorten their operating hours.10 Additionally, to prevent the spread of COVID-19 among children, all primary, junior high, and high schools, as well as special support schools, in Hokkaido Prefecture were closed from February 28 to May 31, 2020.11 According to our surveillance data spanning July 2019 to February 2021, hospitalizations due to respiratory infections such as respiratory syncytial virus (RSV), human metapneumovirus (hMPV), and influenza decreased by over 99% following the emergence of COVID-19.12 Additionally, albeit to a lesser extent, hospitalizations associated with respiratory HAdV infections also decreased by approximately 40% after the COVID-19 pandemic compared with pre-pandemic levels.12
Subsequently, with the relaxation of infectious control measures against COVID-19, such as the easing of mask-wearing guidelines, the reopening of schools, and the increase in population movement, various infectious diseases have resurged.13, 14 In Japan, gradual steps were taken from 2022 onwards to ease mask-wearing guidelines and resume acceptance of individual overseas travelers. Furthermore, as of May 8, 2023, COVID-19 was reclassified as a Class 5 infectious disease, equivalent to seasonal influenza. In Hokkaido Prefecture, hMPV infections and influenza, which had been scarcely observed since March 2020, experienced resurgences around October 2022 and March 2023, respectively.15
At the end of 2023, Hokkaido Prefecture faced a significant resurgence of respiratory HAdV infections, unlike anything observed in recent years. Since July 2019, we have been conducting surveillance of pediatric hospitalizations due to infectious diseases across multiple facilities in Hokkaido Prefecture. In this study, we sought to elucidate the characteristics of the notable outbreak of respiratory HAdV infections in 2023 using surveillance data.
2 MATERIALS AND METHODS
2.1 Study period and institutions
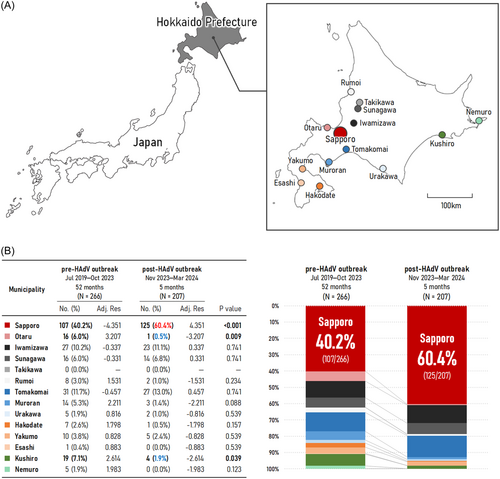
We collected data from patients aged 0−15 years who were diagnosed with respiratory HAdV infection and admitted to 18 hospitals in Hokkaido Prefecture, Japan, between July 1, 2019, and March 17, 2024 (Figure 1A). The inclusion criterion was a positive result on either a rapid antigen detection test or multiplex nested-polymerase chain reaction (PCR) test (BioFire FilmArray Respiratory Panel 2.1; bioMérieux Japan) for HAdV using throat swab or nasopharyngeal swab.16 In hospitals equipped with both rapid antigen detection test kits and the FilmArray Respiratory Panel 2.1, the attending physician predominantly conducted the rapid antigen detection test. When a comprehensive examination of respiratory viruses was deemed necessary, the FilmArray Respiratory Panel was chosen for testing. WHO surveillance case definitions for Severe Acute Respiratory Infection (an acute respiratory illness with a measured temperature of ≥38°C and cough, with onset within the past 10 days that requires hospitalization) were not required as part of the inclusion criteria. Patients were categorized into six age groups: <1, 1, 2, 3−6, 7−12, and 13−15 years. Hokkaido Prefecture, situated in the northernmost region of Japan, has a population of approximately 5.2 million, constituting 4.1% of Japan's total population (Figure 1A).17 It is estimated that 10.8% of the population in Hokkaido Prefecture is under the age of 15 years.18
2.2 Data analysis
The hospitalization rates per 100 000 person-years were calculated using Poisson regression, with exact 95% confidence intervals based on the number of hospitalizations and the size of the target population in the hospitals' catchment areas.18 We compared the number of hospitalized patients per municipality during two periods: the 52 months before the HAdV outbreak (July 2019 to October 2023) and the 5 months after the outbreak (November 2023 to March 2024). We employed the chi-squared test and conducted a residual analysis to compare the two groups. Adjusted standardized residuals were calculated to identify significant values after obtaining statistically significant differences in the chi-squared test. p-Values less than 0.05 were considered significant. The statistical analyses were performed using R Statistical Software (version 4.0.2; R Foundation for Statistical Computing).
2.3 Ethical approval
This study was approved by the Ethics Committee of Sapporo Medical University (Institutional ethical clearance number: 312-3349). Opt-out disclosures were made regarding the study design. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and the principles set out in the Helsinki Declaration, as revised in 2013.
3 RESULTS
Between July 1, 2019, and March 17, 2024, there were a total of 473 admissions due to respiratory HAdV infections. From July 2019 to September 2023, the number of hospitalizations remained consistently below five cases per week. However, a notable surge in patient numbers commenced in late October 2023, with weekly admissions reaching 15−20 cases per week from November to December (Figure 2A). The peak of this surge occurred during the 50th week of 2023 (December 11−17), with 20 cases per week. Subsequently, the number of cases rapidly decreased through January 2024, with 6−8 hospitalizations per week continuing until March 2024.
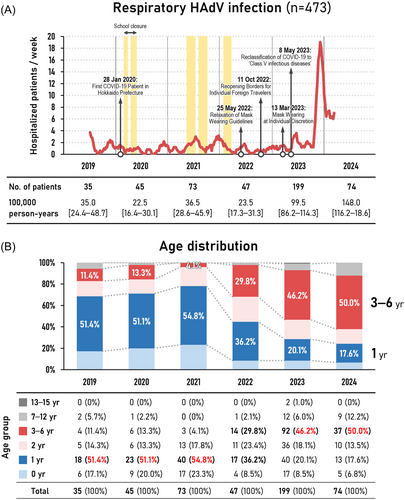
We compared the age distribution of hospitalized patients annually (Figure 2B). In 2019, 2020, and 2021, infants aged 1 year accounted for over 50% of admissions (2019: 51.4% [18/35], 2020: 51.1% [23/45], 2021: 54.8% [40/73]), while admissions for children aged 3−6 years hovered around 10% (2019: 11.4% [4/35], 2020: 13.3% [6/45], 2021: 4.1% [3/73]). However, from 2022 onwards, there was a noticeable decrease in the proportion of 1-year-old infants and a corresponding increase in the proportion of children aged 3−6 years. In 2023, 1-year-old infants accounted for 20.1% (40/199) of admissions, while children aged 3−6 years constituted 46.2% (92/199). From January to March 2024, 1-year-old infants represented only 17.6% (13/74) of admissions, with children aged 3−6 years making up the majority at 50.0% (37/74).
The number of hospitalized patients per municipality significantly changed before (July 2019 to October 2023) and after (November 2023 to March 2024) the respiratory HAdV outbreak (χ2 (12) = 42.62, p < 0.01, V = 0.300). Compared to the pre-outbreak period, the post-outbreak period saw a significant increase in hospitalizations in Sapporo (107/266 [40.2%] to 125/207 [60.4%], p < 0.001) (Figure 1B). In contrast, Otaru and Kushiro experienced a significant decrease in hospitalizations (Otaru: 6.0% [16/266] to 0.5% [1/207], p = 0.009; Kushiro: 7.1% [19/266] to 1.9% [4/207], p = 0.039).
During the study period, there were no reports of acute hepatitis cases in which HAdV was detected.
4 DISCUSSION
We have documented the most extensive outbreak of respiratory HAdV infections in Hokkaido Prefecture over the past 5 years, with the peak occurring in November and December 2023, particularly in Sapporo (Figure 1B). Sapporo is the largest city in Hokkaido Prefecture, with a population of 1.97 million, accounting for 37.7% of the entire population of Hokkaido Prefecture.18 Respiratory HAdV infections typically spread regionally or locally and can rapidly proliferate in closed environments such as daycare centers, where children spend most of their day.19 The respiratory HAdV outbreak in November to December 2023 may have spread across multiple daycare centers in Sapporo. Interestingly, in Otaru, a neighboring city approximately 40 km from Sapporo, there were no significant hospitalizations after November 2023. This observation indicates that even if respiratory HAdV outbreaks occur in nearby municipalities, a clear outbreak may not develop unless the infection is introduced into the community.
It is noteworthy that our surveillance commenced in July 2019, providing approximately 7 months of data before the onset of the COVID-19 pandemic. To compensate for this limitation, we referred to the sentinel surveillance data for PCF in children, published by the Hokkaido Infectious Disease Surveillance Center spanning from 2014 to 2024.20 Although the sentinel surveillance data and the hospitalization numbers in our study cannot be compared due to different methodologies, the trend in PCF reporting from 2019 to 2024 closely paralleled the fluctuation in hospital admissions for respiratory HAdV infections observed in our study. Notably, during the COVID-19 control measures enforced in Hokkaido Prefecture from 2020 to 2022, the number of reported PCF cases was slightly lower compared with the pre-COVID-19 years 2014 to 2019.
Comparing the age distribution of hospitalized patients annually revealed intriguing findings (Figure 2B). While infants aged 1 year represented most of the hospitalized patients from 2019 to 2021, there was a significant shift to children aged 3−6 years in 2023 and 2024. This shift echoes a similar trend observed during the resurgence of RSV and hMPV infections in our previous study in 2021 and 2022, where the predominant age group requiring hospitalization became older compared with the pre-COVID-19 era.15, 21 This pattern aligns with similar trends reported globally.13, 22, 23
In Japan, public health institutes and public health centers nationwide detect HAdV based on the manuals provided by the National Institute of Infectious Diseases (NIID), Japan, with their data integrated by the NIID.24, 25 According to this data, from 2014 to 2019, type 3 HAdV was the most frequently detected among patients with PCF, accounting for approximately 40% of cases. However, following the COVID-19 pandemic, type 3 HAdV was rarely detected in 2021 and 2022. The absence of exposure to type 3 HAdV during this period may have resulted in the accumulation of older children who lacked sufficient neutralizing antibody titers. Remarkably, type 3 HAdV was detected in approximately 70% of cases in 2023. It is well-established that neutralizing antibodies offer protection specific to the virus type and do not confer broad immunity against different types of HAdV.26 The exposure of numerous older children lacking sufficient neutralizing antibody titers to type 3 HAdV may have resulted in severe symptoms requiring hospitalization. However, it should be noted that the circulating types of HAdV can vary by region, and it is uncertain whether the trends observed nationally in Japan are reflective of those in Hokkaido Prefecture.3 Furthermore, HAdV comprises more than 100 serologically distinct types, many of which are recombinants with three major capsid genes—penton base, hexon, and fiber genes.27 Therefore, accurately distinguishing and detecting all types can be challenging, and it is important to recognize that HAdV types that have not been identified may be included in the NIID's data.
Studies conducted in the United States have indicated an increase in HAdV circulation from January to June 2023.28 Similarly to Japan, type 3 HAdV remained undetected there in 2021 and 2022, but emerged as the predominant type (66.3%) in 2023. Notably, type 3 HAdV detections in the United States in 2023 were primarily among children aged 3−5 years, while non-HAdV-3 detections were more prevalent in children under 3 years old. Additionally, studies from China also mentioned a significant decrease in type B HAdV, including type 3, following the implementation of COVID-19 non-pharmaceutical interventions in January 2020.29, 30 The resurgence of HAdV-B3 circulation after its initial decline due to COVID-19 control measures highlights the potential for substantial outbreaks of respiratory HAdV infections worldwide, emphasizing the need for continued vigilance.
Since 2022, there has been a sharp increase in reports of unexplained acute hepatitis in children worldwide, some of which have had fatal outcomes.31 Notably, many of these cases have detected HAdV, especially in Europe and the United States. However, according to a nationwide survey in Japan from January 2017 to June 2022, reports of acute hepatitis in children were fewer after the onset of the COVID-19 pandemic than before, with only 1.7% (12/707) of cases detecting HAdV.32 In this study, we captured a significant outbreak of respiratory HAdV infections. However, during the study period, there were no reports of acute hepatitis in children in which HAdV was detected. Nevertheless, as the number of HAdV infections increases, there may be a potential for patients to develop acute hepatitis, necessitating careful monitoring in the future.
This study had several limitations. First, the results of this study are based on weekly surveillance data of patients who were admitted to 18 hospitals with which we regularly collaborate. As such, we only have information on age and gender, and do not have detailed data on the clinical course of the patients during hospitalization. Therefore, it was not possible to conduct an in-depth analysis of their clinical progression. Second, there were no predefined criteria for conducting rapid antigen detection tests and multiplex PCR tests, which could have introduced selection bias. Third, the 18 hospitals in our study did not uniformly utilize the same rapid antigen detection kits. For example, some hospitals used QuickNaviTM-Adeno2 (Denka Co., Ltd.), while other hospitals used ImunoAce Adeno (TAUNS Laboratories). It is noteworthy that the sensitivity and specificity of rapid antigen detection tests vary considerably depending on the product.33 Additionally, some facilities had introduced the BioFire FilmArray Respiratory Panel 2.1, while others had not. These variabilities in testing methods could potentially introduce detection bias. Fourth, multiplex PCR systems occasionally identify mixed viral infections, leading to an overcounting of cases.34, 35
5 CONCLUSIONS
A notable surge in respiratory HAdV infections occurred in Hokkaido Prefecture during November and December 2023, marking an event that was unprecedented in recent years. Notably, the majority of hospitalized children belonged to the older age group of 3−6 years. This surge may be attributed to the resurgence of type 3 HAdV infections in 2023, which were rarely detected in 2021 and 2022. Continuous epidemiological surveillance remains indispensable for accurately assessing the impact of HAdV infections on children in the post-COVID-19 era.
AUTHOR CONTRIBUTIONS
Yuya Fukuda was involved in study conceptualization, methodology, formal analysis, investigation, and writing the original draft. Atsuo Togashi, Satoshi Hirakawa, Masaki Yamamoto, Shinobu Fukumura, Tomohiro Nawa, Nana Kushima, Jun Kunizaki, Kouhei Nishino, Ryoma Kimura, Toshitaka Kizawa, Dai Yamamoto, Ryoh Takeuchi, Yuta Sasaoka, Masayoshi Kikuchi, Takuro Ito, Kazushige Nagai, Hirofumi Asakura, Sayaka Nishimura, Masaki Yoshida, and Kosuke Tsuchida were involved in the study investigation. Takeshi Tsugawa was involved in critically revising the article for important intellectual content. All authors revised the manuscript, approved the manuscript to be published, and agreed to be accountable for all aspects of the work in ensuring that issues related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. All authors meet the ICMJE authorship criteria.
ACKNOWLEDGMENTS
We would like to thank all the pediatricians who participated in this survey. We thank Lorraine Law, BSc, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, Yuya Fukuda, upon reasonable request.