New-onset neurodegenerative diseases following SARS-CoV-2 infection: An analysis of prediction interval
We read with interest the article by Rahmati et al. titled “New-onset neurodegenerative diseases as long-term sequelae of SARS-CoV-2 infection: A systematic review and meta-analysis” published in the Journal of Medical Virology.1 The authors performed an expansive systematic review and meta-analysis including over 33 million individuals to determine whether COVID-19 survivors are at an increased risk of developing Alzheimer's disease (AD), dementia, and Parkinson's disease (PD).1 They found a significant association between SARS-CoV-2 infection and a 50% increased risk of AD, 66% increased risk of dementia, and 44% increased risk of PD.1 These findings imply that a considerable number of people are potentially susceptible to neurodegenerative complications following the COVID-19 pandemic. There is a need to reevaluate strategies related to neurocognitive screening, preventative actions, and health care resource allocation. If confirmed, these findings1 could substantially impact clinical practice and health policies related to the long-term care of COVID-19 survivors.
However, substantial heterogeneity was observed among the included studies for all outcomes, with I2 values ranging from 86% to 97%.1 As the authors discussed,1 differences in patient populations, follow-up times, diagnostic criteria, and control groups likely contributed to the high heterogeneity. Additionally, most studies in the original meta-analysis1 were conducted in the United States, which may limit the generalizability of the findings to other populations. Before applying these findings clinically or developing policies based on these findings, the heterogeneity and generalizability issues must be addressed. To address these critical issues, we chose to calculate the prediction intervals for the meta-analysis outcomes. Prediction intervals account for between-study variance and provide estimates of the range of effect sizes expected in similar but new settings and populations.2-4 In contrast, confidence intervals only describe the precision of the pooled effect size. Other common methods for examining heterogeneity, such as subgroup analysis or meta-regression, may identify explanatory factors, but do not directly quantify overall variability. We believe that prediction intervals complement these other techniques and are particularly suitable for assessing generalizability issues stemming from the high observed heterogeneity. By directly estimating effect size variability across populations, prediction intervals can indicate whether meta-analytic conclusions are likely to be robust and applicable when implemented in real-world clinical scenarios and in future studies.2-4
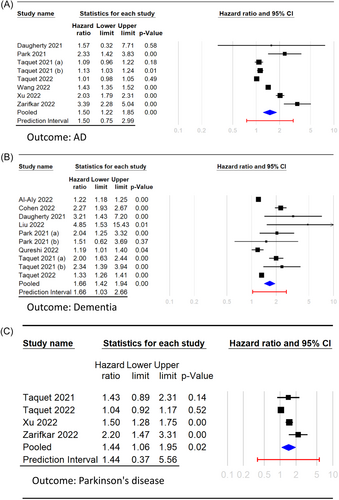
As the original meta-analysis1 did not include prediction interval calculations, we revisited the original article and collected raw data. Comprehensive Meta-Analysis (Version 4, Biostat) was used for this analysis. As depicted in Figure 1, the prediction interval for AD ranged from 0.75 to 2.99 (Figure 1A). For dementia, the interval was between 1.03 and 2.66 (Figure 1B); for PD, it was 0.37−5.56 (Figure 1C). The broad prediction intervals for AD and PD, which overlap with the null value of 1, suggest that any potential increased risk might not be consistently applicable to new populations. More studies are required before drawing conclusions about whether SARS-CoV-2 infection increases the risk of AD and PD. However, there appears to be a more definitive association between SARS-CoV-2 infection and increased risk of dementia.
In conclusion, we congratulate the authors of this impressive systematic review and meta-analysis to synthesize current literature on the potential neurodegenerative complications of COVID-19. Their research underscores a significant area that requires further exploration. Future studies should investigate the causes of heterogeneity and evaluate the generalizability of these findings across diverse global populations. It is only after addressing the issues of unexplained heterogeneity and ensuring widespread applicability that definitive conclusions can be drawn regarding the risks of neurodegenerative diseases post-COVID-19 as well as the subsequent implications for clinical practices and health policy formulation.
AUTHOR CONTRIBUTIONS
I-Wen Chen and Kuo-Chuan Hung wrote the main manuscript text. Hsiu-Jung Lin prepared Figure 1. All authors read and approved the final version of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




