Prevalence of orthostatic intolerance in long covid clinic patients and healthy volunteers: A multicenter study
Trial registration numbers NCT05057260, ISRCTN15022307.
Abstract
Orthostatic intolerance (OI), including postural orthostatic tachycardia syndrome (PoTS) and orthostatic hypotension (OH), are often reported in long covid, but published studies are small with inconsistent results. We sought to estimate the prevalence of objective OI in patients attending long covid clinics and healthy volunteers and associations with OI symptoms and comorbidities. Participants with a diagnosis of long covid were recruited from eight UK long covid clinics, and healthy volunteers from general population. All undertook standardized National Aeronautics and Space Administration Lean Test (NLT). Participants' history of typical OI symptoms (e.g., dizziness, palpitations) before and during the NLT were recorded. Two hundred seventy-seven long covid patients and 50 frequency-matched healthy volunteers were tested. Healthy volunteers had no history of OI symptoms or symptoms during NLT or PoTS, 10% had asymptomatic OH. One hundred thirty (47%) long covid patients had previous history of OI symptoms and 144 (52%) developed symptoms during the NLT. Forty-one (15%) had an abnormal NLT, 20 (7%) met criteria for PoTS, and 21 (8%) had OH. Of patients with an abnormal NLT, 45% had no prior symptoms of OI. Relaxing the diagnostic thresholds for PoTS from two consecutive abnormal readings to one abnormal reading during the NLT, resulted in 11% of long covid participants (an additional 4%) meeting criteria for PoTS, but not in healthy volunteers. More than half of long covid patients experienced OI symptoms during NLT and more than one in 10 patients met the criteria for either PoTS or OH, half of whom did not report previous typical OI symptoms. We therefore recommend all patients attending long covid clinics are offered an NLT and appropriate management commenced.
1 INTRODUCTION
The protracted form of COVID-19 infection is known as long covid1-3 and is frequently accompanied by orthostatic intolerance (OI)4, 5 (symptoms suggestive of an abnormal haemodynamic response to upright posture), such as dizziness, light-headedness, palpitations, or tremulousness.6 During objective testing, the blood pressure may fall significantly on standing (orthostatic hypotension, OH)7, 8 or there may be a significant rise in heart rate on standing without a drop in blood pressure—a condition known as orthostatic tachycardia (OT), or (if accompanied by symptoms during postural testing) postural orthostatic tachycardia syndrome (PoTS).6, 9 The diagnosis of PoTS requires OH to be excluded, hence a patient may have either OH or PoTS but not both. Both OH and PoTS occur in several different conditions and are thought to be due to abnormal function of the autonomic nervous system.6, 10, 11 OH is typically found in older people, people with diabetes, and people on diuretics.7, 8 PoTS tends to occur more in younger people, and can incur diagnostic delays, with often-marked functional impairment and psychological impact.12, 13 Some studies have suggested a link between PoTS and myalgic encephalomyelitis/chronic fatigue syndrome.14-17 Orthostatic abnormalities including OH, OT, and PoTS have also been identified as a sequel of long covid5, 18-23 which can have a significant impact on day-to-day functioning.24
Long covid is associated with many diverse abnormalities in the neurological and cardiovascular systems, including abnormal autonomic response (“dysautonomia”)10, 23, 25-28 which has been observed in other post-viral conditions.29 Symptoms of long covid can be complex and prolonged,30 many of which overlap with those of OI, and include dizziness, palpitations, tightness or pain in the chest, and tingling in the extremities on standing.4, 20 The presentation of nonspecific OI symptoms, such as generalized tiredness and cognitive impairment, can render a diagnosis of OH or PoTS difficult to detect.29, 30 This is further compounded given the lack of association in long covid with specific symptoms and those associated with typical OI.23, 31 There have been several previous studies on the prevalence of OH and PoTS in long covid patients,23 but they are small or single-clinic studies,5, 31 and samples were sometimes skewed. Prevalence of OI is varied and ranges from 2% to 33% 19, 23 with a reported incidence of 71% obtained from a sample of 29 patients with OI referred for tilt table testing (a specialist test not available in standard clinics).24
This study was designed to answer three important questions about OI in long covid using a large sample drawn from multiple clinics. First, what is the overall prevalence of OH and PoTS in an unselected clinic population using a standard objective test, the 10 min National Aeronautics and Space Administration Lean Test (NLT) and how does it differ from healthy volunteers with no long covid? Second, can people with OH and PoTS be identified purely by testing those who reported typical OI symptoms such as palpitations or dizziness on standing, or is formal NLT testing of everyone necessary? And third, what associations are there between long covid's features, comorbidities, and either OH or PoTS?
2 METHODS
2.1 The LOCOMOTION study
The work reported here was part of LOCOMOTION (LOng COvid Multidisciplinary consortium Optimizing Treatments and services across the NHS), a 36-month multisite case study of 10 long covid clinics (of which eight participated in this substudy), beginning in 2021, which seeks to optimize long covid care across the clinics. Each clinic offers multidisciplinary care to patients referred from primary care (and, in some cases, self-referred). A study protocol for LOCOMOTION, with details of management, governance, and patient involvement has been published.32 Ethics approval was granted by Yorkshire & The Humber—Bradford Leeds Research Ethics Committee (REC; ref: 21/YH/0276) and subsequent amendments.
2.2 Patient involvement
One of the work packages in LOCOMOTION involves a quality improvement collaborative, in which front-line clinicians from all 10 clinics and patient advisors identify priority areas for improvement and follow a cycle of measuring current practice, implementing change, and remeasuring practice [paper submitted]. The study concept and question of whether PoTS was being diagnosed and adequately managed in these clinics was the leading priority for our patient advisers and among the top questions raised by clinicians.
2.3 Sampling and data sources
Based on previous literature,17, 33 we estimated that 250 long covid patients would provide sufficient precision to estimate 30% positive NLT to within ±6%. With 50 healthy volunteers, this would also provide 90% power to detect a 20% difference between groups in positive NLTs (30% vs. 10%) at p < 0.05.
Data collection occurred from May to October 2023 in eight clinics across the UK. Consecutive patients attending participating clinics with a confirmed clinical diagnosis of long covid (as per NICE guidelines criteria)34 were invited to join the study. Inclusion criteria were age over 18, able and willing to consent, either a long covid clinic patient or a healthy volunteer, and (if self-testing at home) in possession of a blood pressure machine. The healthy volunteers were age-sex frequency-matched to the long covid group using 10-year age-bands.
Exclusion criteria were inability to give informed consent or comply with test instructions, if the clinical team considered the test unsuitable or unsafe (e.g., if the patient could not stand unaided), and any coexisting condition that could interfere with autonomic or haemodynamic function (e.g., pregnancy). Verbal informed consent to perform the NLT were obtained from all participants. Written consent were obtained by the healthy volunteers, this was considered unnecessary for the long covid patient since this intervention was already part of standard clinical assessment in many clinics and its introduction had been justified as a quality improvement measure.
2.4 OI symptoms
Before having the test, participants were asked about their long covid symptoms specifically to detail typical symptoms suggestive of OI6: dizziness, palpitations, chest pain or discomfort, tremulousness.
2.5 The NASA lean test
The NLT was used as per published instructions.35 The NLT has been validated for detecting OI in long covid and other conditions such as chronic fatigue syndrome, fibromyalgia, and PoTS.17, 23, 36 Participants were offered the test as part of a clinic assessment or given the option of self-administering at home for the few sites that offered this.
In the NLT, the participant first lies quietly for 2−5 min, then two supine readings (pulse and blood pressure) were taken 1 min apart. The participant then stands up slowly with the shoulders leaning against a wall (for support), with feet about 15 cm from the wall. Six further readings were taken at 1−2 min intervals.
The NLT was terminated prematurely if participants' symptoms were such that they were unable to complete the full 10 min or if the clinician was concerned. If the NLT was stopped early, available data were analyzed.31 Regular meetings were held to ensure consistency in practice across participating sites.
Table 1 shows the criteria we used for diagnosing OH, PoTS, OI, symptomatic NLT, and a positive NLT.
| Orthostatic intolerance (OI) | Dizziness/light-headedness, palpitations, chest pain, or tremulousness which get worse when sitting or standing and improves or resolves when lying down |
| Orthostatic hypotension (OH) | Fall in systolic blood pressure within the first three readings of at least 20 mmHg, or fall in diastolic blood pressure of at least 10 mmHg with or without acute symptoms during test |
| Orthostatic tachycardia (OT) | Increase in HR above baseline of at least 30 bpm, sustained for two consecutive readings, after excluding OH |
| Postural orthostatic tachycardia syndrome (PoTS) | OT plus symptoms of OI during the NLT |
| Symptomatic NLT | Any symptoms reported during the NLT, including baseline symptoms that were exacerbated by standing |
| Positive NLT | Patients meeting the criteria for PoTS or OH |
| Narrow pulse pressure (PP)a | Difference between systolic and diastolic blood pressure which is less than 25% of the systolic blood pressure |
- a 33.
2.6 Objectives
We aimed to estimate (1) the prevalence of subjective OI (symptoms of OT) and objective OI (OH and PoTS) in healthy people and in long covid patients; (2) the association between patient characteristics and prevalence of objective OI, OH, and PoTS; (3) the prevalence of OH and PoTS in people with a history of OI symptoms compared to those without a history; (4) the impact of relaxing the standard thresholds from two abnormal readings to one abnormal reading during the NLT for the diagnosis of PoTS.
2.7 Data management
Anonymized data were shared with the host site, University of Leeds, for data analysis, adhering with sites' local governance procedures and in compliance with the ethics approvals.
2.8 Statistical analysis
All statistical analyses were conducted in Stata version 18 [StataCorp. 2023; Stata: Release 18; Statistical Software: StataCorp LLC]. 95% confidence intervals (CI) were calculated for proportions of participants with sustained increased in HR, OI, OH, narrow PP, and PoTS during their NLT. Where there were no participants in a category, one-sided exact 97.5% CIs were calculated. Comparisons between two proportions used Fisher's exact test, with exact 95% CIs.
To identify predictors of PoTS or OH in long covid patients, logistic regression was used to quantify associations between patient characteristics (age, sex, body mass index [BMI], ethnicity), preexisting comorbidities, and prior symptoms (see list above) and confirmation of PoTS following an NLT. Models were calculated both unadjusted and adjusted for age and sex. Categories with fewer than 10 participants were merged or excluded. Where an NLT was terminated early, the last measurements were carried forward.
2.9 Sensitivity analyses
To understand whether long covid patients were experiencing symptoms at lower thresholds than the formal definition of PoTS, we explored the robustness of our results when applying different definitions. We evaluated sensitivity to how long an increased heart rate needed to be sustained for (over 2 min, any two consecutive time points, any two time points, or any one time point).
3 RESULTS
3.1 Participants
Across eight clinics, 277 patients and 50 healthy volunteers frequency-matched on age and sex were recruited. Participant characteristics are shown in Table 2. The demographic characteristics of long covid patients recruited to this study broadly reflected those of long covid clinic populations in the country.37 Healthy volunteers were matched on age and sex but had lower mean BMI and fewer comorbidities than long covid patients (Table 2).
| Long covid patients | Healthy volunteers | |
|---|---|---|
| (n = 277) | (n = 50) | |
| Mean age (years) (SD) | 48 (13) | 48 (16) |
| Sex | ||
| Female (%) | 173 (62%) | 32 (64%) |
| Male (%) | 104 (38%) | 18 (36%) |
| Mean body mass index (kg/m2) (SD) | 29 (7) | 25 (5) |
| Ethnicity | ||
| White (%) | 219 (79%) | 31 (62%) |
| Black, Black British, Caribbean, or African (%) | 7 (3%) | 0 (0%) |
| Asian/Asian British (%) | 23 (8%) | 3 (6%) |
| Mixed, multiple, or other ethnic groups (%) | 16 (6%) | 14 (28%) |
| Not recorded (%) | 12 (4%) | 2 (4%) |
| Known medical conditions | ||
| Long covid | 277 (100%) | 0 (0%) |
| Allergies or autoimmune conditions (%) | 44 (16%) | 6 (12%) |
| Other respiratory conditions (%) | 1 (<1%) | 0 (0%) |
| Other inflammatory conditions (%) | 12 (4%) | 2 (3%) |
| Hypertension (%) | 28 (10%) | 4 (6%) |
| Hypotension (%) | 0 (0%) | 0 (0%) |
| Other heart conditions (%) | 22 (8%) | 2 (4%) |
| Type 2 diabetes mellitus (%) | 16 (6%) | 1 (2%) |
| Mental health condition (%) | 43 (16%) | 0 (0%) |
| Median duration of long Covid (IQR) (months) | 18 (14−28) | - |
| Admitted to hospital with initial SARS-CoV-2 infection (%)a | 16 (9%) | - |
| Admitted to intensive care with initial SARS-CoV-2 infection (%)a | 4 (2%) | - |
- a Where numbers do not sum to totals, this is because of incomplete data.
3.2 Prevalence of OI, OH, and PoTS in healthy volunteers
None of the healthy volunteers had symptoms of OI before testing or had to terminate the NLT early because of symptoms. None of these participants had orthostatic tachycardia 0/50 (0%) (95% CI: 0%−7%) or met the criteria for PoTS (Table 3). Five (10%, 95% CI: 3%−22%) met the haemodynamic criteria for OH (Table 3), four were identified within 2 min of standing and one at minute four. All healthy volunteers had no previous history suggestive of OI and were asymptomatic during the test.
| Long covid patients (n = 277) | ||||
|---|---|---|---|---|
| With previous history of OI (n = 130) | No previous history of OI (n = 147) | All long covid patients (n = 277) | Healthy voluntees (n = 50) | |
| Met criteria for PoTS (%) | 14 (11%) | 6 (4%) | 20 (7%) | 0 (0%) |
| (95% CI) | (6%−17%) | (2%−9%) | (4%−11%) | (0%−7%) |
| Met criteria for OH with or without symptoms during NLT (%) | 7 (5%) | 14 (10%) | 21 (8%) | 5 (10%) |
| (95% CI) | (2%−11%) | (5%−15%) | (5%−11%) | (3%−22%) |
- Abbreviations: OH, orthostatic hypotension; OI, orthostatic intolerance; PoTS, postural orthostatic tachycardia syndrome.
3.3 Prevalence of OI, OH, and PoTS in long covid clinic patients
3.3.1 OI
Of the 277 patients recruited from long covid clinics, 130 (47%) had a previous history of symptoms suggestive of OI (dizziness, palpitations, chest pain, or tremors) before their NLT. A total of 144 (52%) were symptomatic during the NLT, with a range of acute symptoms reported (most commonly dizziness but also palpitations, chest pain or tremors, fatigue, muscle or joint pain, cognitive dysfunction, headache, visual disturbances, breathlessness, tingling or numbness in the skin, sweating, or clamminess) (Table 4). In the NLT, 20 (7%, 95% CI: 4%−11%) long covid patients met the criteria for PoTS and 21 (8%, 5%−11%) met the criteria for OH (Table 3), 18 reached the threshold for OH within the first 2 min of standing and three by minute four. A total of 46 (17%) patients stopped the test early because of excessive symptoms. Of these, just six met the criteria for PoTS and seven met the criteria for OH (see Table 4 for details of tests ended prematurely).
| In long COVID patients who could not complete NLT | |
|---|---|
| Symptom | (n = 46) |
| Symptoms of orthostatic intolerance | |
| Dizziness/light-headedness | 23 (50%, 95% CI: 35%−65%) |
| Palpitations | 5 (11%, 95% CI: 4%−24%) |
| Chest pain/discomfort | 2 (4%, 95% CI: 1%−15%) |
| Tremors | 1 (2%, 95% CI: 0%−12%) |
| Other symptoms of dysautonomia | |
| Tingling/numbness in skin | 11 (24%, 95% CI: 13%−39%) |
| Fatigue | 11 (24%, 95% CI: 13%−39%) |
| Sweating/clammy/hot | 5 (11%, 95% CI: 4%−24%) |
| Breathlessness | 2 (4%, 95% CI: 1%−15%) |
| Headache | 4 (9%, 95% CI: 2%−21%) |
| Muscle/joint pain | 2 (4%, 95% CI: 1%−15%) |
| Cognitive dysfunction | 1 (2%, 95% CI: 0%−12%) |
| Visual disturbances | 1 (2%, 95% CI: 0%−12%) |
3.3.2 Orthostatic hypotension
Twenty-one (8%, 5%−11%) of long covid participants met the criteria for OH, of which 11 (4%) had symptoms during the test and 10 (4%) were asymptomatic.
3.3.3 Orthostatic tachycardia/PoTS
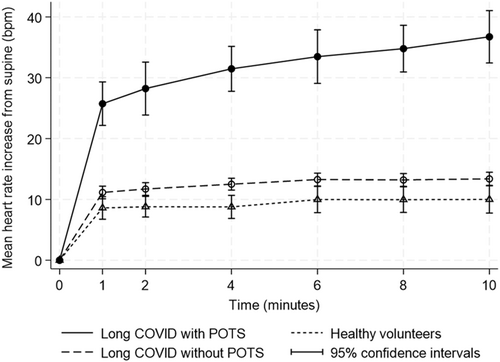
During the NLT, 28 (10%, 7%−14%) participants experienced OT with no drop in blood pressure (data not shown), with 20 (7%, 4%−11%) experiencing acute symptoms (dizziness, palpitations, chest pain, or tremors) during the NLT, meeting the criteria for PoTS (Table 5). As shown in Figure 1, in patients who went on to meet the criteria for PoTS, the marked increase in mean heart rates was apparent shortly after standing, with a more gradual increase thereafter. By contrast, patients with negative test results initially increased by just over 10 bpm on average and remained stable for the remainder of the test. Long covid patients with negative NLT results had mean heart rate increases similar to healthy volunteers with negative NLT.
| In all long covid patients | In those with prior history of OI symptoms | In those meeting criteria for PoTS | In those meeting criteria for OHa | In healthy volunteers | |
|---|---|---|---|---|---|
| Symptom | (n = 277) | (n = 130) | (n = 20) | (n = 21) | (n = 50) |
| All symptoms | |||||
| Any symptoms during NLT | 144 (52%) | 84 (65%) | 20 (100%) | 11 (52%) | 0 (0%) |
| (46%−58%) | (56%−73%) | (83%−100%)b | (30%−74%) | (0%−7%) | |
| Typical symptoms of orthostatic intolerance | |||||
| Dizziness/light-headedness | 92 (33%) | 67 (52%) | 13 (65%) | 5 (24%) | 0 (0%) |
| (28%−39%) | (43%−60%) | (41%−85%) | (8%−47%) | (0%−7%) | |
| Palpitations | 15 (5%) | 13 (10%) | 2 (10%) | 0 (0%) | 0 (0%) |
| (3%−9%) | (5%−16%) | (1%−32%) | (0%−16%) | (0%−7%) | |
| Chest pain/discomfort | 12 (4%) | 10 (8%) | 3 (15%) | 1 (5%) | 0 (0%) |
| (2%−7%) | (4%−14%) | (3%−38%) | (0%−24%) | (0%−7%) | |
| Tremors | 2 (1%) | 2 (2%) | 0 (0%) | 0 (0%) | 0 (0%) |
| (0%−3%) | (0%−5%) | (0%−17%) | (0%−16%) | (0%−7%) | |
| Other symptoms of orthostatic intolerance | |||||
| Tingling/numbness in skin | 34 (12%) | 18 (14%) | 6 (30%) | 2 (10%) | 0 (0%) |
| (9%−17%) | (8%−21%) | (12%−54%) | (1%−30%) | (0%−7%) | |
| Fatigue | 26 (9%) | 6 (5%) | 1 (5%) | 3 (14%) | 0 (0%) |
| (6%−13%) | (2%−10%) | (0%−25%) | (3%−36%) | (0%−7%) | |
| Sweating/clammy/hot | 19 (7%) | 10 (8%) | 2 (10%) | 3 (14%) | 0 (0%) |
| (4%−11%) | (4%−14%) | (1%−32%) | (3%−36%) | (0%−7%) | |
| Breathlessness | 15 (5%) | 7 (5%) | 3 (15%) | 0 (0%) | 0 (0%) |
| (3%−9%) | (2%−11%) | (3%−38%) | (0%−16%) | (0%−7%) | |
| Headache | 11 (4%) | 6 (5%) | 5 (25%) | 1 (5%) | 0 (0%) |
| (2%−7%) | (2%−10%) | (9%−49%) | (0%−24%) | (0%−7%) | |
| Muscle/joint pain | 4 (1%) | 3 (2%) | 0 (0%) | 0 (0%) | 0 (0%) |
| (0%−4%) | (0%−7%) | (0%−17%) | (0%−16%) | (0%−7%) | |
| Cognitive dysfunction | 1 (<1%) | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) |
| (0%−2%) | (0%−4%) | (0%−17%) | (0%−16%) | (0%−7%) | |
| Visual disturbances | 5 (2%) | 3 (2%) | 0 (0%) | 1 (5%) | 0 (0%) |
| (1%−4%) | (0%−7%) | (0%−17%) | (0%−24%) | (0%−7%) |
- Abbreviations: NLT, NASA Lean Test; OH, orthostatic hypotension; OI, orthostatic intolerance; PoTS, postural orthostatic tachycardia syndrome.
- a All patients meeting haemodynamic criteria for OH included including those with and without symptoms during lean test.
- b By definition, all cases of PoTS were symptomatic during the lean test.
3.4 Association between patient characteristics and prevalence of OI, OH, and PoTS
Symptoms experienced during the NLT are shown in Table 4. Associations between long covid patient characteristics, preexisting comorbidities, and prior symptoms with PoTS and with OH are presented in Supporting Information S1: Tables 1 and 2, respectively. Patients meeting the criteria for PoTS tended to be younger and more likely to be female, and report a higher prevalence of mental health conditions such as anxiety or depression, though CIs were wide. Patients with PoTs were also more likely to have reported a history of typical OI symptoms compared to those with OH. Conversely, patients with OH were older with more physical health comorbidities.
3.5 Association between prior history of OI and OH or PoTS
Whilst long covid patients who reported a prior history suggestive of OI, were more likely to meet the criteria for PoTS (RR = 2.6, 1.0−6.7, p = 0.03), 6 of the 20 had no history of OI symptoms (Table 3). By contrast, only a third of those who met the criteria for OH, 7 out of the 21, reported a history suggestive of OI. The occurrence of OH in those who did not report a history suggestive of OI was the same (10%) as that seen in the asymptomatic healthy volunteers (Table 6).
| Long COVID patients (n = 277) | Healthy controls (n = 50) | |||||||
|---|---|---|---|---|---|---|---|---|
| History of long COVID symptoms suggestive of orthostatic intolerancea | History of long COVID symptoms suggestive of orthostatic intolerancea | |||||||
| No (n = 147) | Yes (n = 130) | No (n = 50) | Yes (n = 0) | |||||
| Lean test measures | n (%) | (95% CI) | n (%) | (95% CI) | n (%) | (95% CI) | n (%) | (95% CI) |
| Orthostatic tachycardia (increased heart rateb with no drop in blood pressurec) | ||||||||
| With no acute symptoms during NLT | 5 (3%) | 1 (8%) | 3 (2%) | 0 (7%) | 0 (0%) | 0 (7%) | - | - |
| With acute symptoms during NLT (PoTS)d | 6 (4%) | 2 (9%) | 14 (11%) | 6 (17%) | 0 (0%) | 0 (7%) | - | - |
| Orthostatic hypotension (fall in blood pressureb) | ||||||||
| With no acute symptoms during NLT | 6 (4%) | 2 (9%) | 4 (3%) | 0 (8%) | 5 (10%) | 3 (22%) | - | - |
| With acute symptoms during NLTd | 8 (5%) | 2 (10%) | 3 (2%) | 0 (7%) | 0 (0%) | 0 (7%) | - | - |
| Narrow pulse pressure (pulse pressure <25% of systolic blood pressure) | ||||||||
| With no acute symptoms during NLT | 27 (18%) | 12 (26%) | 24 (18%) | 12 (26%) | 10 (20%) | 10 (34%) | - | - |
| With acute symptoms during NLTd | 31 (21%) | 15 (29%) | 40 (31%) | 23 (39%) | 0 (0%) | 0 (7%) | - | - |
- a History of long COVID symptoms suggestive of orthostatic intolerance before the lean test was taken as dizziness, palpitations, chest pain, or tremors.
- b Heart rate increased by ≥30 bpm (age 18+) or ≥40 bpm (age <18) sustained over two consecutive time points.
- c Fall in systolic blood pressure ≥20 mmHg or diastolic blood pressure ≥10 mmHg within first 4 min.
- d Symptoms of dysautonomia included dizziness, palpitations, chest pain or tremors, fatigue, muscle or joint pain, cognitive dysfunction, headache, visual disturbances, breathlessness, tingling or numbness in the skin, sweating, or clamminess.
3.6 Sensitivity to relaxing thresholds for diagnosing OH and PoTS
When the criterion for the increased heart rate to be sustained was relaxed, from two consecutive to one reading, this resulted in increasing the numbers of patients meeting the criteria for PoTS (from 7% to 11%) with no increase noted in healthy volunteers (Table 7). Increases were similar for those with and without a prior history of OI symptoms. In addition, decreasing the threshold from ≥30 to ≥20 bpm resulted in approximately twice as many long covid patients meeting the criteria for PoTS. However, the increase in numbers that would meet the criteria was similar in patients with and without previous history of OI (Table 7). If the lower threshold was used, three (6%) healthy volunteers would have met the relaxed criteria for OT (data not shown), but still none would have met the criteria for PoTS because all healthy volunteers were asymptomatic during the NLT.
| Long covid patients (n = 277) | ||||
|---|---|---|---|---|
| History of OI symptoms (n = 130) | No history of OI symptoms (n = 147) | All long covid patients (n = 277) | Healthy volunteers (n = 50) | |
| Symptomatic during NLT with two consecutive heart rate readings ≥30 bpm above supine (%) | 14 (11%) | 6 (4%) | 20 (7%) | 0 (0%) |
| (95% CI) | (6%−17%) | (2%−9%) | (4%−11%) | (0%−7%) |
| Symptomatic during NLT with single heart rate reading ≥30 bpm above supine (%) | 20 (15%) | 11 (7%) | 31 (11%) | 0 (0%) |
| (95% CI) | (10%−23%) | (4%−13%) | (8%−16%) | (0%−7%) |
| Symptomatic during NLT with two consecutive heart rate readings ≥20 bpm above supine (%) | 33 (25%) | 17 (12%) | 50 (18%) | 0 (0%) |
| (95% CI) | (18%−34%) | (7%−18%) | (14%−23%) | (0%−7%) |
- Abbreviation: OI, orthostatic intolerance.
3.7 Additional findings
Further analyses, reported in the Table 6, include a difference in pulse pressure (PP) between long covid and healthy volunteers. While PP is not a routine clinical measurement, 122 (44%) of long covid patients were found to have a narrow PP (difference between diastolic and systolic, less than 25% of systolic blood pressure) compared to 10 (20%) of healthy volunteers. A narrow PP was seen more frequently, 71 out of 122 (58%), in long covid patients who reported acute symptoms during the NLT. The occurrence of a narrow PP was not associated with a history of OI, with 48% of long covid patients reporting a history suggestive of OI and 52% did not (data not shown).
4 DISCUSSION
These findings strongly confirm that OI, OH, and PoTS are all associated with a diagnosis of long covid, whilst OI, symptomatic OH, and PoTS are rare in healthy volunteers. Whilst half of long covid clinic patients have symptoms of OI, not all reach the NLT threshold for either OH or PoTS. PoTS was more common in younger female patients, whilst OH was more common in older patients with comorbidities. Relaxing the criteria for sustained increase in heart rate would categorize more long covid patients with PoTS without resulting in healthy asymptomatic people being misclassified.
Previous studies of the prevalence of OI, OH, OT, and PoTS in long covid patients have been on small or unrepresentative samples,23 with elevated rates of PoTS over 70% in a select cohort.5, 20 However, our estimates are consistent with those in comparable populations of 2%−14%.19, 31, 38 Whilst estimates of OH in long covid vary from 4% to 28%, our results are comparable to similarly-aged cohorts.23, 31 Some differences in estimated prevalence can be explained by different lean test protocols, for example, restricted diets,33 which are not practical for routine clinic assessments. We applied commonly used criteria for PoTS, but implementation varies internationally. Others have previously applied a single elevated HR measurement,9, 33, 38 an average of two,39 the last three,17 or two consecutive readings.6, 31 These different thresholds have not previously been explored within the same cohort.
Acute symptoms during the NLT have been reported in 33%−66% of patients with long covid population.31, 38 We saw similarly high prevalence of 53% (114 patients) with acute symptoms during the NLT which were not explained by haemodynamic measurements. This lack of association between symptoms and a positive NLT is consistent with previous findings.19, 31, 38 Whilst most patients were able to complete a full 10 min of standing, 17% (46 patients) terminated the test early because of excessive symptoms, less than our previous report, (30) but higher than others have found.38 Dizziness (65%, n = 13) was the most frequent acute NLT symptom of PoTS, consistent with previous work,5, 38 but also tingling (30%, n = 6), headaches (25%, n = 5), breathlessness (15%, n = 3), and chest discomfort (15%, n = 3), contrasting with symptoms in people with OH of dizziness (25%, n = 5), fatigue (14%, n = 3), clamminess (14%, n = 3), and tingling (10%, n = 2).
Narrow PP has previously been reported as low in long covid patients during an NLT,33 Vernon et al. reported a significantly lower mean PP (20% of systolic BP at 10 min) compared to those with ME/CFS and the control group (29% of SBP at 10 min). There are studies suggesting an association between narrow PP and reduced cerebral blood flow in chronic fatigue patients.40, 41 While we did not measure cerebral blood flow in our participants, our findings support the occurrence of the reduction of PP in long covid. We are not able to conjecture further on the underlying pathophysiological abnormalities, nor make recommendation for clinical practice, but support this is an area for further research.
Potential limitations of our study include that all patients were recruited from specialist long covid clinics, so prevalences may not be applicable in the community setting. We were unable to establish whether dysautonomia and OI are related to the severity of long covid, though previous work suggests this association is unlikely to be strong.31 Our healthy volunteer comparator group was not individually matched but well-matched in overall age-sex distribution. Furthermore, our study was limited to UK patients and did adequately reflect a range of ethnic groups.
This is the largest study on prevalence of PoTS and OH in long covid to date, conducted across eight long covid clinics serving different populations, following standardized test administration, and including a healthy volunteer comparator group, allowing us to estimate the prevalence of PoTS and OH in long covid clinic patients. Our study also demonstrates the feasibility of real-world NLT testing across various clinical settings including self-administration at home. Assessing sensitivity to relaxing the criteria for diagnosis is a further strength of the work.
Our findings suggest the NLT is tolerated by most patients and should be considered as part of a holistic assessment to explore OI objectively in all patients with long covid rather than limiting it to those with typical symptoms of OI. Existing criteria for PoTS do not explain all symptoms and could be relaxed for those with at least one elevated HR rise >30 bpm with acute symptoms during the NLT or those with a sustained HR rise >20 bpm, or using modified versions of the test that allow capturing the triggers of OI such as exertion or food.42
We have demonstrated the value of the NLT in long covid as a safe and simple field test for OI, which can be performed either in a clinic setting or self-administered at home. Earlier detection of OI and dysautonomia should result in commencement of conservative measures and, if required, pharmacological management.4 Symptom trajectories and long-term outcomes of OI in long covid should be an area for future research.43 The myriad of autonomic symptoms and objective findings caused by infectious diseases is not unique to long Covid but also seen in other viral infections,29 with one study identifying chronic fatigue in 40% of patients a few years after SARS,44 and others reporting tachycardia.45 Health professionals supporting people living with long covid and other post-viral syndromes should be trained in the assessment, interpretation and management of OI and dysautonomia with clear pathways to further management.46
LOCOMOTION CONSORTIUM
Adam Mosley NHS Research Assistant [email protected]; Amy Parkin NHS Clinical Research Fellow [email protected]; Amy Rebane Patient and Public Involvment Manager [email protected]; Ashliegh Lovett NHS Clinical Research Fellow [email protected]; Carlos Echevarria Principal Investigator [email protected]; Clare Rayner Patient Advisory Group Member [email protected]; Darren Winch Patient Advisory Group Member [email protected]; Ghazala Mir Co-Investigator [email protected]; Ian Tucker-Bell Patient Advisory Group Member [email protected]; Juliet Harris NHS Research Assistant [email protected]; Karen Cook Patient Advisory Group Member [email protected]; Madeline Goodwin Research Asisstant [email protected]; Megan Ball NHS Clinical Research Fellow [email protected]; Nawar Bakerly Principal Investigator [email protected]; Nikki Smith Patient Advisory Group Member [email protected]; Rachael Evans Principal Investigator [email protected]; Ruairidh Milne Patient Advisory Group Member [email protected]; Samantha Jones NHS Clinical Research Fellow [email protected]; Sarah Elkin Principal Investigator [email protected]; Sophie Evans Patient Advisory Group Member [email protected]; Stephen Halpin Principal Investigator [email protected]; Zacchaeus Falope Principal Investigator [email protected].
ACKNOWLEDGMENTS
We would like to acknowledge and thank the participants for their time and contribution. This work is independent research funded by the National Institute for Health and Care Research (NIHR) (Long Covid grant, Ref: COV-LT2-0016). The views expressed in this publication are those of the authors and not necessarily those of NIHR or The Department of Health and Social Care.
CONFLICT OF INTEREST STATEMENT
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: all authors had financial support from National Institute for Health and Care Research for the submitted work. M. S. has received grants through his University from UKRI, is Editor-in-Chief of “Advances in Rehabilitation Science and Practice,” is Editorial Board Member of “Frontiers in Pain Research,” is President of “British Society of Physical and Rehabilitation Medicine.” D. C. G. has received grants through his University from British Heart Foundation, NHS England, and NHS National Services Scotland. T. G. is Independent SAGE member. J. S. has received grants from Wellcome Trust, Office of the Chief Scientific Advisor Scotland, and Public Health Scotland. There are no other relationships or activities that could appear to have influenced the submitted work.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




