Low prevalence of anti-Orthopoxvirus neutralizing antibodies in an urban population of Brazil
Abstract
Since 1999, Vaccinia virus (VACV) has been described as a causative agent of bovine vaccinia (BV), a zoonotic disease that occurs mainly in rural areas of Brazil. However, the circulation of VACV in urban environments and its associated burden has been poorly explored. Moreover, the current monkeypox (mpox) outbreak has raised questions regarding the immune status of the worldwide population previous vaccinated against smallpox. Hence, we conducted a cross-sectional study to better understand the prevalence of anti-OPV neutralizing antibodies (NA) and related exposure factors in a susceptible urban population of Brazil. A total of 372 individuals were sampled, yielding an overall seroprevalence of 16.9% (CI95% = 13.4–21.1), and antibodies titers ranging from 100 to 800 neutralizing units/mL. The prevalence of NA among individuals potentially vaccinated against smallpox (≥36 years old [yo]) was 24.9% (IC 95% = 19.5–31.2), and among those unvaccinated (<36yo) was 6.7% (IC 95% = 3.7–11.8). Interestingly, contact with horses was pointed out as an exposure factor for the presence of NA, however, the multivariate logistic regression analysis indicated that age ≥36yo and the presence of vaccine take were independently associated with the presence of anti-OPV NA. Our findings suggest that vulnerable populations could be subclinically exposed to VACV in urban areas, drawing attention to alternative routes of zoonotic VACV exposure. Our data is also important for better strategies to mitigate zoonotic OPV infections mainly among vulnerable populations.
1 INTRODUCTION
After smallpox was declared eradicated in 1980, routine vaccination was discontinued,1 contributing to the potential rise of other orthopoxviruses (OPV). Zoonotic OPVs can infect several mammalian host species and are associated with repeated outbreaks worldwide and spillover into humans.2-7 Animal-to-human and person-to-person OPV transmission have been documented over the past 20 years related to zoonotic OPV species mainly Vaccinia viruses (VACV), Cowpox virus (CPXV), and Monkeypox virus (MPXV).2-6
Until recently, the circulation of zoonotic OPV has been recorded in specific regions of the world, including, but not limited to, South America, Central, and West Africa, Europe, the Middle East, and Asia.2-7 However, with the current global monkeypox (mpox) outbreak, MPXV has become the most significant zoonotic OPV for humans since the eradication of smallpox, as cases were mostly due to human-to-human transmission.7, 8 More than 87 314 mpox cases and 129 deaths were confirmed, including more than 104 locations that do not customarily report mpox, which rekindled the questioning of the immune status of the population after decades of smallpox vaccine discontinuation.9, 10
Indeed, the current spread of mpox to countries where the disease is not endemic has alarmed experts looking for answers to the silent spread hypothesis. Although mpox is a mild disease and the current outbreak has a low fatality rate (<1%),11 cases of death were already reported, the first one recorded in Brazil on July 29th, 2022, in a 41-year-old man with underlying comorbidities. As of May 19th, 2023, 10 915 mpox cases have been confirmed in Brazil, the majority located in São Paulo, followed by Rio de Janeiro and Minas Gerais State.9, 12 Not surprisingly, the Southeast region of Brazil is well known as the epicenter of a vesiculopustular disease called bovine vaccinia (BV), which is caused by VACV, an OPV circulating in Brazil since 1960.4, 5
Zoonotic VACV infections have often been reported in Minas Gerais State, mostly as occupational infections.4, 5, 13-15 Rural workers in dairy farms have been identified as the leading risk group as they have direct contact with dairy cows presenting vesicular lesions on their teats.4, 5, 13-15 The presence of vesiculopustular, ulcerated, necrotic and painful lesions are observed mainly on hands of affected individuals due to its close contact with infected animals during the milking process.4, 5, 13, 14 However, lesions can spread to secondary body sites such as forearms, arms, and face. Other signals and systemic symptoms such as fever, lymphadenopathy, headache, and myalgia are also reported.4, 5, 13-15
To date, few seroepidemiological studies aiming to better understand the profile of populations at risk or protected against OPV (in case of those already vaccinated against smallpox) have been conducted in Brazil. Prevalence rates of anti-OPV neutralizing antibodies (NAs) ranging from 9.8% to 43% have been described in rural populations, possible exposed to VACV through the classical transmission route (direct contact with dairy cows).13, 16-18 Furthermore, the presence of NA has been significantly associated with age, male gender, rural workers handling bovines, and previous outbreak reported in the dairy farms.17, 18 However, individuals ≥36 years old (yo) (defined as potentially vaccinated against smallpox) are also affected, reinforcing the decrease of previous immunity against OPV.13-16, 18 In fact, significant differences in NAs titers related to age has been documented,18-22 which could be possibly related to immunosenescence (characterized as a dysregulation of innate and adaptive immunity cells associated with aging), consequently leading to a decrease in antibodies responses. Furthermore, other factors such as vaccine types, injector types, and booster schedules could also influence the durability of immune response as suggested.22
Recent studies have drawn attention to the potential circulation of VACV in urban areas of Brazil, highlighting a greater concern to public health and the burden that could be associated with human infections.4, 5, 23-25 Furthermore, questions whether individuals vaccinated against smallpox more than 40 years ago would be protected in the event of any zoonotic exposure (or even smallpox bioterrorism) is still unclear. Few studies have also shown that many individuals did not develop the vaccine take, which is an useful indicator of successful vaccination.18, 21 Previous results from our research group indicated that 61.0% of individuals from rural areas in Brazil, which were potentially vaccinated against smallpox present the vaccine take.18
Hence, considering a scenario of mpox emergence, individuals with none or very low immunity against OPV, and VACV reaching urban areas, we aimed to assess the prevalence of NAs against OPV in an urban population of Brazil that can be natural exposed to VACV, also describing associated exposure factors. In addition, this study represents an opportunity to discuss and to contribute with significant data for public health response to mitigate zoonotic OPV infections mainly in vulnerable populations, can help to subsidize strategy the vaccines implementation, such as priority groups definition.
2 MATERIALS AND METHODS
2.1 Study area and design
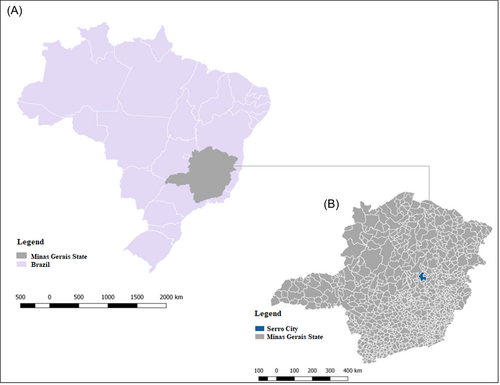
During 2015–2018, a cross-sectional study was carried out in the urban area of Serro city (18°36′17″S 43°22′46″W) (Figure 1), an important dairy basin where dairy products are culturally made by raw milk, located in Minas Gerais State, Brazil. Serro has a population of 20 835 inhabitants, with 11 060 residents in urban areas,26 and is characterized as an endemic area for BV.4, 5, 15, 18 Sample size calculation was performed using an expected prevalence of 50% and confidence interval of 95%, an accuracy of 10% around the estimate and a design effect of 2.0. Using Open-Epi version 2.3.1, a minimum sample of 372 individuals was determined for the study.
2.2 Study participants and samples collection
A structured questionnaire was applied to collect demographic data and factors potentially associated with VACV exposure. As routine smallpox vaccination was discontinued in Brazil in 1978,1 we defined individuals ≥36yo at the time of the sample collection as potentially vaccinated against smallpox, given the underlying uncertainty as they should have been vaccinated as recommended by World Health Organization. On the other hand, individuals <36yo were not vaccinated. Additionally, a clinical inspection was made on the left arm of participants born before 1978 for the presence of a smallpox vaccine scar (vaccine take), which is strongly correlates with protection. Blood samples in the absence of coagulants from individuals who voluntarily agreed to participate in the study.
2.3 Serologic analysis
A plaque reduction neutralization test (PRNT) was also performed as NAs are related to protective immunity against OPV.27 Briefly, sera samples were heated to 56°C for 30 min to denature complement system proteins and then diluted in Eagle's Minimum Essential Medium (MEM) free of fetal bovine serum (FBS) to a screening ratio of 1:40. Samples were added to the same volume (1:1) of a solution containing around 150 plaque forming units (PFU) of VACV-WR. This mixture was incubated for 16 h at 37°C. Six-well plates containing BSC-40 cells monolayers were inoculated with the mixture. Plates were incubated at 37°C for 1 h in an atmosphere with 5% of CO2. MEM supplemented with 2% FBS were added to each well and incubated again at 37°C with 5% of CO2 for 48 h. Cell monolayer were fixed with 10% formalin and stained with a 1% crystal violet solution. All samples were tested in triplicate. Samples that exhibited a minimum of 50% of plaque formation inhibition were considered positive for NAs. All positive samples were titrated according to the PRNT protocol described above. Dilutions were performed in a twofold serial dilution of the sera from 1:40 to 1:5120. The last dilution in which 50% PFU reduction was observed was used as a reference to calculate the value of neutralizing units (NU) per milliliter (NU/mL). The value was obtained by dividing 1 mL by the volume of virus/serum solution inoculated on cell monolayer and multiplying it by the least dilution that shows a 50% reduction in PFUs.
2.4 Statistical analysis
A bivariate analysis was carried out using Chi-square and Fisher's exact tests when appropriate, with a significance level of 5% (p ≤ 0.05), to determine the association between NAs and exposure factors to OPV. Relative odds ratios and 95% confidence intervals were calculated when appropriate. Variables with a significance level of p < 0.20 were considered candidates to fit in the multivariate model, including all biologically plausible two-way interactions. A backward approach was used, and the best model was defined as the one that included significantly associated variables (p < 0.05). Analysis was performed on Epi-Info software version 7.2.0.1.
3 RESULTS
3.1 Demographic characteristics of the population
A total of 372 individuals were surveyed in urban areas of Serro city, Minas Gerais State. Table 1 presents the demographic characteristics of the surveyed population. Women represented 54% of participants. The median age was 40.7 years (ranging from 5 to 94 years). The majority (64.2%) self-reported mixed race/ethnicity and had an average income of two minimum wages. The illiteracy rate among the participants was 4.6%, and 51.3% had a minimum/medium education level. Approximately 48% of individuals reported an occupational status related to service provision, while 16.1% were at schooling age, and 12% reported they were retired.
| Demographics | N (%) | PRNT positive (%)a | PRNT negative (%)a | p value | Odds ratio CI95% |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 201 (54.0) | 32 (15.9) | 169 (84.1) | 0.33 | 0.86 (0.5–1.5) |
| Male | 171 (46.0) | 31 (18.1) | 140 (81.9) | ||
| Age (years) | |||||
| <36 | 163 (43.8) | 11 (6.7) | 152 (93.3) | <0.0001 | 4.6 (2.3–9.1) |
| ≥36 | 209 (56.2) | 52 (24.9) | 157 (75.1) | ||
| Self-reported skin color | |||||
| Mixed | 239 (64.2) | 39 (16.3) | 200 (83.7) | 0.71 | NC |
| Black | 64 (17.2) | 10 (15.6) | 54 (84.4) | ||
| White | 69 (18.5) | 14 (20.3) | 55 (79.7) | ||
| Incomeb | |||||
| ≤1 min wage | 104 (27.9) | 23 (22.1) | 81 (77.9) | 0.06 | NC |
| 1–2 min wage | 145 (39.0) | 21 (14.5) | 124 (85.5) | ||
| >2 min wage | 61 (16.4) | 17 (27.9) | 44 (72.1) | ||
| Education levelc | |||||
| Elementary school or less | 191 (51.3) | 32 (16.8) | 159 (83.2) | 0.9 | NC |
| High school | 130 (34.9) | 23 (17.7) | 107 (82.3) | ||
| Higher education | 32 (8.6) | 5 (15.6) | 27 (84.4) | ||
| Have never gone to school | 17 (4.6) | 3 (17.6) | 14 (82.4) | ||
| Occupation | |||||
| Homemaker | 22 (5.9) | 4 (18.2) | 18 (81.8) | <0.0001 | NC |
| Healthcare workers | 19 (5.1) | 1 (5.3) | 18 (94.7) | ||
| Rural workerd | 32 (8.6) | 11 (34.4) | 21 (65.6) | ||
| Schooling age | 60 (16.1) | 6 (10.0) | 54 (90.0) | ||
| Retired | 45 (12.1) | 16 (35.6) | 29 (64.4) | ||
| Other | 179 (48.1) | 25 (14.0) | 154 (86.0) | ||
| Not employed | 7 (1.9) | 0 | 7 (100.0) | ||
| Totale | 372 (100.0) | 63 (16.9) | 309 (83.1) | ||
- Abbreviation: NC, not calculated.
- a Percent frequencies were calculated by line.
- b Income value in Brazilian currency during 2015–2018 increased from R$ 788.00 to R$ 954.00 (R$ 1.00 = US$ 0.2038 approximately).
- c Elementary school or less (<8 years of study), High school or more (8–12 years of study). Higher education (college degree or more).
- d Individuals that worked as rural worked in the past.
- e Totals may not add up to 100% due to missing or not reported data.
3.2 Prevalence of anti-Orthopoxvirus NAs
NAs were detected in 63 participants, representing an overall prevalence rate of 16.9% (CI95% = 13.4–21.1) (Table 2). Antibodies titers ranged from 100 to 800 NU/mL. Based on age threshold (36 years), more than half of the participants (56.2%) would have been eligible to have received a smallpox vaccine during the vaccination campaign. The prevalence rate of NA among individuals that should have received smallpox vaccination (≥36yo) was 24.9% (IC 95% = 19.5–31.2), and among those unvaccinated (<36yo) was 6.7% (IC 95% = 3.7–11.8). It is important to mention that all individuals ≤14yo (n = 31) tested negative for the presence of NA. On the other hand, only 11 individuals (8.5%) aged 15–35yo had detectable NA.
| Participants | Prevalence rate (CI95%) |
|---|---|
| Overall | 16.9 (13.4–21.1) |
| Vaccinateda (≥36 years old) | 24.9 (19.5–31.2) |
| Nonvaccinatedb (<36 years old) | 6.7 (3.7–11.8) |
| Presence of vaccine takec | |
| Yes | 35.9 (23.3–53.1) |
| No | 23.5 (15.9–34.0) |
- Abbreviation: WHO, World Health Organization.
- a Individuals ≥36 years old at the time of the study were defined as potentially vaccinated against smallpox, given the underlying uncertainty as they should have been vaccinated as recommended by WHO.
- b Individuals <36 years old at the time of the study were not vaccinated during smallpox eradication campaign.
- c The presence of vaccine take was determined by examination on left arm of each participant.
3.3 Exposure factors
Potential exposure factors to VACV are presented in Table 3. Here, we considered the presence of vaccine take as a previous form of exposure to VACV. A total of 64 individuals with evidence of smallpox vaccination (≥36yo) presented the vaccine take, and 23 of them (35.9%) had detectable NA. On the other hand, 20.0% of individuals without the vaccine take had detectable NA, suggesting a natural exposure to VACV.
| Exposure factors | N (%)a | PRNT positive (%)b | PRNT negative (%)b | p value | Odds ratio CI95% |
|---|---|---|---|---|---|
| Smallpox vaccine takec | |||||
| Yes | 64 (30.6) | 23 (35.9) | 41 (64.1) | 0.02 | 2.3 (1.2–4.4) |
| No | 145 (69.4) | 29 (20.0) | 116 (80.0) | ||
| Contact with domestic dogs | |||||
| Yes | 278 (74.2) | 34 (12.2) | 244 (87.8) | 0.1 | 2.5 (0.8–7.5) |
| No | 18 (5.8) | 5 (27.7) | 14 (72.3) | ||
| Contact with domestic cats | |||||
| Yes | 121 (32.5) | 17 (14.1) | 104 (85.9) | 0.9 | 1.1 (0.6–1.8) |
| No | 175 (47.3) | 22 (12.6) | 153 (87.4) | ||
| Contact with dairy cattle | |||||
| Yes | 63 (16.9) | 13 (20.6) | 50 (79.4) | 0.06 | 2.1 (1.0–4.3) |
| No | 234 (62.9) | 26 (11.1) | 208 (88.9) | ||
| Contact with horses | |||||
| Yes | 64 (17.2) | 14 (21.9) | 50 (78.1) | 0.03 | 2.3 (1.1–4.8) |
| No | 233 (62.6) | 25 (10.7) | 208 (89.3) | ||
| Presence of rodents in the household | |||||
| Yes | 92 (24.7) | 20 (21.7) | 72 (78.3) | 0.7 | 1.2 (0.6–2.3) |
| No | 110 (29.6) | 21 (19.1) | 89 (80.9) | ||
| Consumption of raw milk | |||||
| Yes | 95 (25.5) | 18 (19.0) | 77 (81.0) | 0.5 | 1.2 (0.6–2.2) |
| No | 277 (74.4) | 45 (16.2) | 232 (83.8) | ||
| Consumption of cheese | |||||
| Yes | 333 (89.5) | 54 (16.2) | 279 (83.8) | 0.3 | 1.6 (0.7–3.4) |
| No | 39 (10.5) | 9 (23.0) | 30 (77.0) | ||
| Total | 372 (100.0) | 63 (16.9) | 309 (83.1) | ||
- a Totals may not add up to 100% due to missing or not reported data.
- b Percent frequencies are shown by line.
- c Vaccine take were calculated only among individuals potentially vaccinated against smallpox according to the age threshold.
We also evaluated the direct contact with domesticated animals, such as dogs, cats, bovines, and equids. A total of 278 (74.2%) participants reported they have contact with dogs, while 121 (32.5%) said they have contact with cats. Regarding farming animals, 63 (16.9%) participants reported they had contact with dairy cattle and 64 (17.2%) had previous contact with horses.
We further inquired about the presence of rodents at the domicile or surroundings. A total of 92 individuals (24.7%) reported they saw rodents in their household (inside or in the backyard), while 9.5% of them reported seeing rodents in the surroundings such as on the street or abandoned land/properties. A total of 56 individuals (15.0%) reported they had previous contact with wild animals such as rodents, marsupials, and nonhuman primates.
The consumption of raw milk (unpasteurized) was reported by 95 individuals (25.5%), while most of them (89.5%) regularly consume cheese made from raw milk.
Potential exposure factors to VACV in young population (those <36yo) unvaccinated with detectable anti-OPV NA are presented in Table 4. Among this group, eight individuals (72.7%) reported contact with a dog and the presence of rodents on the property; seven (63.6%) the consumption of artisanal cheese (raw); six (54.5%) raw milk consumption; three (27.3%) production of milk derivatives; and two (18.2%) contact with cat, contact with bovine e/or equine and milking.
| Gender | Age (years) | Contact with dogs | Contact with cats | Previous contact with cattle and/or horses | Reported the presence of rodents around the property | Consumption of raw milk | Consumption of artisanal cheese | Previous history of milking practice | Previous history of participating in artisanal cheese production |
|---|---|---|---|---|---|---|---|---|---|
| F | 17 | Yes | No | No | Yes | No | No | No | No |
| Fa | 15 | Yes | Yes | No | No | No | Yes | No | No |
| Fa | 34 | Yes | Yes | No | Yes | No | Yes | Yes | Yes |
| Ma | 17 | Yes | No | No | Yes | Yes | Yes | No | No |
| M | 26 | No | No | No | Yes | Yes | Yes | No | No |
| F | 24 | No | No | No | Yes | Yes | Yes | No | No |
| Ma | 17 | Yes | No | Yes | Yes | Yes | No | No | No |
| Ma | 15 | Yes | No | No | Yes | Yes | No | Yes | Yes |
| F | 21 | No | No | No | No | No | No | No | No |
| Fa | 22 | Yes | No | No | No | No | Yes | No | No |
| Ma | 30 | Yes | No | Yes | Yes | Yes | Yes | No | Yes |
- Note: F = female, M = male.
- a Individuals who reported contact with domestic animals (dogs and cats) and the consumption of raw milk and artisanal cheese.
3.4 Factors significantly linked to the presence of anti-OPV antibodies
Demographic characteristics significantly associated with the presence of NA in the univariate analysis were age ≥36yo (crude odds ratio [crOR] = 4.6; CI95% = 2.3–9.1, p < 0.0001) and occupation as rural workers (crOR = 2.3; CI95% = 1.1–4.8, p < 0.0001). Exposure factors for VACV infection associated with the presence of NA in the univariate analysis were the presence of vaccine take (crOR = 2.3; CI95% = 1.2–4.4, p = 0.02) and contact with horses (crOR = 2.0; CI95% = 1.1–4.8, p = 0.03).
Variables independently associated with the presence of NA in logistic regression model were age ≥36yo and the presence of vaccine take. Individuals older than 36 years were three times more likely to present NA than younger individuals (OR = 3.4; CI95% = 1.6–7.2; p = 0.0009). Furthermore, individuals that had a vaccine take were almost two times more likely to present NA than those that did not have a vaccine take (OR = 2.2; CI95% = 1.2–4.3, p = 0.01).
4 DISCUSSION
Cessation of smallpox vaccination 42 years ago increased the probability of zoonotic OPV infections in humans.1-3, 22 The current mpox outbreak worldwide corroborates the susceptibility of the young population (those <42yo) due to the lack of cross-protective immunity against OPV.7, 8, 11, 22 However, several studies have shown whether different populations vaccinated against smallpox could still maintain or not some residual protective immunity against OPV.20, 28-34
Populational studies conducted in the United States and Japan revealed that individuals vaccinated against smallpox maintained a stable and long-lasting antibody response against OPV.28, 29 On the other hand, a study performed in China showed a low prevalence and low antibody titers.20 Other studies showed that high titers of anti-OPV antibodies and long-lasting humoral immunity could be correlated with multiple vaccinations,30 as well as a strong NA response could be the main protective mechanism in re-exposures to OPV.31 These data corroborate our findings in which 24.9% of vaccinated individuals were five times more likely to have NA when compared with nonvaccinated ones (p < 0.001).
Even in endemic region, the prevalence of anti-OPV NA in our study was lower when compared to the prevalence in most of rural populations surveyed in Brazil (rates ranging from 27.9% to 43.0%).13, 16, 18 However, we found that the population located in urban areas of Serro city showed a higher prevalence compared to the study performed by Figueiredo et al.17 (although the authors sampled a low number of individuals in that study). Contrasting with data from other countries, our prevalence was lower than what found in a urban population from South India,35 but interestingly much higher when compared to many individuals surveyed in Bolivia, France, Laos, Mali, and Thailand, that showed none or very low titers of NA response against OPV.36-38
The persistence of NA found here could be associated with continuous exposure to a naturally circulating OPV, as suggested.4, 5, 15, 30 However, we also found that 75.1% of individuals potentially vaccinated against smallpox tested negative for NA, suggesting that many individuals could have a decline in antibody titers, corroborating previous findings.36, 37 This fact also highlights the vulnerability of most individuals (even the vaccinated ones), to zoonotic OPV infections, especially to mpox, a high pathogenic OPV causing a current outbreak worldwide.7-10 Furthermore, a recent study showed that a patient vaccinated against smallpox 8 years ago was still susceptible to mpox, presenting mild disease.36 Also, case-series of individuals previously immunized against smallpox has been diagnosed with mpox during the current outbreak,39, 40 as well as individuals recently vaccinated in 2022.37
Interestingly, only 35.0% of the individuals potentially vaccinated against smallpox had the vaccine take, which is historically categorized as a protective marker of successful smallpox vaccination.1, 19, 21 However, 23/64 individuals that presented the vaccine take had detectable NA, corroborating the findings described by Tan21 and coworkers in which vaccinated individuals failed in developing the take, and consequently an antibody response. In fact, some cases of mpox re-infection among men who have sex with men with multiple exposure to mpox, despite of the presence of detectable NA were described, contradicting the “full protection” conferred by NA.41-43 Nevertheless, in the study performed by Kennedy et al, the entire population selected based on the vaccine take presented a NA response.19 Taken together, these findings highlight the need of carefully address whether individuals vaccinated ≥40 years ago could still be protected in cases of OPV emergence (such as circulation of VACV in urban areas and the current mpox outbreak), which could help formulating vaccination strategies in priority groups.
The OPV seroprevalence has been used as an indicator of zoonotic OPV exposure/circulation. Here, 11 unvaccinated individuals (6.3%) that did not report any history of VACV-like infection or contact with individuals infected by VACV had detectable NA. This result suggests those individuals could have potentially been exposed to VACV through different sources other than the classic contact with infected dairy cattle as previously suggested. In fact, none of the evaluated exposure factors significantly influenced the presence of NA in unvaccinated individuals. However, two individuals reported performing milking in the past, and two other individuals reported previous contact with dairy cattle and horses, which is strongly associated with VACV exposure.4, 5, 13-15, 18
It is also important to mention that eight unvaccinated participants that had detectable NA reported contact with domestic dogs, and two of them reported contact with domestic cats. Previous studies from our group have suggested the silent circulation of VACV in urban environments, the potential of dogs and cats in zoonotic VACV transmission chain, as well as the burden for human and animal health in urban centers.24-26 Additional studies are needed to confirm if pets (i.e., dogs and cats) are indeed susceptible and can transmit VACV to humans causing disease, similar to CPXV infections through infected cats (and potentially by dogs) in Europe.2, 44-46 In the current mpox outbreak, evidence of human-to-dog transmission was reported46 and one dog MPXV case was confirmed in Brazil highlighting the importance of OPV surveillance in these animals.47
Seven unvaccinated individuals with detectable NA reported consumption of artisanal cheese and six of them reported consumption of made from raw milk, also suggesting the role of dairy products as alternative routes for zoonotic VACV transmission. Indeed, VACV has been detected in unpasteurized dairy products, however the effect of such contamination on VACV transmission to humans is still unknown.5, 48-50 Although the consumption of raw milk and artisanal cheese was not significantly associated with NA, additional population-based studies and further assessments regarding dairy products as potential alternative routes of disease spread are necessary for guiding public health authorities in planning and implementation of preventive and control programs.
Our study has limitations. It was hard to precisely estimate if individuals sampled here had contact with infected dairy cows in the past. Serro city is located at the countryside area of Minas Gerais State, and it is categorized as a “rural” city. Moreover, many people have access to farms, participating in farm tours to experience the local culture, hence it could be hard to approach individuals with none or very few contact with farm animals. Furthermore, vaccination history was inferred by means of age and the presence of vaccine take, but no vaccination health records or datasets were available for analysis. Additionally, 63.0% of unvaccinated individuals that tested positive for NA reported they had contact with domestic animals and consumption of raw milk and artisanal cheese. Thus, further studies are necessaries to accurately investigate the influence of different routes of zoonotic OPV infections. However, our findings are important in a public health basis and reinforce the hypothesis of alternative routes of zoonotic VACV transmission, which can contribute to the virus circulation in urban environments.4, 15, 23-25
In conclusion, our results surprisingly confirm a low seroprevalence of anti-OPV NA in a previously smallpox-vaccinated urban population of Brazil and indicate regular contact with zoonotic OPV, even in the absence of recognized outbreaks. Data presented here are helpful to public health authorities and intended to improve OPV control practices, increasing awareness and minimizing the potential risk of sanitary and hygienic conditions. Our study also highlights the need to strengthen virological surveillance to reduce OPV infections’ economic and medical burden. Furthermore, in the context of the current mpox outbreak, it brings a recent analysis of seroprevalence in a population exposed to other OPV, which may be useful in the elaboration of vaccination strategies guidelines and other public health policies.
AUTHOR CONTRIBUTIONS
Jaqueline Silva de Oliveira, Galileu Barbosa Costa, and Giliane de Souza Trindade: conceptualized and designed this study. Jaqueline Silva de Oliveira, Galileu Barbosa Costa, Ana Gabriella Stoffella Dutra, and Danilo Bretas de Oliveira: participated in field expeditions, samples and data collection. Jaqueline Silva de Oliveira, Galileu Barbosa Costa, Ana Gabriella Stoffella Dutra, Iago José da Silva Domingos, Pedro Starling Pereira Martins da Costa, and Pedro Henrique Bastos e Silva: worked on samples processing, storage, and performed the laboratory experiments. Jaqueline Silva de Oliveira and Galileu Barbosa Costa: led and performed the data analysis. Erna Geessien Kroon, Danilo Bretas de Oliveira, and Giliane de Souza Trindade: supervised and all materials. Jaqueline Silva de Oliveira and Galileu Barbosa Costa: wrote the original draft. All authors had full access to all the data, revised the manuscript for important intellectual content, and edited the final manuscript. All authors had final responsibility for the decision to submit for publication.
ACKNOWLEDGMENTS
We thank colleagues from Laboratório de Vírus for their excellent technical support. We are grateful for the assistance of Secretaria Municipal de Saúde from Serro City during field expeditions. Financial support was provided by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) (grant numbers 88882.348380/2010-1), Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG) (Grant Numbers APQ-04039-17 and APQ-0104018), and Câmara Pox – Ministério da Ciência, Tecnologia e Inovações (MCTI/CNPq, Grant Number 405249/2022-5). Giliane de Souza Trindade and Erna Geessien Kroon are researchers from CNPq.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Ethical clearance was obtained from the Research Ethics Committee of Universidade Federal de Minas Gerais under the registration protocol 1.974.249. All adult participants provided informed written consent before interview participation and collection of specimens. Participants <18 years of age provided age-appropriate assent, and parents or guardians provided consent on their behalf.
Open Research
DATA AVAILABILITY STATEMENT
All data are provided in the manuscript and the related supplements.




