Vaccination status for mild and asymptomatic infections with SARS-CoV-2 Omicron BA.2 variant in Shanghai
Yong Yin, Jilei Lin, Shuhua Yuan, Erzhen Chen, Junhua Zheng, and Wei Wang contributed equally to this study.
Abstract
This study aimed to evaluate the effects of different vaccine regimens on mild and asymptomatic infections with SARS-CoV-2 Omicron BA.2 variant in Shanghai. All asymptomatic patients and those with mild symptoms of Omicron infections were recruited from three major Fangcang shelter hospitals between March 26, 2022 and May 20, 2022. Nucleic acid for SARS-CoV-2 by real-time reverse-transcription polymerase chain reaction methods in nasopharyngeal swabs was assessed every day during the hospitalization. The value of cycle threshold lower than 35 was considered as positive result of SARS-CoV-2. A total of 214 592 cases were included in this study. The proportion of the asymptomatic patients was 76.90% and 23.10% of the recruited patients had mild symptoms. The median (interquartile range [IQR]: 25–75) duration of viral shedding (DVS) was 7 (5–10) days among all participants. The DVS varied greatly among different age groups. Children and the elderly had longer DVS compared with the adults. The booster shot of inactivated vaccine contributed to the shorter DVS in patients aged ≥70 years compared with the unvaccinated patients (8 [6–11] vs. 9 [6–12] days, p = 0.002]. Full inactivated vaccine regimen contributed to the shorter DVS in patients aged 3–6 years (7 [5–9] vs. 8 [5–10] days, p = 0.001]. In conclusion, the full inactivated vaccine regimen on children aged 3–6 years and booster inactivated vaccine regimen on the elderly aged ≥70 years appeared to be effective in reducing DVS. The booster vaccine regimen should be rigorously promoted and implemented.
1 INTRODUCTION
Since the end of 2019, the coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been spreading rapidly worldwide.1 After controlling the initial COVID-19 epidemic in Wuhan city in early 2020, the massive outbreak of SARS-CoV-2 was prevented in China over the past 2 years.2 Compared with more than 500 million confirmed cases and over 6 million deaths due to SARS-CoV-2 infection worldwide, it was estimated that more than 150 million lives might be saved by the “dynamic zero” COVID-19 policy in China.3
SARS-CoV-2 Omicron variant emerged in November 2021 and has been spreading rapidly across the world since then. SARS-CoV-2 Omicron infections continue to increase in China due to its increased transmissibility and immune escape capability.4, 5 In recent months, the incidence of SARS-CoV-2 Omicron infections increased rapidly in Shanghai, China.6 According to the Shanghai Municipal Health Commission, as of June 23, 2022, there were 627 107 confirmed cases including 591 518 asymptomatic cases and patients with mild symptoms in Shanghai. Asymptomatic patients and those with mild symptoms accounted for the majority of Omicron infections and played an important role in the transmission of COVID-19.7-9 Most developed countries have abandoned strict public health measures and no longer perform large scale and frequent viral nucleic acid screenings. Therefore, the proportion of asymptomatic Omicron infections or the infections with mild symptoms might be under-reported by these countries.10-12 While in China, according to the “dynamic zero” COVID-19 policy, all infections, regardless with or without symptoms, must be confirmed as soon as possible with large scale and frequent viral nucleic acid screenings. Therefore, the evidence from the current epidemic in Shanghai may highly reflect the reality compared with the previous reports.10, 12
The overall vaccination rate is more than 70% in Shanghai,3 but the breakthrough infections have emerged in many vaccine recipients. This study aimed to evaluate the association of different vaccine regimen for mild and asymptomatic infections with SARS-CoV-2 Omicron BA.2 variant. Furthermore, the clinical characteristics and the duration of viral shedding (DVS) of patients without any symptoms or with mild symptoms were also assessed.
2 METHODS
2.1 Study design and participants
This retrospective, multicenter, observational study was conducted in Shanghai, China. According to the “dynamic zero” COVID-19 policy, large scale viral nucleic acid screenings were conducted frequently in communities, institutions, and clinics of Shanghai. Regardless of sex and age, the confirmed cases without any symptoms or with mild symptoms identified by centers for disease control and prevention (CDC) were required to be admitted to Fangcang shelter hospitals that were the alternative care sites.13 The Fangcang shelter hospitals in Shanghai were large-scale, temporary hospitals, which were rapidly built by converting existing public facilities, such as stadiums and exhibition centers, into health-care facilities. Before the admission, doctors will evaluate the patients' condition, and only patients without any symptoms or with mild symptoms can be finally admitted to the Fangcang shelter hospitals. By isolating and treating only mild and asymptomatic cases, Fangcang shelter hospitals in Shanghai freed up the inpatient units providing respiratory support and intensive care. All patients with SARS-CoV-2 infection who had no symptoms or mild symptoms were recruited from three major Fangcang shelter hospitals (National Convention and Exhibition Center, New International Expo Center, and Expo exhibition hall) between March 26, 2022 and May 20, 2022. These Fangcang shelter hospitals provided more than 60 000 beds.
The exclusion criteria included any of the following: (1) the results of viral nucleic acid test were still positive till May 20, 2022; (2) time from illness onset to being admitted to Fangcang shelter hospitals was more than 2 weeks; and (3) patients' information was missing or obviously incorrect.
2.2 Definition
Mild and asymptomatic infection with SARS-CoV-2 Omicron variant was defined as follows14 (according to the ninth edition of “Diagnosis and treatment of pneumonia caused by SARS-CoV-2,” http://www.nhc.gov.cn/): (1) Patients with positive results of nucleic acid for SARS-CoV-2 by real-time reverse-transcription polymerase chain reaction (RT-PCR) methods in nasopharyngeal swabs, and the positive patients would be finally confirmed by the CDC of Shanghai. (2) Patients without any symptoms were considered as asymptomatic infections. (3) Patients without dyspnea, decrease of oxygen saturation, progressive symptoms, pneumonia signs in chest imaging or without the need of escalation of medical care were considered as mild infections.
The “dynamic zero” COVID-19 policy in China refers to a strategy of quickly identifying and containing any new COVID-19 outbreaks through targeted lockdowns, mass testing, contact tracing, and quarantine measures. The goal of this policy is to prevent the spread of COVID-19 within the community and maintain zero local transmissions of the virus. All COVID-19 patients need to be isolated in Fangcang hospitals and must test negative for the virus before being discharged.
2.3 Data collection
Patients' information on national identification numbers, date of birth, gender, clinical manifestations, past medical history, date of illness onset, and the different vaccination status (types and doses) was recorded in Fangcang shelter hospitals. There are three types of vaccines including inactivated vaccine (Sinovac and Sinopharm), adenovirus vector vaccine (CanSinoBIO), and protein subunit vaccine (Zifivax). The entire viruses cultured in vitro and inactivated by chemical reagents are the vaccine components of inactivated vaccine. Engineered viruses with replication-attenuated carrying genetic material of viral proteins or polypeptides are the vaccine components of adenovirus vector vaccine. Cell-expressing systems express viral proteins or peptides systemically are the vaccine components of protein subunit vaccine. The study of Li et al. shows the detailed information of these vaccine.15 One shot of adenovirus vector vaccine,16 two shots of inactivated vaccine, and three shots of protein subunit vaccine were regarded as the full vaccine regimen. In January 2021, healthy adults (18–59 years old) started to receive the vaccines against COVID-19 in China. In the later period, the elderly and children (>3 years old) will be gradually vaccinated with COVID-19 vaccine. Inactivated vaccine is the first vaccine used in China, and it is also the most widely used vaccine. Adults and the elderly can receive the full and booster vaccine regimens (inactivated vaccine, adenovirus vector vaccine, and protein subunit vaccine). Children are only allowed to receive the inactivated vaccine, the booster shot of vaccine is not implemented for children in China. Although the vaccination is not mandatory, the majority of the population received the vaccination by the government propaganda.
2.4 Nucleic acid for SARS-CoV-2
Nucleic acid for SARS-CoV-2 by RT-PCR methods in nasopharyngeal swabs was assessed every day during the hospitalization. According to the governmental COVID-19 policy (the zero dynamic policy), the negative viral load is the necessary condition for discharge. The value of cycle threshold higher than 35 was considered as negative result of SARS-CoV-2 while cycle threshold lower than 35 was considered as positive. The date of the second test of the two consecutive negative nucleic acid tests was regarded as the date of negative viral load. Daily nucleic acid testing for SARS-CoV-2 for patients were conducted in Fangcang shelter hospital. The DVS was defined as the time (day) from illness onset (the first time of positive viral load test) to the negative viral load.
2.5 Statistical analysis
Continuous data were compared by using Mann–Whitney U test and were presented as medians with interquartile range [IQR]: 25–75 for variables were almost not normally distributed. Categorical variables were analyzed by the χ2 test or Fisher's exact test as appropriate and expressed as numbers (n) and percentages (%). Statistical significance was set at p < 0.05 (two-tailed). All statistical analyses were performed using R software 4.1.0 and SPSS Statistics 25.0.
3 RESULTS
3.1 Characteristics of the included population
A total of 236 084 patients without any symptoms or with mild symptoms were hospitalized in three major Fangcang shelter hospitals between March 26, 2022 and May 20, 2022. According to the inclusion and exclusion criteria of this study, 214 592 cases were finally included in the analysis. Supporting Information: Figure S1 shows the detailed information of the selection process. Patients aged 18–69 years accounted for the majority of all the study participants (92.87%), while the people aged <18 or ≥70 years made up only 5.25% and 1.88% of all the study subjects, respectively. The median time from illness onset to being admitted to Fangcang shelter hospitals was 2 days. Table 1 shows the detailed information about the characteristics of study participants.
| Value | |
|---|---|
| Sample size | 214 592 |
| Sex (male, %) | 126 584 (58.99%) |
| Mean age (years old, m ± SD) | 41.59 ± 15.47 |
| Age group (n, %), y | |
| <7 | 2947 (1.37%) |
| 7–13 | 4701 (2.19%) |
| 14–18 | 3617 (1.69%) |
| 18–29 | 42 379 (19.75%) |
| 30–44 | 66 950 (31.20%) |
| 45–59 | 67 816 (31.60%) |
| 60–69 | 22 156 (10.32%) |
| ≥70 | 4026 (1.88%) |
| Days from illness onset to being admitted to hospitals (days, median [IQR: 25–75]) | 2 (1-4) |
| Site of screening (n, %) | |
| Clinics | 56 393 (26.28%) |
| Screening in community | 94 523 (44.05%) |
| Screening in institutions | 31 579 (14.72%) |
| Nucleic acid test sites | 32 097 (14.96%) |
| Clinical symptoms (n, %) | |
| Cough | 43 041 (20.06%) |
| Sputum | 23 082 (10.76%) |
| Fever | 9294 (4.33%) |
| Muscle soreness | 8983 (4.19%) |
| Fatigue | 11 554 (5.38%) |
| Nasal symptoms (runny/stuffy/sneeze) | 3701 (1.72%) |
| Throat soreness | 4054 (1.89%) |
| Oral symptoms (hypogeusia/parched) | 760 (0.35%) |
| Olfactory dysfunction | 441 (0.21%) |
| Headache | 2247 (1.05%) |
| Chest pain | 414 (0.19%) |
| Dyspnea | 105 (0.05%) |
| Ocular symptoms (conjunctivitis/dry eyes) | 84 (0.04%) |
| Abdominal symptoms (vomit/abdominal pain/nausea) | 446 (0.21%) |
| Asymptomatic | 165 018 (76.90%) |
| Underlying diseases (n, %) | |
| Cardiovascular diseases | 7474 (3.48%) |
| Cerebral diseases | 1555 (0.72%) |
| Endocrine diseases | 1140 (0.53%) |
| Respiratory diseases | 1553 (0.72%) |
| Abdominal diseases | 1434 (0.67%) |
| Tumor | 602 (0.28%) |
| Other diseases | 2925 (1.36%) |
| No | 199 900 (93.15%) |
| Type of vaccine (n, %) | |
| Unvaccinated | 47 294 (22.04%) |
| Inactivated vaccine | 160 887 (74.97%) |
| Adenovirus vector vaccine | 4196 (1.96%) |
| Protein subunit vaccine | 2215 (1.03%) |
| Vaccination status (n, %) | |
| Unvaccinated | 47 294 (22.04%) |
| Partial | 5510 (2.57%) |
| Full (without booster) | 69 461 (32.37%) |
| Booster | 92 327 (43.02%) |
| Duration of viral shedding (days, median [IQR: 25–75])a | 7 (5–10) |
| Duration in Fangcang shelter hospitals (days, median [IQR: 25–75]) | 7 (5–10) |
- Abbreviations: IQR, interquartile range; m ± sd, mean ± standard deviation.
- a Duration of viral shedding: the time from illness onset to the negative viral load.
There were 126 584 male and 88 008 female patients. The ratio of male to female was higher in the patients aged 14–39 years compared with other age groups (Supporting Information: Figure S2A). The number of the patients with one or more underlying diseases was 14 692 (6.85%). The patients aged ≥60 years had higher proportion of underlying diseases compared with other age groups (Supporting Information: Figure S2A). The proportion of the asymptomatic patients was 76.90% in this study. The top five symptoms were similar across all age groups, including cough, sputum, fever, fatigue, and muscle soreness (Supporting Information: Figure S2B). Supporting Information: Tables S1 and S2 provide detailed information for Supporting Information: Figure S2.
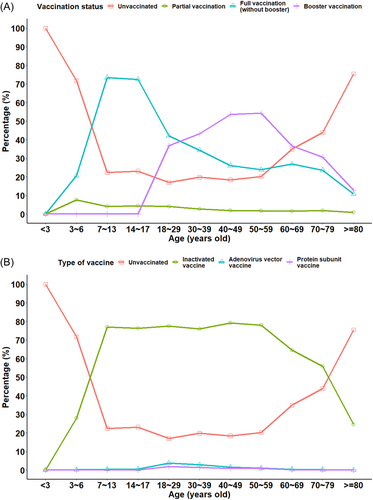
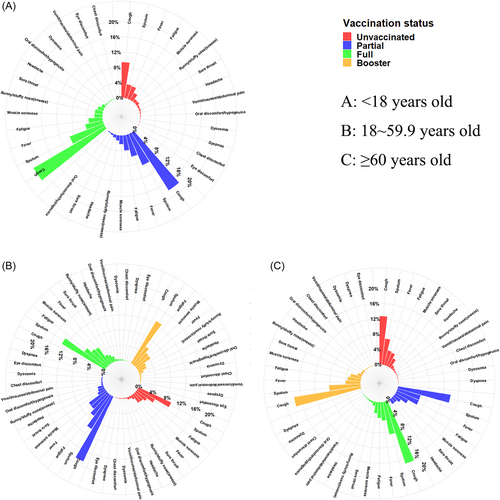
3.2 Vaccination status and clinical symptoms
The overall full vaccination rate was 75.39% and only 43.02% patients had received booster vaccination, and less than 25% of patients aged <7 or ≥80 years were fully vaccinated (Figure 1A). Inactivated vaccine accounted for the 96.17% of the vaccine, and accounted for the highest proportion of vaccine across all age groups (Figure 1B). Figure 2A shows that partial and full inactivated vaccine regimen could not reduce the incidence of clinical symptoms in children aged 3–17.9 years. Figure 2B,C shows that partial, full, and booster-inactivated vaccine regimen could not reduce the incidence of clinical symptoms adults and elderly participants. Similar results of the adenovirus vector vaccine and protein subunit vaccine were shown in Supporting Information: Figures S3 and S4.
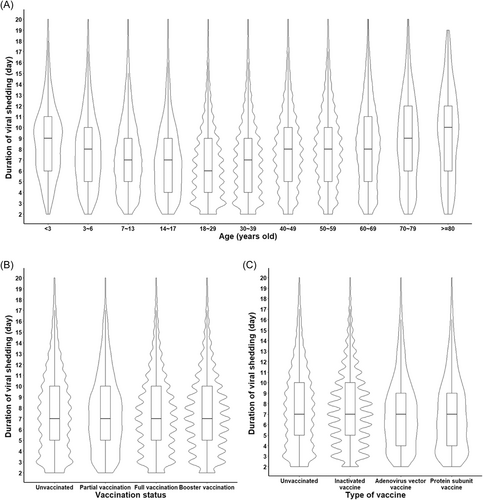
3.3 Vaccination status and DVS
Our results showed that the DVS varied greatly among different age groups, children and elderly participants had longer DVS compared with adults. The patients aged 18–29 years had the shortest duration (median [IQR: 25–75): 6 [4–9] days) while those aged ≥80 years had the longest duration (median [IQR: 25–75]: 10 [6–13] days) (p < 0.001) (Figure 3A). All median of DVS of patients with different vaccination status were 7 days (IQR: 25–75: 5–10) (Figure 3B). All median of DVS of patients with different types of vaccines were 7 days (IQR: 25–75: 5–10) (Figure 3C).
We also analyzed the DVS of patients across different age groups with different vaccination status. Compared with the unvaccinated patients, the booster vaccine regimen contributed to the shorter DVS in patients aged ≥70 years (8 [6–11] vs. 9 [6–12] days, p = 0.002) (Figure 4A). The full vaccine regimen did not reduce the DVS compared with the unvaccinated patients aged ≥70 years (8 [6–12] vs. 9 [6–12] days, p = 0.057) (Figure 4A). Compared with the unvaccinated patients, the booster-inactivated vaccine regimen contributed to the shorter DVS in patients aged ≥70 years (8 [6–11] vs. 9 [6–12] days, p = 0.002) (Figure 4B). However, the full inactivated vaccine regimen did not reduce the DVS compared with the unvaccinated patients aged ≥70 years (8 [6–12] vs. 9 [6–12] days, p = 0.072) (Figure 4B). Compared with the unvaccinated patients aged 3–6 years, full inactivated vaccine regimen contributed to the shorter DVS in patients aged 3–6 years (7 [5–9] vs. 8 [5–10] days, p = 0.001) (Figure 4B). The patients aged ≥60 years with booster adenovirus vector vaccine regimen seems to have a shorter DVS compared with the unvaccinated patients aged ≥60 years, however, the difference was insignificant (8 [5.75–10] vs. 9 [5–12] days, p = 0.432) (Figure 4C). There was no significant effect of full or booster adenovirus vector vaccine regimen on DVS compared with the unvaccinated patients in every group (all p > 0.05) (Figure 4C). The full protein subunit vaccine regimen contributed to the shorter DVS in the patients aged 30–39 years compared with the unvaccinated patients (6 [4–9] vs. 7 [4–9] days, p < 0.001) (Figure 4D), but no significant difference was observed in partial protein subunit vaccine regimen (5 [4–9] vs. 7 [4–9] days, p = 0.161) (Figure 4D). The small sample size of patients with partial protein subunit vaccine regimen might be the reason of the insignificant statistical result of DVS between patients with partial protein subunit vaccine regimen and unvaccinated patients. The patients aged 40–49 years with full or partial protein subunit vaccine regimen seems to have a shorter DVS compared with the unvaccinated patients aged 40–49 years, however, both p values were insignificant (7 [5–10] and 7 [5.25–9] vs. 8 [5–10] days, p = 0.922 and 0.827) (Figure 4D). The patients with full protein subunit vaccine regimen did not have shorter DVS compared with the unvaccinated patients aged ≥60 years (8 [4–10] vs. 9 [5–12] days, p = 0.179) (Figure 4D).
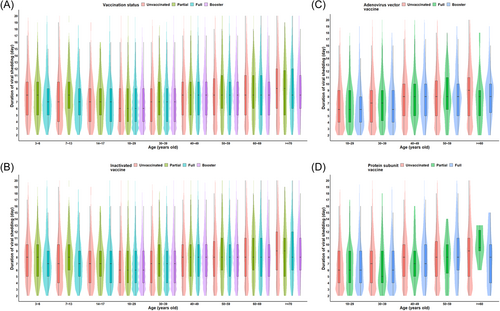
4 DISCUSSION
This study provides an initial assessment of epidemiological characteristics of asymptomatic patients and those with mild symptoms of Omicron infections in Shanghai and shows the relationship between different vaccination status and DVS. Our results show that the DVS varied greatly among different age groups, children and elderly participants had longer DVS compared with adults. The full inactivated vaccine regimen contributed to shorter DVS in children aged 3–6 years. The booster-inactivated vaccine regimen contributed to shorter DVS especially in the people aged ≥70 years. The full protein subunit vaccine regimen contributed to the shorter DVS in the patients aged 30–39 years compared with the unvaccinated patients.
According to the Shanghai Municipal Health Commission, as of June 23, 2022, it was reported that the proportion of asymptomatic cases and patients with mild symptoms was 94.32% of all confirmed cases in Shanghai. In this study, we found that asymptomatic patients and those with mild symptoms accounted for 76.90% and 23.10% of all patients, respectively, across three major Fangcang shelter hospitals in Shanghai. The proportion of asymptomatic patients in this study was higher than previous reports,17-19 and it may be because many Omicron infections without any symptoms might not be detected in previous studies, which could lead to under-reporting bias. One previous study indicated that the proportion of infections with clinical symptoms was overrated without large-scale viral nucleic acid screening.20
The proportion of the patients with booster vaccination in this study was lower than the proportion of population with booster vaccination in Shanghai. This result suggests that the booster vaccination may contribute to a reduction of breakthrough infection of Omicron. One previous study showed that S-specific memory B cells and Omicron cross-reactive T-cell responses activated by booster vaccination (CoronaVac) contributed to reduced frequencies of breakthrough infection.21 However, the undeniable fact is that despite many people receiving the full and booster vaccination, Omicron is currently causing a large number of breakthrough infections. The immune responses induced by vaccine may be influenced by the genetic variant of SARS-CoV-2. Previous one study showed that less immunogenic than Delta may be the reasons of low COVID-19 vaccine effectiveness against omicron variant.22 Neutralizing activity of antibodies for the Omicron variants was reduced significantly compared with the Beta and Delta.23, 24 As Omicron becomes the dominant variant worldwide and causes the significant amount of breakthrough infections, we need to explore more effective vaccines for Omicron.
Our results showed that the booster shot of inactivated vaccine shortened the DVS in patients aged ≥70 years, whereas a full inactivated vaccine regimen did not shortened the DVS in patients aged ≥70 years. A previous study showed that neutralizing antibody potency enhanced by three doses of CoronaVac may reduce the risk of infection against ongoing BA.2.21 The neutralizing antibody induced by three doses of an inactivated vaccine may be one of the reasons that shortened the DVS in patients aged ≥70 years. Moreover, the booster shot of inactivated vaccine was more effective than the full inactivated vaccine regimen in reducing DVS in patients aged ≥70 years. However, our results showed that the effect of full and booster adenovirus vector vaccine regimen on DVS was similar. And the booster adenovirus vector vaccine regimen did not get a more significant benefit than the full adenovirus vector vaccine regimen in reducing DVS. Previous study showed that the efficacy was similar between full and booster doses of adenovirus vector vaccine, despite decreased T-cell responses and increased antibody responses after the booster dose.25 Antivector immunity of the adenovirus vector vaccine may be the reason for the similar effect.26
Our findings may have important implications for health policy makers. First, age is a significant factor in influencing vaccine efficacy and DVS, and it is more important for the elderly and children to receive full vaccination than young adults. Interestingly, this evidence was also found in unvaccinated people that age plays an important role in influencing DVS. Previous one study showed that coordinated SARS-CoV-2-specific adaptive immune responses were associated with severity of the disease in COVID-19, suggesting roles for both CD4+ and CD8+ T cells in protective immunity.27 However, coordination of SARS-CoV-2 antigen-specific responses was disrupted in individuals ≥65 years old.28 Another study showed that neutralizing antibody activity was reduced in children COVID-19 cohorts compared with adult COVID-19 cohorts. Therefore, children and the elderly have longer DVS than adult. Second, as DVS differed with age, we should explore a more reasonable quarantine time for different age groups. Third, the full and booster vaccinations were associated with the shorter DVS, so the previous full vaccine regimen and a booster shot against COVID-19 should be promoted and implemented for the unvaccinated population.
Limitations of this study should be acknowledged. First, this is a multicenter, retrospective study with only one-third of the Omicron infections in Shanghai, and therefore, the conclusion should be drawn with caution. Second, some information was self-reported, which may lead to recall bias. Furthermore, the clinical information (from illness onset to hospitalization) was collected in the hospital admission process, and some symptoms that occurred in the later stages of infection might be missed.
5 CONCLUSION
In conclusion, the DVS varied greatly among different age groups, children and elderly participants had longer DVS compared with adults. The full inactivated vaccine regimen on children aged 3–6 years and a booster inactivated vaccine regimen on the elderly aged ≥70 years appeared to be effective in reducing DVS, the full protein subunit vaccine regimen contributed to the shorter DVS in the patients aged 30–39 years. The previous vaccination against COVID-19 pandemic should be rigorously promoted and implemented for the unvaccinated population.
AUTHOR CONTRIBUTIONS
Yong Yin, Jilei Lin, and Shuhua Yuan conceptualized and designed the study, supervised data collection, carried out the initial analyses, drafted the initial manuscript. Yi He, Bin Dong, and Fen Zhang designed the data collection instruments and collected data. Shilu Tong coordinated and supervised data collection, assisted in the statistical analysis, and revised the manuscript. Erzhen Chen, Junhua Zheng, and Wei Wang conceptualized and designed the study, supervised data collection, reviewed and revised the manuscript. All authors critically reviewed the manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
The study was approved by the ethics committee of the Shanghai Children's Medical Center and conducted according to the Declaration of Helsinki guidelines (SCMCIRB-K2022069-1). The requirement of obtaining informed consent was waived because this study was conducted retrospectively, and all patients' information was handled anonymously.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions. The deidentified individual participant data set used in this article will be made available with publication upon reasonable request.




