Hypertension is still a moving target in the context of COVID-19 and post-acute COVID-19 syndrome
To the Editor,
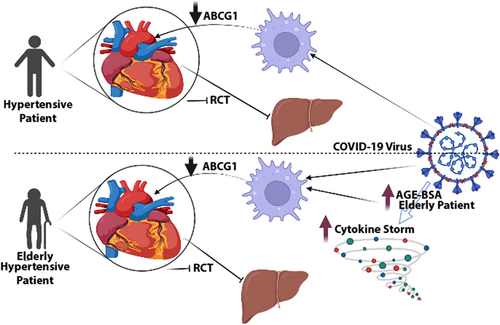
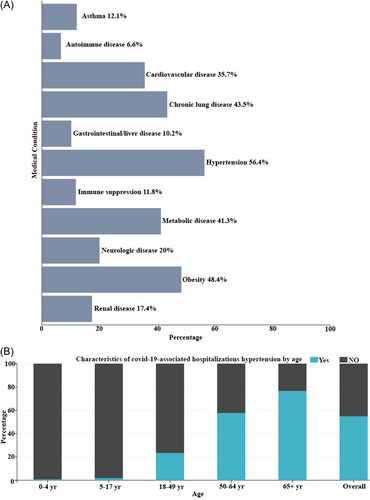
The current worldwide coronavirus sickness outbreak is caused by a new coronavirus structurally connected to the virus that causes severe acute respiratory syndrome (SARS), known as (COVID-19). Indeed, since COVID-19 (SARSCoV2) was discovered in Wuhan, Hubei Province, China in December 2019, healthcare systems throughout the world have faced huge challenges.1 Hypertension, which is common in people all over the world, has been recognized as a key risk factor for higher COVID-19 severity. Patients with COVID-19 who are hypertensive are more likely to get severe pneumonia or organ damage than patients who are not hypertensive. Furthermore, these individuals have increased inflammatory responses and are more likely to die from COVID-19 than those without hypertension.2 Compared to nonhypertensive individuals, COVID-19-positive hypertensive patients had a greater risk of death, hospitalizations, hospital admissions to the intensive care unit, and severe disease/complications. Hence, The COVID-19 pandemic has been a significant stressor and obstacle to efficient chronic illness management, even if there is conflicting information about biological concerns for hypertension therapy throughout the pandemic.3 In addition, a recent study demonstrated that COVID-19 raise systolic and diastolic blood pressure and may cause new-onset hypertension.4 Long-term follow-up of COVID-19 patients reveals a higher prevalence of hypertension and an increase in death following hospital discharge.5 Many gaps in information exist, notably regarding the overall influence of hypertension on SARS-CoV-2 infection and the development of long-term sequelae such as post-COVID syndrome and long-COVID-19.6 Furthermore, given the huge and growing number of COVID-19 patients (about 585 million worldwide), the dangers of the post-COVID syndrome and long-COVID-19 might impact a substantial number of individuals worldwide.1 Here, we would like to shed light on the potential involvement of hypertension in COVID-19 and post-acute COVID-19 syndrome. By utilizing the preliminary hospitalization data of COVID-NET (https://www.cdc.gov/coronavirus/) to evaluate the effect of underlying medical issues on the percentage of hospitalized COVID-19 patients. Data are limited to cases reported between March 1, 2020, and June 30, 2022. This frame sample was done among hospitalized people aged ≥18 years with weighted percentages of persons with underlying medical disorders. According to the findings, hypertension accounts for the largest percentage of COVID-19-related hospitalizations among all medical illnesses (Figure 1A). Following that, our analysis revealed that the percentage of hospitalizations related to hypertension rose with age (65+ years old) as compared to (18–49 years old) and (50–65 years old) (Figure 1B). We recently demonstrated that ATP Binding Cassette Subfamily G Member 1 (ABCG1) depletion in macrophages causes post-acute COVID19 cardiovascular issues due to decreased high density lipoprotein (HDL) and reverse cholesterol transport (RCT) activities.1 In hypertensive individuals, ABCG1 expression in monocytes is decreased, which might be corrected by antihypertensive medication. ABCG1 deficiency is linked to impaired cholesterol efflux from monocyte-derived macrophages.7 In adults with hypertension, plasma Mid-Regional pro-Atrial Natriuretic Peptide (MR-proANP) measures arterial stiffness and hypertension severity.8 According to the findings of a substantial prospective, observational study of patients with COVID-19 infection, higher levels of MR-proANP at admission are associated with the disease severity of COVID-19 and act as a powerful and independent prognostic marker of 28-day mortality.9
On the other hand, ageing is a complicated multifactorial process defined by the accumulation of detrimental alterations in many cells and tissues, resulting in the gradual loss of structural integrity and physiological functioning in diverse organ systems. Macromolecular damage and biochemical alterations may occur as a result of physiological aging and age-related diseases such as diabetes, cataract, Alzheimer's disease, amyloidosis, atherosclerosis, and Parkinson's disease. As a result, the process of macromolecular glycation can be ascribed to ageing and age-related illnesses as a common phenomenon. Several studies have found that the buildup of advanced glycation end product (AGE)-modified macromolecules, whether eaten in meals or increased by inflammation, may hasten the decrease of multisystem function in ageing and so contribute to ageing phenotypes. These research' authors revealed that glycation could change the structure and function of intracellular and extracellular matrix expressions, resulting in tissue stiffness and long-lasting inflammatory response. In this regard, AGE-bovine serum albumin (AGE-BSA) showed both immunosuppressive and inflammatory effects on the human immune system via MAPK-ERK and Myeloid differentiation primary response 88 (MyD88) transduced nuclear factor NF-κappa-B P50 Subunit (NF-κBp50) signaling pathways. The peptide-glucose conjugates' baseline size and the molecules' glycome composition controlled the interlukin-6 (IL-6)-inducing activity of AGE-BSA.10 Microarray and reverse transcription real-time PCR investigations deduced that AGE-BSA exposure lowered ABCG1 messenger RNA levels in human macrophages.11 Besides, AGE-BSA can reduce cholesterol efflux from macrophages to HDL via a liver X receptor-independent mechanism.11 As a result, we may conclude that hypertension is a substantial risk factor for COVID-19 hospitalization due to ABCG1 depletion linked with poor macrophage cholesterol export. Further, older hypertension patients who are also infected with COVID-19 have a greater risk of hospitalization than younger hypertensive patients due to the inflammatory impact of AGE-BSA and the decrease of cholesterol efflux from macrophages. The reduction of RCT activities is responsible for cardiovascular complications in post-acute COVID-19 syndrome (Figure 2). Consequently, under COVID-19 and post-acute COVID-19 syndrome, hypertension remains a critical goal.