Spatiotemporal analysis of the morbidity of global Omicron from November 2021 to February 2022
Abstract
The Omicron variant was first reported to the World Health Organization (WHO) from South Africa on November 24, 2021; this variant is spreading rapidly worldwide. No study has conducted a spatiotemporal analysis of the morbidity of Omicron infection at the country level; hence, to explore the spatial transmission of the Omicron variant among the 220 countries worldwide, we aimed to the analyze its spatial autocorrelation and to conduct a multiple linear regression to investigate the underlying factors associated with the pandemic. This study was an ecological study. Data on the number of confirmed cases were extracted from the WHO website. The spatiotemporal characteristic was described in a thematic map. The Global Moran Index (Moran's I) was used to detect the spatial autocorrelation, while the local indicators of spatial association (LISA) were used to analyze the local spatial correlation characteristics. The joinpoint regression model was used to explore the change in the trend of the Omicron incidence over time. The association between the morbidity of Omicron and influencing factors were analyzed using multiple linear regression. This study was an ecological study. Data on the number of confirmed cases were extracted from the WHO website. The spatiotemporal characteristic was described in a thematic map. The Global Moran Index (Moran's I) was used to detect the spatial autocorrelation, while the LISA were used to analyze the local spatial correlation characteristics. The joinpoint regression model was used to explore the change in the trend of the Omicron incidence over time. The association between the morbidity of Omicron and influencing factors were analyzed using multiple linear regression. The value of Moran's I was positive (Moran's I = 0.061, Z-score = 3.772, p = 0.007), indicating a spatial correlation of the morbidity of Omicron at the country level. From November 26, 2021 to February 26, 2022; the morbidity showed obvious spatial clustering. Hotspot clustering was observed mostly in Europe (locations in High–High category: 24). Coldspot clustering was observed mostly in Africa and Asia (locations in Low−Low category: 32). The result of joinpoint regression showed an increasing trend from December 21, 2021 to January 26, 2022. Results of the multiple linear regression analysis demonstrated that the morbidity of Omicron was strongly positively correlated with income support (coefficient = 1.905, 95% confidence interval [CI]: 1.354–2.456, p < 0.001) and strongly negatively correlated with close public transport (coefficient = −1.591, 95% CI: −2.461 to −0.721, p = 0.001). Omicron outbreaks exhibited spatial clustering at the country level worldwide; the countries with higher disease morbidity could impact the other countries that are surrounded by and close to it. The locations with High–High clustering category, which referred to the countries with higher disease morbidity, were mainly observed in Europe, and its adjoining country also showed high spatial clustering. The morbidity of Omicron increased from December 21, 2021 to January 26, 2022. The higher morbidity of Omicron was associated with the economic and policy interventions implemented; hence, to deal with the epidemic, the prevention and control measures should be strengthened in all aspects.
1 INTRODUCTION
An unknown type of pneumonia broke out in December 2019, which was known as the coronavirus disease 2019 (COVID-19). The International Committee on Classification of Viruses identified the virus as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 Omicron was the SARS-CoV-2 variant (B.1.1.529) that was first reported to the World Health Organization (WHO) from South Africa on November 24, 2021; the WHO regarded B.1.1.529 as a variant of concern (VOC) and designated it as Omicron on November 26, 2021.2 The daily COVID-19 case numbers rapidly increased in South Africa, and it quickly spread in neighboring countries.3 The number of patients with confirmed Omicron infection has significantly increased worldwide. The VOC is spreading rapidly and has crossed many borders worldwide; it is more contagious than the other variants of SARS-CoV-2.4 Therefore, it is important to monitor the spread of the disease systematically, predict new outbreaks early, and identify the temporal and spatial changes of COVID-19 transmission.
Tong et al.5 analyzed the spatiotemporal spread of Omicron in nine provinces in South Africa; they observed that the spatiotemporal spread was relatively slow during the first stage and following the emergence of the Omicron variant in Gauteng; after implementing the prevention and control measures, the transmission of the Omicron infection was controlled. Wang et al. analyzed the COVID-19 confirmed case data, Baidu migration index data, air pollutants, meteorological data, and government response strictness index data using the global and local spatial autocorrelation analysis, spatiotemporal scanning statistics, and Spearman's rank correlation. Results showed that the distribution of COVID-19 cases in China tended to stabilize over time, with spatial correlation and prominent clustering regions; the specific months with high incidence of COVID-19 were January to March, and the area with the highest aggregation risk was Hubei Province.6 Gupta et al. analyzed the spatial autocorrelation, hotspot clustering, and spatial regression in the urban zones of India. Results suggested that the autocorrelation initially increased over time; hotspot clustering was observed in western Maharashtra, eastern Tamil Nadu, Gujarat, and around Kolkata. Urbanization and transit mediums, especially rail and aviation, were positively correlated with higher incidence of infections.7 These scholars not only explored the abovementioned countries and regions, they also analyzed three cities in the United States, Minas Gerais State in southeastern Brazil, and Italy in Europe.8-10
VOC has become a public health threat worldwide; its pathogenic characteristics and the epidemic have caused a public health burden. This study aimed to investigate the global spatiotemporal characteristics and relative influencing factors of the novel Omicron variant of SARS-CoV-2. Although many studies have shown the spatiotemporal distribution of COVID-19, they explored the transmission of COVID-19 in only a few countries, some states, provinces, or urban cities. In this study, the countries worldwide were analyzed, and every country was used as a unit of analysis. The local indicators of spatial association (LISA) clustering map was used for identifying the clustering areas to improve the public health messaging and intervention strategies implemented in these areas. The morbidity of Omicron infection and the influencing factors were analyzed to elucidate the potential factors related to the higher morbidity at the country level. This will help identify the regions that require appropriate intervention strategies.
2 MATERIALS AND METHODS
2.1 Data source
The number of confirmed cases in each country worldwide was obtained from the WHO COVID-19 Dashboard (https://covid19.who.int/info/) on February 26, 2022.11 We filtered the data of confirmed cases from November 26, 2021 to February 26, 2022 since the declaration of the Omicron variant as a VOC by the WHO, which contributed to the rapid increase in the number of COVID cases. The population of each country, territory, and area were downloaded from the United Nations website (https://population.un.org/wpp/). Data on the responses policy were collected from the Our World in Data website.12
The cartographic base of the country, territory, and area was obtained from GADM website (http://www.gadm.org/), including the longitude and latitude of 220 countries, territories, and areas. In the following, we were uniformly called country, territory and area as location.
2.2 Statistical analyses
2.2.1 Handling of missing values and multiple linear regression analysis
Multiple linear regression was performed to explore the factors that influence the morbidity of Omicron, control the confounding factors, and evaluate the independent effects of multiple independent variables on dependent variables. The multiple imputation method was used to handle the missing values in the data, which were included in the multiple linear regression analysis using STATA (version 16.1). The status of missing values are shown in Table 1. At first, the missing data were set as an mi data set, and then their attributes were modified to determine which variables contain missing values and which of them contain complete values. Then, 10 imputations were created for each missing value, producing 10 copies of the data set, each of which had missing values imputed using “switching regression,” an iterative multivariable regression technique. Each data set had missing values suitably imputed, and each complete data set was analyzed independently using the regression model. Estimates of the parameters of interest were averaged across the 10 copies to provide a single estimate based on the Rubin's rule.13, 14
| Variablesa | Range of values | Missing value (n) | N | Percentage |
|---|---|---|---|---|
| Stringency index | 2.78–93.52 | 7270 | 23 047 | 31.54 |
| Containment index | 14.29–84.52 | 7270 | 23 047 | 31.54 |
| Restriction gatherings | 0–4 | 7255 | 23 047 | 31.48 |
| Facial coverings | 0–4 | 7266 | 23 047 | 31.53 |
| Cancel public events | 0–2 | 7243 | 23 047 | 31.43 |
| Workplace closures | 0–3 | 7243 | 23 047 | 31.43 |
| Testing policy | 0–3 | 7303 | 23 047 | 31.69 |
| Contact tracing | 0–2 | 7268 | 23 047 | 31.54 |
| School closures | 0–3 | 7231 | 23 047 | 31.38 |
| Stay home requirements | 0–3 | 7267 | 23 047 | 31.53 |
| Income support | 0–2 | 7281 | 23 047 | 31.59 |
| Debt relief | 0–2 | 7303 | 23 047 | 31.69 |
| Public information campaigns | 0–2 | 7282 | 23 047 | 31.60 |
| Restrictions internal movements | 0–2 | 7261 | 23 047 | 31.51 |
| Vaccination policy | 0–5 | 7268 | 23 047 | 31.54 |
| Close public transport | 0–2 | 7238 | 23 047 | 31.41 |
| International travel controls | 0–4 | 7270 | 23 047 | 31.54 |
- Abbreviations: n, number of missing values; N, total number of observation.
- a Stringency index and containment index were assigned as continuous variables, while the other variables were assigned as ordinal variables.
2.3 Spatial analysis
In this ecological study, an exploratory analysis of the global spatial and temporal distribution of Omicron cases from November 26, 2021 to February 26, 2022 was conducted. The country was adopted as units of analysis, and the distribution of cases by area was evaluated. The database of cases contained information from 237 locations. The data of 17 locations did not match the geographical database. A total of 220 locations were analyzed, and 32 locations were defined as missing values.
Morbidity was used to depict the influence of Omicron infection in healthy people, which was calculated as the total number of cases in each period divided by the population then multiplied by 10 000. The distribution of morbidity in each country was determined using the QGIS software (version 3.16.4) to present the cartographic data and construct the thematic maps.
Spatial autocorrelation analysis was conducted using the GeoDa software (version 1.18.0; GeoDa Center). To assess for spatial clustering of Omicron cases at the country level, an inverse distance contiguity matrix was created. The distance was measured using Euclidean distance and was expressed in degrees. The threshold value was 31.865, which is the minimum value to indicate the absence of neighborless observations (isolates).
To analyze the spatial autocorrelation, the values of the Global Moran Index (Moran's I) and LISA were calculated. Moran's I was used to measure the relationship between the same attributes of adjacent spatial units, with the values ranging from −1 to 1. Positive values indicate a positive spatial correlation; that is, the closer their spatial positions, more similar their attributes. A negative value indicates a negative spatial correlation, the nearer the spatial locations, the more different their attributes. Values that are close to 1 indicate a stronger spatial autocorrelation. A value of 0 indicates the absence of a spatial autocorrelation.15, 16 LISA was used to assess the influence of individual locations on the magnitude of the global statistic and to identify the “outliers.” The spatial patterns in the LISA cluster map were divided into five categories: High–High (hotspot), Low–Low (coldspot), Low–High, High–Low, and Not Significant. The High–High and Low–Low locations indicated spatial clustering of similar values, that is, high values (or low values) surrounded by high (or low) neighboring values. Both High–High and Low–Low locations denoted a positive spatial autocorrelation, implying a spatial homogeneity. The Low–High and High–Low locations were regarded as spatial outliers, indicating a spatial association of dissimilar values. Low–High was defined as low values surrounded by high neighboring values, while High–Low was defined as high values surrounded by low values. Low–High and High–Low represent a negative spatial autocorrelation, thus implying a spatial heterogeneity.16, 17
2.4 Temporal analysis
Joinpoint regression model was used to divided a long-term trend line into segments, and each segment was described with continuous linearity. Linear models can only describe or predict one trend, and time series models also have several limitations. By contrast, the joinpoint regression model was a better choice for determining the trend of disease. It was used to calculate the daily percent change (DPC) to characterize the trends in disease rates over time; the rates were assumed to change at a constant percentage of the rate of the previous day. In recent years, more and more researchers have conducted analyses to determine the trend of the COVID-19 outbreak.18 The global-level morbidity was calculated by dividing the total number of cases every day in all 220 locations by the population in all 220 locations then multiplying the quotient by one million. Then, the data were imported into the Joinpoint Regression Program 4.9.1.0 (https://surveillance.cancer.gov/joinpoint/, accessed on June 26, 2022), with the crude rate as dependent variable and the independent variable as daily number of cases. Assignment 0–92 corresponded to the date from November 26, 2021 to February 26, 2022 and the option of log-transformed was selected Yes. The rest option was in default (Grid Search method and Monte Carlo mutation test for joinpoint analysis, estimating the parameter and selected model).
3 RESULTS
3.1 Spatial and temporal distribution
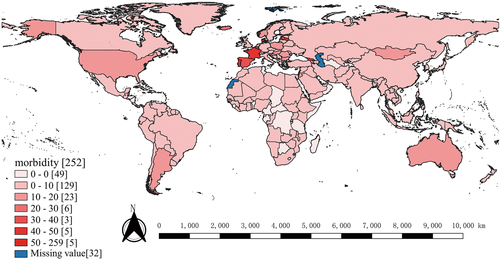
The morbidity of COVID-19 was classified into the following categories: 0–0, 0–10, 10–20, 20–30, 30–40, 40–50, and 50–259 (per 10 000 people) and missing value.
Figure 1 shows the distribution of morbidity from November 26, 2021 to February 26, 2022; in Europe, 129 locations were in the 0–10 category, while 5 were in the 50–259 category. The morbidity rate in these locations was analyzed, and results showed that Faroe Islands had the highest morbidity, followed by Réunion, Guam, Latvia and Israel (258.887, 181.568, 91.838, 56.765, and 54.799, respectively). Meanwhile, 49 locations, in Africa were in the 0–0 category, while 23 locations from different continents were in the 10–20 category. A total of 6, 3, and 5 locations were under the 20–30, 30–40, and 40–50 categories, respectively.
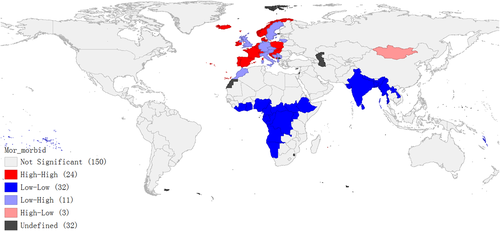
3.2 Spatial autocorrelation
The Moran's I was positive (Moran's I = 0.061, Z-score = 3.772, p = 0.007) during the period, indicating a persistent positive spatial correlation and a spatial clustering in majority of the Omicron cases in each location, not randomly distributed. The closer the value of Moran's I to 1 or −1, the stronger the spatial autocorrelation. Geography could influence the transmission of Omicron; the morbidity in each location was correlated with the geospatial location of the adjacent country.
Figure 2 shows the LISA cluster map of morbidity. Hotspot clustering was relatively high in the western European countries, and a total of 24 countries were categorized as High–High. The Faroe Islands ranked first in terms of morbidity (High–High category); its trend of new cases swiftly increased since the emergence of the Omicron variant. This finding suggested that the Omicron variant is strongly contagious. The Low–Low category was mainly observed in southern Africa and some locations in Asia (total locations: 32). The Low–High and High–Low categories were observed in Europe and Asia (11 and 3, respectively). The corresponding categories of all mentioned locations are shown in Table 2.
| High–High | Low–Low | Low–High | High–Low |
|---|---|---|---|
| Andorra | Angola | Albania | Mongolia |
| Belgium | American Samoa | Austria | Sint Maarten |
| Switzerland | Bangladesh | Bosnia and Herzegovina | Réunion |
| Denmark | Central African Republic | Czechia | |
| Spain | Ivory Coast | Germany | |
| France | Cameroon | The United Kingdom | |
| Faroe Islands | Democratic Republic of the Congo | Italy | |
| Gibraltar | Congo | Lithuania | |
| Croatia | Cook Islands | Morocco | |
| Hungary | Ethiopia | Serbia | |
| Isle of Man | Gabon | Sweden | |
| Ireland | Ghana | ||
| Iceland | Equatorial Guinea | ||
| Liechtenstein | India | ||
| Luxembourg | Lao People's Democratic Republic | ||
| Monaco | Liberia | ||
| Montenegro | Sri Lanka | ||
| Netherlands | Myanmar | ||
| Norway | Namibia | ||
| Poland | Nigeria | ||
| Portugal | Niue | ||
| San Marino | Nepal | ||
| Slovakia | French Polynesia | ||
| Slovenia | Rwanda | ||
| South Sudan | |||
| Togo | |||
| Tokelau | |||
| Tonga | |||
| Uganda | |||
| Vanuatu | |||
| Wallis and Futuna | |||
| Samoa |
- Abbreviation: LISA, local indicators of spatial association.
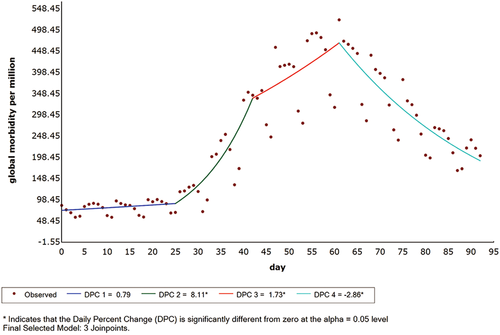
3.3 Changes in the trend of Omicron outbreak
Figure 3 shows the changes in the trend of the Omicron cases; then, the number of cases in the two periods has eventually declined (Figure 3). From November 26, 2021 to December 21, 2021, the morbidity of Omicron showed a nonsignificant DPC of +0.8% (95% confidence interval [CI]: −1.0 to 2.6, p = 0.386), followed by a daily significant increase of +8.1% (95% CI: 5.6–10.7, p < 0.001) from December 21, 2021 to January 7, 2022, a DPC of +1.7% (95% CI: 0.3–3.1, p = 0.015) from January 7, 2022 to January 26, 2022, and a significant decrease of −2.9% (95% CI: −3.5 to −2.2, p < 0.001) from January 26, 2022 to February 26, 2022 (Table 3). The global morbidity reached the peak on January 26, 2022, which corresponds to the DPC three period.
| Date | DPC (95% CI) | t | p |
|---|---|---|---|
| World | |||
| 2021/11/26–2021/12/21 | 0.8 (−1.0 to 2.6) | 0.9 | 0.386 |
| 2021/12/21–2022/1/7 | 8.1 (5.6–10.7) | 6.6 | <0.001 |
| 2022/1/7–2022/1/26 | 1.7 (0.3–3.1) | 2.5 | 0.015 |
| 2022/1/26–2022/02/26 | −2.9 (−3.5 to −2.2) | −8.6 | <0.001 |
- Abbreviations: CI, confidence interval; DPC, daily percent change.
3.4 Multiple linear regression
Results of the multiple linear regression analysis showed that close public transport was strongly negatively correlated with the morbidity of Omicron, followed by facial coverings, stay home requirements, cancel public events, restrictions internal movements, international travel controls, school closures, testing policy, and debt relief. The morbidity was positively associated with income support, workplace closures, and containment index (Table 4).
| Variables | Coefficient | SE | t | p | 95% CI |
|---|---|---|---|---|---|
| Stringency index | −0.053 | 0.088 | −0.61 | 0.547 | −0.231 to 0.124 |
| Containment index | 0.358 | 0.100 | 3.57 | 0.001 | 0.155–0.561 |
| Restriction gatherings | −0.149 | 0.207 | −0.72 | 0.474 | −0.558 to 0.261 |
| Facial coverings | −1.571 | 0.293 | −5.36 | <0.001 | −2.168 to −0.974 |
| Cancel public events | −1.275 | 0.512 | −2.49 | 0.016 | −2.300 to −0.250 |
| Workplace closures | 1.050 | 0.410 | 2.56 | 0.016 | 0.209 to 1.890 |
| Testing policy | −0.825 | 0.329 | −2.51 | 0.014 | −1.478 to −0.171 |
| Contact tracing | −0.243 | 0.518 | −0.47 | 0.643 | −1.301 to 0.815 |
| School closures | −0.883 | 0.302 | −2.92 | 0.006 | −1.493 to −0.273 |
| Stay home requirements | −1.485 | 0.404 | −3.68 | 0.001 | −2.321 to −0.649 |
| Income support | 1.905 | 0.278 | 6.85 | <0.001 | 1.354–2.456 |
| Debt relief | −0.633 | 0.246 | −2.57 | 0.012 | −1.124 to −0.143 |
| Public information campaigns | 0.077 | 0.791 | 0.10 | 0.923 | −1.533 to 1.688 |
| Restrictions internal movements | −1.271 | 0.406 | −3.13 | 0.004 | −2.104 to −0.438 |
| Vaccination policy | 0.354 | 0.284 | 1.25 | 0.219 | −0.219 to 0.928 |
| Close public transport | −1.591 | 0.435 | −3.65 | 0.001 | −2.461 to −0.721 |
| International travel controls | −0.988 | 0.285 | −3.47 | 0.002 | −1.568 to −0.408 |
- Abbreviations: CI, confidence interval; SE, standard error.
4 DISCUSSION
As reported in the WHO COVID-19 Dashboard (https://covid19.who.int/info/) on February 26, 2022, COVID-19 quickly spread worldwide since the emergence of the Omicron variant. This study investigated the association between the novel Omicron variant and its influencing factors by conducting a spatiotemporal analysis.
We noted that the morbidity of daily new confirmed cases was negatively correlated with close public transport, facial coverings, stay home requirements, cancel public events, restrictions internal movements, international travel controls, school closures, testing policy, and debt relief. The more enhanced the level of these responses policy, the lower the morbidity. Fowler et al.19 elucidated that stay-at-home orders might have reduced the number of confirmed cases in the United States. Another study also showed a similar result, when the first COVID-19 case was reported in Wuhan, China and resulted in a higher morbidity, due to population mobility, which was partially explained by the intracity movement of the people who provided public services to fight the epidemic.20 Thus, strengthening the preventive measures such as implementation of stay at home requirements, closure of public transports, international travel controls, school closures, and cancellation of public events can reduce the morbidity.
Positive correlations were observed between Omicron morbidity and income support, workplace closures, and containment index. Feng et al.21 found that the number of confirmed cases was positively correlated with gross domestic product in LiaoNing and Jilin, China. Marcos César Ferreira also found that the population most vulnerable to COVID-19 were those living in the districts with lower salaries and slum areas in the São Paulo municipality, Brazil.19 Madden et al.22 found a similar result in Ireland; that is, the higher the deprivation index and the larger the population density, the higher the morbidity. However, the stay at home index (an indicator of population mobility) was negatively associated with morbidity. Another study showed that the most deprived areas, the region with the lowest employment rate, and higher housing density were associated with higher morbidity.23
From November 26, 2021 to December 21, 2021, since the emergence of the Omicron variant, the morbidity rate increased slowly. From December 21, 2021 to January 26, 2022, it swiftly reached the peak in just 1 month, demonstrating that the Omicron variant spread rapidly within a short period of time. Desingu et al.24 also found a similar trend in three regions (South Africa, Europe, and North America) from November 29, 2021 to January 3, 2022. It may be caused by mutations in the spike (S) protein receptor-binding domain; thus, the Omicron variant was considered to be significantly more infectious.25 Finally, it showed a decreasing incidence, suggesting that the response policy and preventive measures implemented worldwide since January 26, 2022 were effective. The graph of the joinpoint regression analysis showed that morbidity changed within 7 days, suggesting that the transmission pattern of Omicron was based on a 7-day cycle.
Our analysis demonstrated a spatial autocorrelation worldwide; the risk of Omicron infection differed significantly, and spatial clustering varied greatly across continents. The global morbidity of Omicron showed spatiotemporal clustering patterns from November 26, 2021 to February 26, 2022 as reported in our study. The finding demonstrated that Europe was the continent that possessed the most number of locations under High–High category, and most of the locations showing spatial clustering were observed in western countries of Europe.
Chu et al.26 analyzed the cross-country COVID-19 pandemic in Europe; results showed the highest level of connectedness among European countries, reflecting the severe outbreak of COVID-19, in late March and early April 2020, and the first wave of the pandemic subsided in May 2020. Shariati et al. conducted a hotspot analysis and a spatial autocorrelation analysis of the cumulative incidence rate in all countries at the end of March and April 2020. Results demonstrated High-High clusters in the southern, northern, and western Europe.27
The LISA cluster map showed that Africa and Asia had Low–Low clusters; some countries with low morbidity were also surround by countries with low morbidity. The probable cause of this phenomenon is that these countries implemented effective prevention and control measures. Rampal et al. collected country-specific policy documents, official government media statements, mainstream news portals, global statistics databases, and the latest published literature available from January to October 2020, and analyzed the situational and epidemiological trend of six South-East Asian countries (Malaysia, Singapore, Thailand, Philippines, Indonesia, and Myanmar). Results showed that the primary strategies for preventing virus transmission were observing good hygiene practices, maintaining social distancing, implementation appropriate airborne precautions, contact tracing, early detection, and isolation.28 The countries under the Hotspot category should implement these measures to strictly control the spread of the disease.
This study showed the spatial distribution of the morbidity of Omicron and the morbidity rate in every location worldwide. The disease became more and more serious over time; not only one country was influenced by the disease, but other countries surrounded by those with high morbidity were also affected. Salehi et al.29 developed a useful online interactive dashboard (https://mahdisalehi.shinyapps.io/Covid19Dashboard/) that visualize and follow the confirmed cases of COVID-19 in real-time; the dashboard showed that the number of confirmed cases and deaths due to COVID-19 were remained high. The highest risk was observed in Europe; in Asia, the morbidity was reportedly low.
Although many scholars have investigated the aforementioned factors related to the morbidity of COVID-19, either they analyzed the question locally or they did not cope with this topic from a geospatial perspective. Our study collected data from various countries worldwide to explore the association between Omicron response policies and morbidity of Omicron; furthermore, the study investigated the morbidity pattern from November 26, 2021 to February 26, 2022.
This study has some limitations. Morbidity was analyzed based on the reported COVID-19 cases by the WHO. There were delays in data reporting, and data on the influencing variables had missing values; hence, we adopted multiple interpolation methods to address this issue. However, it may also cause deviations in the results.
5 CONCLUSION
According to the country level distribution of Omicron from November 26, 2021 to February 26, 2022, the morbidity observed in the different locations worldwide was a clear situation; Europe was most impacted, followed by North America, South America, Oceania, Asia, and Africa. Hence, stricter prevention and control measures should be implemented.
The morbidity gradually increased, and the difference was not statistically significant in the first month since the emergence of the Omicron variant. The morbidity rapidly increased from December 21, 2021 to January 26, 2022, with the Omicron infection spreading quickly worldwide during this period. After taking effective measures, the morbidity started to decrease in January 26, 2022.
The result of Moran's I showed that morbidity had a positive spatial correlation at the country level during the period, thus suggesting the clustering of morbidity worldwide. The disease could transmit among the locations, and the morbidity in each location could impact the surrounding locations. Therefore, the epidemic should not only be managed by one country. Others, especially the surrounding countries, should also be provided with assistance.
The LISA cluster map showed a strong clustering of Omicron incidence in Europe and a Low–Low category in Africa. Outlier, Low–High, and High–Low categories were most observed in the countries in Europe, while the Not Significant category mostly observed in the countries in North America Oceania, and Asia.
The morbidity of Omicron is was strongly negatively correlated with variable close public transport and strongly positively correlated with income support; this finding may indicate that the economic and policy interventions have a significant impact on morbidity. We should pay more attention to the relative prevention measures for preventing and controlling the transmission of disease. To better cope with the spread of disease, we should not ignore the spatiotemporal characteristics of the disease.
AUTHOR CONTRIBUTIONS
Yuelang Liang conceptualized, designed methodology, did a formal analysis, and wrote the original draft. Zijun Gong scrubbed data and maintained research data. Jiajia Guo and Qi Cheng collected literature and visualized the data. Zhenjiang Yao reviewed and revised the article, obtained the funding, and supervised this study. All authors read and approved the final manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
The article did not involve human participants or animal samples, and the data used in this study were open data collected from the network or official report. Therefore, ethical approval was not necessary for this study.
Open Research
DATA AVAILABILITY STATEMENT
The data sets were collected from the World Health Organization Coronavirus Dashboard (https://covid19.who.int/info/), the United Nations (https://population.un.org/wpp/), the Our World in Data website, and the GADM website (http://www.gadm.org/). The data sets used and analyzed during the study are available from the corresponding author on reasonable request. Research data are not shared.