Prevalence of EBV, CMV, and HPV in oral squamous cell carcinoma patients in the Pakistani population
Abstract
Many studies have proposed an important role of viruses in the pathogenesis of oral cancer. The present study aimed to find out the prevalence of Epstein-Barr virus (EBV), cytomegalovirus (CMV), and human papillomavirus (HPV) among patients with oral squamous cell carcinoma (OSCC) in a Pakistani cohort. We investigated tissue samples obtained from 58 patients with OSCC using the polymerase chain reaction assay. No sample was positive for HPV. EBV was identified in 15 patients (25.86%), and CMV in three patients (5.17%). Coinfection with one or more viruses was detected in two cases and was coinfection with EBV and CMV. These results suggest a low prevalence of these viruses in OSCC patients in the Pakistani population compared to most other countries where the prevalence of these viruses has been reported in the past. Nevertheless, further studies are necessary to determine the potential role of EBV and the possible importance of CMV as an infection cofactor in oral cancer.
1 INTRODUCTION
Head and neck cancer ranks sixth among the most common malignant tumors worldwide and is one of the major problems of public health worldwide.1 There are several types of cancers of the oral cavity, but approximately 90% are squamous cell carcinomas. Many different risk factors play their roles in the etiology of oral cancer. The effect of some etiological factors is well-established in the literature, such as consumption of tobacco and alcohol, poor oral hygiene and inappropriate dietary habits.2, 3
The role of oncogenic viruses in the development of oral squamous cell carcinoma (OSCC) has been proposed previously.4-6 It is known that human papillomaviruses (HPV) do play an important role in a subset of head and neck squamous cell carcinoma (HNSCC).7 Currently, 20% to 30% of patients with OSCC do not have the traditional risk factors of smoking and alcohol use and HPV appears as the major driver of malignant transformation.8 The Epstein-Barr virus (EBV) has long been related to nasopharyngeal carcinoma. A recent meta-analysis showed a significant association between EBV and OSCCs 9 though there are studies not reporting a significant association.10 Some members of the Herpesviridae family (EBV and HHV-8) are also recognized as carcinogens. Other herpesviruses such as cytomegalovirus (CMV) and HHV-6 and -7 may be associated with a malignant phenotype, but their carcinogenic role remains unclear.11 Persistent infection with EBV has been linked to the development of malignancies including HPV-associated oral carcinoma. However, the possible role of EBV and other herpesviruses in HPV-associated oral cancers is still poorly understood. With different viruses associated with HNSCC, it is important to find out their prevalence in the Pakistani cohort of OSCC. The present study aimed to find out the frequencies of EBV, CMV, and HPV infection among patients with OSCC in the Pakistani population.
2 MATERIALS AND METHODS
The present study comprised a group of 58 patients with a diagnosed and histopathologically-confirmed OSCC who were hospitalized at the Dow University Hospital, Karachi during January 2015 to December 2017. The patients had neither previous radiotherapy nor chemotherapy. This research was approved by the Ethics Committee and is per the GCP regulations. Informed consent was obtained from each patient before enrolling them in this study. Five- to six-micron sections of formalin-fixed, paraffin-embedded (FFPE) tissues were used for the extraction of DNA by using QiaAmp FFPE tissue kit (QIAGEN, Germany) as per manufacturer's instruction. A total of 10 μL DNA was used to detect the EBV infection by amplifying the Bam HI W region of the EBV genome by nested PCR.12 While the HPV-L1 gene fragment was amplified by PCR for the detection of HPV infection.13 CMV was detected in real-time PCR assay by using the commercially available Artus CMV RG PCR Kit (QIAGEN). Statistical analyses were performed by tabulating the data in Microsoft Excel 365.
3 RESULTS
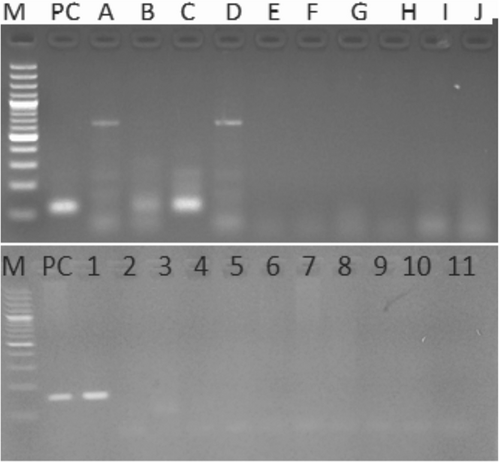
The study included 58 patients with OSCC. The mean age of the patients was 42 years (standard deviation: ±12 years) ranging from 26 to 70 years. Males were 82% and females were 18%. All cases resulted in negative for HPV. CMV was detected in only three cases (5.17%) while 15 cases (25.86%) were positive for EBV (Figure 1). Of the 58 cases, 24 (41.37%) were localized to buccal cavity, 17 (29.3%) to tongue, 11 (18.96%) to lips, and 6 (10.34%) to the palate (Table 1).
| Total | HPV | CMV | EBV | |
|---|---|---|---|---|
| OSCC | 58 | 0 | 3 (5.17%) | 15 (25.86%) |
| Buccal cavity | 24 (41.37%) | 0 | 2 (8.33%) | 10 (41.66%) |
| Tongue | 17 (29.3%) | 0 | 1 (5.55%) | 4 (23.52%) |
| Lip | 11 (18.96%) | 0 | 1 (9.09%) | 0 |
| Palate | 6 (10.34%) | 0 | 0 | 0 |
- Abbreviations: CMV, cytomegalovirus; EBV, Epstein-Barr virus; HPV, human papillomavirus; OSCC, oral squamous cell carcinoma.
In patients with OSCC localized to buccal cavity, only 2 (8.33%) were positive for CMV and 10 (41.66%) were positive for EBV while no one was positive for HPV (Table 1). Of the 17 cases affecting the tongue, only 1 (5.55%) was positive for CMV and 4 (23.52%) were detected positive for EBV while no HPV positive case was detected. In OSCC patients in which lesions were localized to lips, no one was detected positive for HPV and EBV while only 1 (9.09%) was positive for CMV. In six cases in which lesions were localized to the palate, none of the patients were tested positive for HPV, EBV, and CMV.
4 DISCUSSION
We explored the prevalence of HPV and other potentially oncogenic viruses in OSCC cases from different anatomic sites. This is the first study from Pakistan reporting on the HPV, CMV, and EBV infections in oral cancers. HPV infection is considered a sexually-transmitted infection, while EBV is mostly transmitted through saliva.14 Both agents are capable of establishing long-term infection in epithelial cells. A variety of stimuli do play a role in activating viral genome expression.14 Chemicals and sexual behaviors can play a role. In our investigation, HPV was absent in our patients of OSCC compared to the reported global prevalence in the same types of cancer (6% in Yemen to 65% in Sudan for OSCC).15 High HPV prevalence is also reported from the region, that is, 30% in Sri Lanka to 45% in India.15 In a recent study conducted in Italy, the frequency of HPV was 19.6% in OSCC patients, while the coinfection of EBV and HPV was found at 7.84%.16
In a Polish OSCC cohort, HPV was positive in 28.1% patients while EBV and HPV coinfection was found in 34.14% patients.17 In another study from Poland, HPV was detected in 32.5% OSCC patients and coinfection with EBV was found in 30%.18 In a recent investigation, an HPV prevalence of 14.5% was reported in an OPSCC cohort from Thailand.19 The fact that no OSCC patient in our population tested positive for HPV, suggests little or no role of this virus in OSCC patients in the Pakistani population. Our findings are also corroborated by an Indian investigation, which found that none of the samples were HPV positive in a cohort of 60 OSCC patients. This study also suggests that the association between HPV and OSCC may be overestimated, especially in subcontinent populations.20
In our study, the highest overall virus prevalence was EBV, which was seen at 25.86% of the OSCCs. Comparing to the rest of the world, EBV prevalence in OSCC patients in our population was low. Around the world, there is a huge variation in EBV prevalence in OSCC, ranging from 22% in Yemen to 80% in the UK, with a statistically significant higher EBV prevalence in the industrialized countries compared to the developing countries.15 This is comparable to earlier studies performed in Sweden, Sudan, and India regarding EBV prevalence in OSCC.21-23 In a study on immigrants in Sweden, Mousavi et al24 concluded that “early life infection with EBV in the immigrant's countries of origin, and probably a minor contribution by smoking, maybe the main exposures influencing nasopharyngeal carcinoma risks among immigrants to Sweden. In a study conducted in Italy, the frequency of EBV was 50.9% while the coinfection of EBV and HPV was found at 7.84%.16 In a Polish OSCC cohort, EBV was positive in 54.7% of patients while EBV and HPV coinfection was found in 34.14% patients.17 In another study from Poland, EBV was identified in 57.5% of patients. Coinfection with one or more viruses was detected in 30% of cases and most frequently it was coinfection with EBV and HPV (15%).18
In the present study, the prevalence of CMV in the OSCC was 5.17%. The overall prevalence of CMV in patients with OSCC lesions in different countries of the world have been reported from 0 to 91.5%.25, 26 The CMV in our study was slightly less prevalent than in the Southeast of Iran (6.3%) but more prevalent than the Northeast Khorasan region.26 This difference, however, could be owing to the population under study because Delavarian et al26 investigated OSCC patients younger than 40 years while in our patient population, the mean age of the patients was above 42. Wei et al25 also reported a higher prevalence of CMV in OSCC than normal oral tissues. In another study from Poland, CMV was found in 10% of OSCC patients.18 One property of herpesviruses is diversity incidence in different geographic areas. Hence, a variety of genetic, environmental, or viral factors can clarify this regional difference.
Taken together, the results of our study confirm the low prevalence of HPV, CMV, and even EBV in OSCC patients in Pakistan. The reasons for this low prevalence in the Pakistani cohort are not clear but may be related to differences in the genetic architecture of the South Asian population. Another plausible reason may be a substantially different level of exposure of our population to various environmental toxicants. The lack of literature in this context from Pakistan necessitates the importance of further research in this field. Therefore, further studies are required to determine the exact frequency and potential role of these viruses using case-control studies. Possible associations with tobacco and alcohol use and exploring genetic differences in cytochrome P450 genes may hold a clue. It is also important to investigate the possible importance of CMV as an infection cofactor in OSCC.
ACKNOWLEDGMENTS
The authors wish to thank Dow University of Health Sciences, Karachi, and Shifa Tameer-e-Millat University, Islamabad for providing an excellent academic environment to facilitate these kinds of scholarly activities. Funding for this research project was provided by the Dow University of Health Sciences, Karachi, and Shifa Tameer-e-Millat University, Islamabad, Pakistan.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
SA and SK conceptualized the study. SUN, AA, and SG searched the literature, collected the data, and helped in manuscript preparation. AL, SA, and SG helped prepare the manuscript. SA, SK, and SG refined the manuscript for publication. All authors read and approved the final manuscript for publication.




