Is human cytomegalovirus infection associated with essential hypertension? A meta-analysis of 11,878 participants
Abstract
Human cytomegalovirus (HCMV) has been reported to be highly expressed in essential hypertension (EH), and it has been proposed that HCMV infection may contribute to EH development. However, different studies showed opposite results. The present meta-analysis was performed to investigate the association between HCMV infection and the risk of EH. All relevant literature from 1980 to 2015 was extracted from six electronic databases. Odds ratios (OR) and 95% confidence intervals (CI) were used to assess the strength of the association of HCMV infection and risk of EH. Sensitivity analysis and examination for bias were conducted to evaluate cumulative evidence of the association. The random-effect model using the Mantel–Haenszel method was used to give the individual effect-size estimates. Of the 11,878 participants included in this study, there were 3,864 EH patients and 8,014 control subjects. Meta-analysis of nine studies performed in a random-effect model found that EH patients had a higher risk of HCMV infection than normal control subjects (OR = 1.47, 95%CI: 1.13–1.90, P = 0.004; heterogeneity: I2 = 66%, P = 0.002). Sensitivity analysis and bias examination showed the overall quality and consistency of the studies to be acceptable. For subgroup analysis, studies of Chinese populations were selected for further analysis. There was a significant association between HCMV infection and EH among Chinese patients (OR = 2.18, 95%CI:1.43–3.31, P = 0.0003) but not among other ethnic groups (OR = 1.11, 95%CI:0.95–1.31, P = 0.19). These findings provide quantitative support for the association between HCMV infection and high risk of EH in individuals of Chinese ethnicity. J. Med. Virol. 88:852–858, 2016. © 2015 Wiley Periodicals, Inc.
INTRODUCTION
Essential hypertension (EH) is one of the most important cardiovascular diseases affecting humans. At least 20% of Chinese adults are estimated to suffer from EH, with millions of patients dying or becoming disabled every year [Ma et al., 2012]. Similar phenomena have been observed in the U.S. and other Western countries [Lackland, 2013]. The etiology of EH has been investigated in many countries for many years and in many ways. Unfortunately, the major etiologies of EH fall into two broad categories: environmental factors and genetic factors. Although a four-dimensional model has been put forward for the pathogenesis of EH [Wang, 2012], the specific etiologies of EH remain unclear.
Human cytomegalovirus (HCMV) is a member of the beta-herpes virus subfamily. It is a ubiquitous pathogen that infects only humans. Some 50–70% of adults are infected with HCMV, most of them asymptomatically [Huang et al., 2013]. In contrast, immunosuppressed or immunocompromised patients, such as transplant recipients and patients with HIV, commonly experience clinically significant HCMV infections [Harvala et al., 2013; Fowotade et al., 2015]. Clinically, HCMV can cause congenital diseases, pneumonitis, retinitis, and gastroenteritis [Shaaban et al., 1995; Pathanapitoon et al., 2009; Snyder et al., 2010; Maher and Nassar 2013]. Some studies have identified associations between HCMV and coronary heart diseases and atherosclerosis [Horváth et al., 2000; Boeckh and Geballe 2011; Ji et al., 2012]. In 2011, Zhang et al. proposed that HCMV infection may be a novel etiology for EH [Zhang et al., 2011]. Recently, some researchers have reported that HCMV is highly expressed in EH patients [Haarala et al., 2012; Vahdat et al., 2013], but others recorded conflicting results [Fagerberg et al., 1999; Li et al., 2012]. For these reasons, the true relationship between EH and HCMV infection has remained unclear and controversial.
The purpose of the present study was to use meta-analysis of the available evidence from population-based studies of the relationship between EH and HCMV to better assess the possibility that HCMV infection might play an etiological role in EH.
METHODS
Data Sources and Searches
To search for all the studies that investigated the association of HCMV infection and EH in different ethnic groups, we conducted a computerized literature search. All literature from January 1, 1980 to January 8, 2015 was selected from the following databases: the China Nation Knowledge Infrastructure Platform (CNKI), Wanfang database, China Biological Medicine Database (CBM), PubMed, EMBASE, Cochrane Library, Medline, Google Scholar, and reference lists of related articles. “Cytomegalovirus” and “hypertension” and “human cytomegalovirus” and “hypertension” were used as search keywords and subject terms. Only studies published in Chinese or English were included. The references of retrieved articles were also screened. To prevent data duplication, when a report overlapped with another publication, only the more detailed one was kept [Xu et al., 2013].
Studies Selection
The following inclusion criteria were used for the meta-analysis: (i) studies investigating the association of HCMV and hypertension in patients with essential hypertension that included normotensive subjects; (ii) studies of unrelated case-controls (family-based studies were excluded) or cohort studies; (iii) HCMV infection was defined as serologic evidence of HCMV infection (seropositivity for anti-CMV IgG or anti-CMV IgA) and clinical diagnosis as an HCMV-infected or HCMV carrier; (iv) EH was defined as systolic blood pressure (SBP) ≥140 mmHg, and/or diastolic blood pressure (DBP) ≥90 mmHg, and/or treated with anti-hypertensive medicine, and clinical diagnosis as EH patients [Majernick and Madden, 2003]; (v) sufficient information to allow adequate estimation of odds ratios (OR) and 95% confidence interval (CI) of the risk of HCMV infection in patients with essential hypertension and in normotensive subjects. Exclusion criteria included the following: (i) animal or cell studies involving CMV and hypertension; (ii) participants included patients with pre-eclampsia, or healthy pregnant women; (iii) studies with overlapping data.
Data Extraction
Two authors independently reviewed and extracted the data. Disagreements were resolved through discussion among the authors to achieve a consensus. The following information was abstracted from each study: first author, year of publication, ethnic background and resident region of studied population, diagnostic criteria, patient characteristics matched (age, gender, body mass index, etc.), source of samples, method(s) of HCMV detection, number of cases and controls, and number of HCMV-seropositive subjects among both essential hypertensive, and control participants [Gu et al., 2011].
Assessment of Study Methods and the Risk of Bias
The Newcastle–Ottawa quality assessment scale (NOS) was used to assess the quality of the methodology in the included studies. A star system was used to judge the data according to the study populations, comparability of groups, and exposure or outcome of interest. The NOS scale consists of eight questions with nine possible points. The assessment score ranged from 0 to 9. Studies with a total score of six or lower were considered to be of low quality and to have a high risk of bias, and studies with scores of seven or higher were considered to be of high quality and to have a low risk of bias. Two reviewers (Wang ZG and Li M) independently evaluated and cross-checked the quality scores of the included studies (Table I) [Xu et al., 2013; Watson-Jones et al., 2015].
| Quality indicators from NOS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ref. | Selection | Comparability | Exposure/outcome | Score | ||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||||
| Kristensen BO et al. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | 7 | ||
| Chen T et al. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | 7 | ||
| Feng T et al. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | 8 | ||
| Roberts. ET et al. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9 | ||
| Li S et al. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | 8 | ||
| Li C et al. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9 | ||
| Li T et al. | Yes | Yes | Yes | Yes | Yes | No | Yes | No | No | 6 | ||
| Vahdat K et al. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | 7 | ||
| Tang N et al. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | 8 | ||
- NOS: Newcastle–Ottawa quality assessment scale.
- For case-control studies: (1) represents cases with independent validation; (2) cases are consecutive or representative; (3) controls are community; (4) controls have no history of EH and other diseases; (5) study controls are comparable for age and sex; (6) study controls for any additional factors; (7) cases and controls have the same method of ascertainment; (8) was follow-up long enough for outcomes to occur; and (9) cases and controls have complete follow-up.
- For cohort studies: (1) indicates the exposed cohort study representative of the population; (2) the non-exposed cohort drawn from the same population; (3) the exposure ascertainment are from secure record or structured interview; (4) EH was not present at start of study; (5) cohorts are comparable for age and sex; (6) cohorts are comparable for any additional factors; (7) assessment of EH is from secure record; (8) follow-up long enough for EH to occur; and (9) complete follow-up.
Statistical Analysis
OR and 95%CI were used to measure the strength of the association of HCMV infection and EH. A random-effect model using the Mantel–Haenszel method was used to give individual effect-size estimates in Review-Manager 5.2 software [Munafò and Flint 2004]. A χ2-based Q statistic test was performed to assess the heterogeneity of the studies [Lau et al., 1997]. Heterogeneity was considered significant at P < 0.05. The inconsistency index I2 was calculated to evaluate variation, which was caused by heterogeneity rather than by chance, and high values of the index indicate the existence of heterogeneity [Higgins et al., 2003]. The significance of the pooled OR was determined using the Z test, and P < 0.05 was considered significant.
Begg's and Egger's tests were used to estimate publication bias [Sun et al., 2014]. In these analysis, asymmetric plots suggest possible publication bias. All statistical analysis were performed using Review Manager 5.2 (Oxford, England) and Stata version 12.0 (Stata Corporation, College Station, TX). P < 0.05 was considered statistically significant.
RESULTS
Selection of Studies
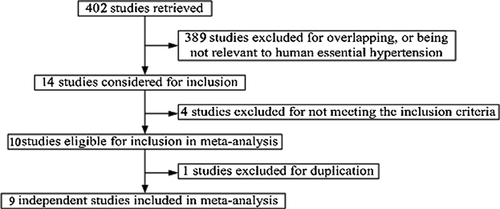
As shown in the flow diagram (Fig. 1), 394 of the 402 studies retrieved were excluded according to inclusion and exclusion criteria as defined above. One study was republished, and one study had insufficient information to allow adequate estimation of OR and 95%CI of HCMV infection risk in EH and normotensive subjects, and they were excluded. Nine studies met the inclusion criteria and were subjected to further analysis of the association of HCMV infection with risk of EH. One study included individuals of Kazakh and Han Chinese ethnicity [Tang et al., 2014]. These two groups were separated for the present analysis.
In an assessment of study quality, of the nine studies included in this meta-analysis, eight were judged to have a low risk of bias and one high risk (Table I). Because the removal of any single study from this meta-analysis did not affect the association between CMV infection and risk of EH, all nine studies qualified for inclusion in the quantitative data synthesis. The main characteristics of the nine studies pooled in this meta-analysis are shown in Table II. They include two cohort studies and seven case-control studies published between 1980 and 2015, involving a total of 11,878 subjects. Five studies were conducted in China, one in Denmark, one in Iran, and two in the U.S.
| Ref. | Year | Ethnicity | Country | Diagnosis of HCV infection | Diagnosis of EH | Matching | Source | Method | Age (year) | Result |
|---|---|---|---|---|---|---|---|---|---|---|
| Kristensen BO et al. | 1982 | White | Denmark | IgG, IgA, IgM | SBP ≥ 140 mmHg, and/or DBP ≥ 90 mmHg | Age, sex, others | C–C | ELISA | 23–64 | − |
| Chen T et al. | 1999 | Asian | China | IgA, IgM | SBP ≥ 140mmHg, and/or DBP ≥ 90mmHg | Age, sex, others | C–C | ELISA | 34–77 | + |
| Feng T et al. | 2001 | Asian | China | IgG, IgM | SBP ≥ 140mmHg, and/or DBP ≥ 90mmHg | Age, sex, others | C–C | RIA, ELISA | 34–68 | + |
| Roberts. ET et al. | 2010 | White | USA | IgG | SBP ≥ 140 mmHg, and/or DBP ≥ 90mmHg | Age, sex, others | cohort | ELISA | 66–101 | − |
| Li S et al. | 2011 | Asian | China | IgG, IgM, qT-PCR | SBP ≥ 140 mmHg, and DBP ≥ 90mmHg | Age, sex, others | C–C | PCR, ELISA | 30–65 | + |
| Li C et al. | 2012 | Non-Hispanic white, | USA | IgG, IgM | SBP ≥ 140 mmHg, and/or DBP ≥ 90 mmHg | Age, sex, others | cohort | ELISA | 16–49 | + (Women) |
| Non-Hispanic black, | − (Man) | |||||||||
| Mexican American, | ||||||||||
| Others | ||||||||||
| Li T et al. | 2012 | Asian | China | IgG, IgM | SBP ≥ 140 mmHg, and/or DBP ≥ 90 mmHg | Age, sex | C–C | ELISA | 32-75 | + |
| Vahdat K et al. | 2013 | Asian | Iran | IgG, IgM | SBP ≥ 140 mmHg, and/or DBP ≥ 90 mmHg | Age, sex, others | C–C | ELISA | 25–66 | + |
| Tang N et al. | 2014 | Asian | China | IgG, IgM, qT-PCR | SBP ≥ 140 mmHg, and/or DBP ≥ 90 mmHg | Age, sex, others | C–C | PCR, ELISA | 18–84 | + |
- HCMV, Human cytomegalovirus; C–C, Case-control study; ELISA, Enzyme-linked immunosorbent assay; RIA, Radioimmunoassay; qT-PCR, Real-time fluorescence quantitative PCR; −, Negative result; +, Positive result.
Association of HCMV and EH
Of the 11,878 participants included in this study, there were 3,864 EH patients and 8,014 control subjects (Fig. 2A). Meta-analysis of nine studies performed in a random-effect model found that EH patients had a higher risk of HCMV infection than normal control subjects (OR = 1.47, 95%CI: 1.13–1.90, P = 0.004; heterogeneity: P = 0.002, I2 = 66%). Because heterogeneity was somewhat high, a sensitivity analysis was performed by deleting studies one by one to find the source. When Kazakh participants from one Chinese study were removed, a significant association was found between HCMV infection and EH (OR = 1.26, 95%CI: 1.02–1.54, P = 0.03), and the heterogeneity was good (I2 = 42%, P = 0.09) [Tang et al., 2014]. The total effect did not change after deletion of any other studies.
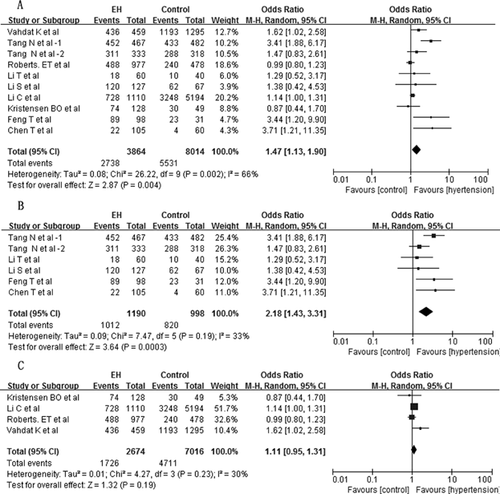
In the subgroup analysis, which assessed the effects of ethnicity, five studies of Chinese subjects were selected for further analysis. There were 1,190 EH patients and 998 normal control subjects (Fig. 2B). A significant association was found between HCMV infection and EH (OR = 2.18, 95%CI: 1.43–3.31, P = 0.0003). The heterogeneity of the five studies was acceptable (I2 = 38%, P = 0.16). The results were not changed by deletion any of the studies. In the other four studies, which covered non-Chinese participants, (2,674 EH patients and 7,016 normal control subjects), no association was found between HCMV infection and EH (OR = 1.11, 95%CI: 0.95–1.31, P = 0.19). A sensitivity analysis was performed, and the studies were removed one at a time. The results remained (Fig. 2C).
Publication Bias
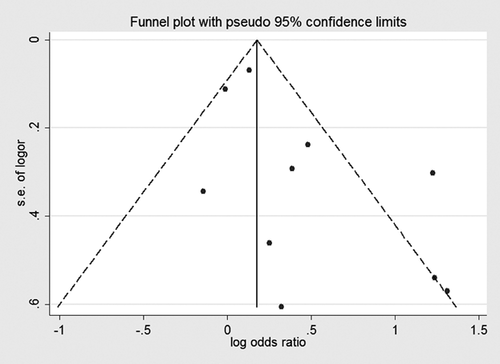
When all nine studies were included in the meta-analysis, no publication bias was detected (Fig. 3, Begg's test P = 0.210, Egger's test P = 0.058). In this way, the overall quality of papers and the publication bias were found to be acceptable.
DISCUSSION
This is the first comprehensive meta-analysis of the association between HCMV infection and risk of EH.
Assessing the risk of bias in observational studies is inherently subjective, so the subjectivity of these ratings was minimized by independent evaluations performed by two evaluators. The studies were scored based on the guidance from NOS and published checklists alongside items related to other methodological features believed to be important to studies of CMV infection and EH.
The methods used to diagnose HCMV infection in the various studies may affect the measured morbidity in both cases and controls. Anti-CMV IgG, and to a lesser extent anti-CMV IgA, are the main serologic markers of primary infection with HCMV. In total, anti-CMV IgG was assessed in eight studies, and anti-CMV IgA in one (Table II). This showed the methodology to be acceptable.
Most healthy people are infected by HCMV after birth and harbor the virus without absence of overt clinical illness [Manuel et al., 2013]. In 2011, Zhang et al. hypothesized that HCMV is an opportunistic pathogen that might contribute to EH by disrupting nitric oxide synthesis (NOS) and immune defenses while activating inflammation and the renin-angiotensin aldosterone system (RAAS), all of which are important in EH pathogenesis [Zhang et al., 2011]. In an animal model, murine CMV (MCMV) infection alone stimulated renin and angiotensin-II (AngII) expression and caused a significant increase in arterial blood pressure [Cheng et al., 2009]. Pharmacologic control of CMV infection or activity might restrict development of hypertension and atherosclerosis [Bruning et al., 1994]. Consistent with the findings of the mouse trial, HCMV might infect different types of human cells and induce expression of cytokines such as (interleukin-2, interleukin-6, tumor necrosis factor, and monocyte chemoattractant protein-1) [Bentz et al., 2006; Botero et al., 2008; Zheng et al., 2012]. In addition, HCMV infection is a risk factor for increased arterial blood pressure and aortic atherosclerosis [Kristensen et al., 1982; Roberts et al., 2010]. It is here concluded that the results of animal model and cell-based studies are consistent with those of epidemiological studies showing that HCMV infection is a risk factor for human EH.
Of the nine studies in this meta-analysis, six showed HCMV infection to be significantly closely related to EH. Roberts et al. found that not only was HCMV infection closely associated with EH but high HCMV antibody titers were positively associated with age and elevated systolic and diastolic blood pressure and inversely associated with flow-mediated dilation [Roberts et al., 2010]. This is consistent with the temporal pattern of EH development.
In two whole studies and in the male participants of one study, HCMV infection was not associated with higher risk of EH [Li et al., 2012]. EH is believed to be a multifactorial and polygenetic disease. In addition to genetic factors, such as single-nucleotide polymorphisms in the renin, mitofusin 2, or E-selectin genes [Wang et al., 2010, 2013; Yang et al., 2015], environmental factors such as stress, smoking, air pollution, diet, and various pathogens have been found to be associated with development of EH [Kunes and Zicha. 2009]. Given that 31% of normotensive subjects and 53% of hypertensive subjects are infected with HCMV, HCMV may be a risk factor for but not necessarily an independent cause of EH [Marques and Morris 2012].
To evaluate confounding factors that might have affected the results of this meta-analysis, the studies were subgrouped by race and ethnicity. HCMV infection was found to be associated with high risk of EH in Chinese individuals but not in others (P = 0.0003 vs. P = 0.19). Because some genetic properties differ across different races and ethnicities, in addition to the possibility of geographic or culture-based environmental risk factors, the association of HCMV infection with a high risk of EH suggests an associated genetic susceptibility profile in Chinese individuals, analogous to what has been observed in American Indians and Alaska Natives, who are at a higher risk for complications of influenza [Thompson et al., 2011].
Confounding variables must be considered when interpreting the results. Because EH often appears after middle age and HCMV primary infection may appear at any age, age may be a confounding variable in this meta-analysis. Low socioeconomic status may be another confounder associated with both HCMV infection and EH. However, such information has not been well reported in most studies. In addition, sample sizes, methods used for HCMV detection, and the ratio of female to male participants may also affect the analysis.
CONCLUSIONS
HCMV is an opportunistic pathogen in humans. Although animal models that employ MCMV have provided data consistent with the possibility that HCMV infection increases blood pressure by affecting vascular function and development of atherosclerosis, clinical studies have been equivocal. The current meta-analysis supports the hypothesis that HCMV is closely associated with human EH, but only in Chinese individuals. Questions as to whether HCMV directly or indirectly increases blood pressure and as to whether elevated seroprevalence of HCMV is a cause or a consequence of EH will require additional study, as will identification of the mechanisms by which HCMV might contribute to EH.
ACKNOWLEDGMENTS
We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this article.