Epstein–Barr virus-related lymphoproliferative disorder, cytomegalovirus reactivation, and varicella zoster virus encephalitis during treatment of medulloblastoma
Abstract
The case of a 14-year-old girl who developed Epstein–Barr virus-related lymphoproliferative disorder, cytomegalovirus reactivation, and Varicella zoster virus encephalitis during treatment for medulloblastoma is described. The patient was diagnosed with a cerebral medulloblastoma and treated with systemic chemotherapy, intrathecal chemotherapy, and radiotherapy. Six months later, she developed persistent low-grade fever, abdominal pain, and vomiting. Several mucosal or ulcerated lesions of the stomach and colon were found on fiberscopy. The infiltrating cells were positive for CD20 and EBER1, and the diagnosis of lymphoproliferative disorder was made. CMV antigen was found in the peripheral lymphocytes at that time. At the same time, it was noted that the patient's language was inappropriate for her age, and a facial and abdominal rash, as well as a right facial palsy, had developed. She was then diagnosed as having VZV encephalitis, because VZV was detected in the CSF. She was treated subsequently with acyclovir and oral steroid, and the VZV encephalitis resolved. The lymphoproliferative disorder improved gradually with rituximab, ganciclovir, and total nutritional support. At the time of the development of the lymphoproliferative disorder and VZV encephalitis, the patient had severe lymphopenia and this may have caused these rare phenomena in a non-transplant setting. J. Med. Virol. 83:1582–1584, 2011. © 2011 Wiley-Liss, Inc.
INTRODUCTION
While it has been known for some time that immunodeficiency-related lymphoproliferative disorders occur in solid organ transplant recipients, as well as in patients with congenital immunodeficiencies and acquired immunodeficiency syndrome (AIDS), the occurrence of lymphoproliferative disorders outside these settings has been recently recognized [Kamel, 1997; Hasserjian et al., 2009]. The case of a 14-year-old girl who developed an Epstein–Barr and cytomegalovirus-related lymphoproliferative disorder with varicella zoster virus (VZV) encephalitis during treatment of medulloblastoma is reported.
CASE REPORT
A 14-year-old girl was diagnosed with cerebral medulloblastoma in April 2009. After partial resection of the tumor, she was treated with a protocol of the Japanese Pediatric Brain Tumor Consortium for medulloblastoma, comprising four courses of systemic high-dose cyclophosphamide, vincristine, cisplatin, and etoposide, with intrathecal methotrexate and dexamethasone. Radiotherapy of the whole brain (24 Gy), whole spine (24 Gy), and cerebellar tumor bed (50 Gy) was performed during the second course of systemic chemotherapy.
In October 2009, after the 4th course of chemotherapy, the patient developed persistent low-grade fever, abdominal pain, and vomiting. Gastroscopy showed several mucosal lesions of the stomach (Fig. 1a). Several ulcerating lesions on the colon were also found on colonoscopy (Fig. 1b). These lesions were diagnosed as lymphoproliferative disorder because the lesional infiltrating cells were positive for CD20 and EBER1 (Fig. 1c). The EBV in the lymphoproliferative disorder showed monoclonality. The serum EBV titers were as follows: EB VCA IgG < 40, VCA IgM < 10, and EBNA < 10. EBV was detected (250 copies/106 cells) in the peripheral blood mononuclear cells. Interestingly, CMV antigen was not detected in the cells of the lymphoproliferative disorder, but CMV antigen was found in the peripheral lymphocytes at that time.
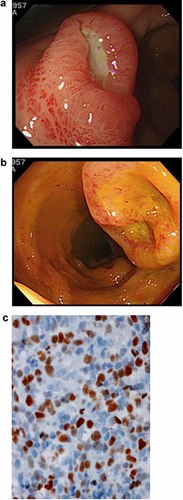
Findings of the patient's lymphoproliferative disorder (a) stomach, (b) large intestine, and (c) histology of EBER staining (stomach).
At the same time, it was noted that the patient's language was inappropriate for age, and she developed a facial and abdominal rash, as well as a right facial palsy. The CSF cell count was 1/µl, and the CSF cytopathology revealed no pathological cells, though VZV was detected by PCR. The brain MRI was unremarkable except for the residual tumor. The patient was then treated with acyclovir and oral steroid, and the symptoms, except abdominal pain, improved, and VZV in the CSF became negative. Because the abdominal pain and lymphoproliferative disorder of the stomach and colon did not improve on fiberscopy in November 2009, weekly rituximab (five times) was started. The EBER of these lesions became negative, but the abdominal pain and the size of the mucosal lesions in the stomach and colon did not improve. Administration of rituximab was stopped, and total parenteral nutritional support was then given. About a month after terminating rituximab, the elevated lesions of the stomach disappeared. The ulcerative lesions of the colon persisted with minimal improvement. Interestingly, EBER was not detected in the ulcerative lesions, but CMV antigen was detected at this time, so ganciclovir was started. Two weeks later, the ulcerative lesions of the colon improved, and CMV antigen disappeared.
Chemotherapy for medulloblastoma was terminated after the diagnosis of lymphoproliferative disorder. The patient is now doing well with no symptoms and no recurrence of medulloblastoma.
When the patient was diagnosed with lymphoproliferative disorder and VZV encephalitis, she was noted to have severe lymphopenia (375/µl) with a marked decrease of CD4-positive cells (34/µl). The decrease in CD4-positive cells had been observed for 18 months after terminating the chemotherapy for medulloblastoma.
DISCUSSION
The patient described developed Epstein–Barr virus-related lymphoproliferative disorder, cytomegalovirus reactivation, and VZV encephalitis at the same time while in an immunocompromised state during treatment for medulloblastoma.
A high incidence of EBV-related lymphoproliferative disorder is well known in patients with primary/secondary immunodeficiencies and in recipients of organ transplants such as bone marrow, heart, lung, and liver [Kawa, 2000]. Recently, there have been several reports of lymphoproliferative disorder following chemotherapy in the non-transplant setting [Johnston et al., 2008; Lee et al., 2008; Hasserjian et al., 2009]. At the onset of lymphoproliferative disorder, the present patient had severe lymphopenia with a marked decrease of CD4-positive cells, which was suggested as the cause of the lymphoproliferative disorder. Moreover, CMV reactivation was noted at the time of the occurrence of the lymphoproliferative disorder. Co-infection with herpes viruses is well known in immunocompromised patients, especially with HIV infection [Syrjanen et al., 1999; Freigassner et al., 2002].
It is reported that acute CMV infection causes EBV immunoactivation [Oill et al., 1977; Aalto et al., 1998], and CMV is associated with several indirect effects, such as increasing the incidence of opportunistic fungal infections and EBV-associated lymphoproliferative disorder after transplantation, as well as accelerating the course of hepatitis C infections in solid organ recipients [Fishman et al., 2007]. These effects of CMV may be mediated by modulation of the immune system, which could increase the pathogenicity of second agents, although the exact mechanism is not yet understood fully.
On the other hand, immunocompromised patients are more likely to develop VZV encephalitis. However, no reports have described co-infection of these three herpes viruses together, as in the present case. Severe immunosuppression by intensive chemotherapy with craniospinal radiotherapy for medulloblastoma might have caused this.
Intensive chemotherapy has improved the outcome of pediatric cancer, but more attention to the occurrence of opportunistic infections, even outside the transplant setting, is needed.