Competency in evidence-based medicine and associated factors among medical radiology technologists in Addis Ababa, Ethiopia
Abstract
Introduction
Evidence-based medicine integrates clinical expertise, patient values and best research evidence in clinical decision-making. This study aimed to assess evidence-based medicine knowledge, attitudes, practices and associated factors among medical radiology technologists in Addis Ababa, Ethiopia.
Methods
A cross-sectional study was conducted among 392 medical radiology technologists from May to August 2022 using a self-administered questionnaire. Bivariate and multivariate logistic regression identified factors associated with evidence-based medicine practice.
Results
Most medical radiology technologists (57.7%) had moderate evidence-based medicine knowledge and 94.9% had favourable attitudes. However, 64.8% demonstrated poor evidence-based medicine practice. Factors significantly associated with better evidence-based medicine practice were moderate knowledge (AOR 1.949, 95% CI 1.155–3.291), good statistical understanding (AOR 1.824, 95% CI 1.135–2.930), sufficient time for evidence-based medicine (AOR 1.892, 95% CI 1.140–3.141), institutional support (AOR 2.093, 95% CI 1.271–3.440) and evidence-based medicine resource access (AOR 1.653, 95% CI 1.028–2.656).
Conclusion
Despite moderate knowledge and positive attitudes towards evidence-based medicine, most medical radiology technologists had suboptimal utilisation. Strategies to improve knowledge, ensure dedicated time, provide institutional support and resources could enhance evidence-based radiology practice.
Introduction
Evidence-based medicine is defined as the integration of clinical expertise, patient values and the best available external clinical evidence from systematic research in the making of decisions about the care of individual patients.1-3 Competency in evidence-based practice requires knowledge and skill in all elements of EBM. It also requires the ability to critically appraise literature. Furthermore, it involves judiciously applying evidence while taking into account both the patient and the local context.1, 4-6
Over the last three decades, the medical industry has been undergoing significant transformations.7 In the field of radiology, these changes are evident in the ongoing enhancements in diagnostic modalities, the availability of non-invasive diagnostic options and the development of innovative imaging techniques.6, 8-10 Given this rapid pace of change, it is crucial for medical radiology technologists (MRTs) to incorporate EBM into their everyday radiological practices.10, 11
An evidence-based radiology practice is a practice that uses the latest literature evidence to justify and optimise imaging techniques considering patient value and preference.6, 12, 13 This approach could lead to the adoption of novel diagnostic techniques which are less expensive, non-invasive, non-ionising and potentially superior in image quality with fewer side effects.14-17
The lack of up-to-date evidence in radiology practice can potentially lead to unnecessary radiation exposure and improper imaging for patients, resulting in an increase in healthcare costs, wastage of time and patient anxiety.1, 9, 10 Most importantly, it would lead to severe radiation risks to the patient that might benefit from non-ionising modalities (particularly in the paediatric population).6, 18 All these practices directly contradict the main principle of radiology: ‘as low as reasonably achievable’.19
So, to address those challenges in radiology practice, several studies advocated EBM to become an integral part of clinicians' daily practice.8-10 In Ethiopia, while there are a few studies that have explored EBM competency among health professionals, most of these studies have been conducted with relatively small sample sizes.20-26 Moreover, as far as the knowledge of the authors, there is no local EBM article that shows data regarding MRT professionals.
Therefore, this study assessed the EBM competency and the associated factors among MRT professionals in Addis Ababa, Ethiopia.
The study provides baseline data on MRTs' current EBM competency levels and barriers hindering EBM implementation in radiology. Additionally, the study report will aid future EBM research across professions and provide key inputs for meta-analyses and systematic reviews.
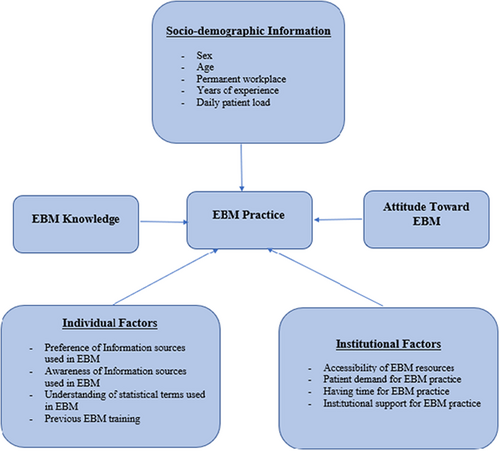
The conceptual framework of this study was summarised as of under Figure 1.
Methods
Study area and period
Addis Ababa, the capital of Ethiopia and the African Union's hub, had an estimated population of around 4.59 million as of 2018.27 The study was conducted among hospitals (public and private) and diagnostic centres in the city. According to the Federal Ministry of Health (FMOH) 2020/2021 annual report, there are 12 public hospitals, 24 private hospitals and 7 diagnostic centres in the city.28 The selection of Addis Ababa as the study area was primarily due to its substantial number of MRT experts (728), which is higher than any other region. This study was conducted from 16 May to 19 August 2022.
Study design, population and setting
A cross-sectional design was conducted. The source population encompassed all MRTs in the specified region (occasionally known as radiographers), while the study populations were those randomly selected and fulfilled the inclusion criteria. Each MRT expert was treated as an individual study unit. Eligibility for the study hinged on whether the MRT professionals were providing radiology services in Addis Ababa during the study period.
Sample size determination and sampling technique
Sample size determination
The sample size for this study was calculated using a single population proportion formula, considering several key assumptions. These included a 95% confidence interval, Zα/2 (1.96), a 5% margin of error (d = 0.05) and a 50% proportion of knowledge, attitude and practice towards EBM, as indicated by previous study.26
The computations resulted in a minimum sample size of n = 384. To account for a potential 10% non-response rate, the sample size was increased to 423, ensuring an adequate number of participants for the study.
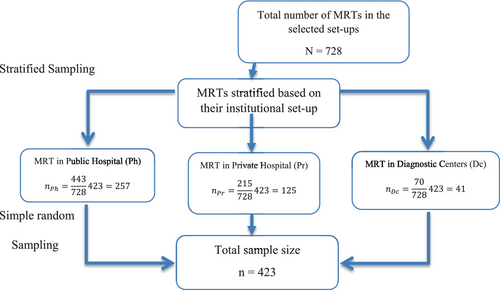
Sampling technique
The initial step involved acquiring a comprehensive list of MRTs from various hospitals and diagnostic centres. The MRTs were then categorised based on their work environment due to differences in institutional setup (public hospital (NPh = 443), private hospital (NPrh = 215) and diagnostic centre (NDc = 70)). After that, a given sample size (n = 423) was allocated in each stratum based on MRTs proportion using a standard proportionate allocation formula . Lastly, within each specified stratum, a simple random sampling technique was implemented using a lottery method (Fig. 2).
Data collection instruments and procedures
The questionnaire tool is divided into six main sections. The first section gathers six pieces of socio-demographic information, the second section assesses EBM knowledge through a 15-item, five-point Likert scale, the third section uses a 17-item, five-point Likert scale to measure MRTs' attitudes towards EBM, the fourth section uses a five-point scale to evaluate the frequency of EBM-related terms in practice and the fifth section examines factors influencing individual practice, with four sub-domains. This section has 28 items rated on three-point and five-point Likert scales. The last section asks MRTs to rate perceived institutional barriers to EBM practice, divided into four subdomains with 15 statements.
The Noor EBM questionnaires were used for competency assessment in all elements of EBM, based on their knowledge and practice and this questionnaire is a certified tool to evaluate competency, attitude and behaviour towards EBM among healthcare professionals.29 It was slightly modified to fit the local radiology practice of MRTs. Other sections were adapted from local literature.24, 26 Data collection was conducted by three nurse professionals using a Google form.
Study variables
In this study, EBM practice was the dependent variable. The independent variables included socio-demographic data, attitude towards EBM, individual factors, institutional factors and EBM knowledge.
Operational definition
EBM knowledge
It is measured using a 15-item scale, with responses labelled as correct, neutral or incorrect. The mean score of the responses is used to categorise knowledge levels according to Bloom's cut-off point (60–79%).30 Thus, individuals with a specified range were in moderate knowledge categories while those who scored above and below the range were in the high and low level of knowledge, respectively.29-31
Attitude towards EBM
It is measured using a 17-item scale, with responses labelled as favourable, neutral or unfavourable. The mean score of the responses is used to categorise attitudes as either favourable or unfavourable.24, 26, 31
EBM practice
It was measured by 10 questions on a five-point Likert scale. Individual items were assessed based on active, neutral and passive labelling in which those who always and often practise EBM were labelled as active practicians and those who never and seldom practise EBM were labelled as passive practicians while sometimes remained intact.
All individual answers for the total practice questions were computed to obtain the total mean scores. The mean score of the responses is used to categorise practices as either good or poor.24, 26
Data quality control
A pre-test of the questionnaire was conducted at Arba-Minch and Hawassa city before the actual data collection on 5% of the sample which was not included in the study. After the pre-test, the questionnaire was checked for possible reliability, completeness and clarity issue. Data error was handled by using a strict value and labelling rule in designing the Google form.
The resultant data showed that the questionnaire had a strong internal consistency based on Cronbach alpha test scores. The reliability for knowledge questions had a Cronbach's alpha value of 0.894, the attitude had a Cronbach's alpha value of 0.701 and practice had a Cronbach's alpha value of 0.818. Additionally, two-day training was given for the data collector on the data collection tools and procedures. Continuous follow-up and supervision throughout the data collection period were employed.
Data analysis
After the data collection process, the incoming data from the Google sheet was checked, cleaned and coded in Excel 365 to be exported into SPSS V 26 for further data analysis. In SPSS, the recoding of variables into their respective variable label and value label was initially employed.
Descriptive statistics (frequency, per cent and mean) were used to describe the socio-demographic characteristics, knowledge, attitude and practice of MRTs towards EBM as well as the individual and institutional barriers. In analytical statistics, a bivariate analysis was initially used to select the independent variables for the final multivariable binary logistic regression. The criteria for including an independent variable were based on the P-value which is (p < 0.25). Finally, multivariable binary logistic regression with a 95% confidence level was employed to assess the association between dependent and independent variables. Variables with a significant association were identified based on AOR, 95% CI and p-value ≤0.05, and finally, the strength of association was declared.
Results
Socio-demographic characteristics
In a survey of 423 MRTs, 392 (92.6%) participated. Of these, 69.6% were men, and 59.4% worked in public hospitals, with the rest in private hospitals (30.4%) and diagnostic centres (10.2%). The majority had between one and five years of radiology experience (81.6%), and while 10.2% had a master's degree, the rest held bachelor's degrees (see Table 1).
| Variables | Permanent workplace | Total | |||
|---|---|---|---|---|---|
| Public hospital | Private hospital | Diagnostic centre | |||
| Sex | Female | 66 (55.6%) | 34 (58.6%) | 19 (16.0%) | 119 (30.4%) |
| Male | 167 (61.2%) | 85 (31.1%) | 21 (7.7%) | 273 (69.6%) | |
| Age | 20–24 | 40 (49.4%) | 29 (35.8%) | 12 (14.8%) | 81 (20.6%) |
| 25–29 | 163 (61.7%) | 76 (28.8%) | 25 (9.5%) | 264 (67.3%) | |
| 30–34 | 24 (63.2%) | 12 (31.6%) | 2 (5.3%) | 38 (9.6%) | |
| 35–39 | 4 (80.0%) | 0 (0.0%) | 1 (20.0%) | 5 (1.2%) | |
| 40–44 | 2 (50.0%) | 2 (50.0%) | 0 (0.0%) | 4 (1.0%) | |
| Years of experience | 1–5 Years | 187 (58.4%) | 98 (30.6%) | 35 (10.9%) | 320 (81.6%) |
| 5–10 Years | 36 (64.3%) | 15 (26.8%) | 5 (8.9%) | 56 (14.3%) | |
| >10 Years | 10 (62.5%) | 6 (37.5%) | 0 (0.0%) | 16 (4.1%) | |
| Patient workload | Low | 5 (21.7%) | 7 (30.4%) | 11 (47.8%) | 23 (5.86%) |
| Medium | 47 (30.5%) | 83 (53.9%) | 24 (15.6%) | 154 (39.3%) | |
| High | 181 (84.2%) | 29 (13.5%) | 5 (2.3%) | 215 (54.8%) | |
| Educational level | BSc | 205 (58.2%) | 110 (31.3%) | 37 (10.5%) | 352 (89.8%) |
| MSc | 28 (70.0%) | 9 (22.5%) | 3 (7.5%) | 40 (10.2%) | |
Evidence-based medicine knowledge
Of all participants, the majority (57.7%) had a moderate level of EBM knowledge, while 38.5% had a poor level of EBM knowledge and only 3.8% showed a high level of knowledge. The average EBM knowledge score was 3.14 (±0.86 SD). Most MRTs (61.0%) correctly identified the need for critical appraisal of research for clinical decision-making. But the other two basic elements of EBM regarding patient care (42.6%) and clinical expertise (38%) were incorrectly answered by a slight majority of MRTs more than those who correctly answered the question.
In terms of other EBM competencies, a considerable proportion of MRTs (41.1%) correctly identified the Cochrane Library as a source of systematic reviews, while 26.5% did not.
Nearly half (49%) understood the PICO (patient, intervention, comparison and outcome) format structure, but 28.3% did not. A notable 41.6% were unaware that meta-analysis provides a higher level of evidence than case–control studies.
While most MRTs (56.6%) recognised the use of EBM in uncertain clinical situations, only 39.8% of them agreed that access to evidence summaries improves practice, and just 36% knew that EBM promotes self-directed learning.
Attitude towards evidence-based medicine
A significant majority of MRTs (94.9%) were identified as having a favourable attitude towards EBM. The average attitude score was 3.84 (±0.46 SD). Over half of the MRTs (55.4%) disagreed that EBM undermines good clinical practice. Similarly, most MRTs (58.2%) were confident that EBM enhances patient health outcomes, and 60.2% expressed a desire to learn more about EBM if given the opportunity. Furthermore, 56.9% disagreed that EBM has limited value in radiology, and 60.7% acknowledged the significance of research findings.
Evidence-based medicine practice
Unlike EBM knowledge and attitude results, only 139 (35.5%) individuals had a good EBM practice while the remaining 253 MRTs (64.8%) were in the poor EBM practice categories. The mean score for EBM practice was 2.91 ± 0.86 SD. Most of the respondents 178 (45.4%) ‘Never’ or ‘Seldom’ (passive practice) utilise multiple search engines for systematic review while 106 individuals (27%) were categorised as active users. Similarly, the majority of included MRTs (49.7%) were classified as passive practitioners in searching for evidence-based medicine material from published journals only. In the ‘ASK’ domain of EBM core competency, a vast majority of respondents (47.7%) were categorised as having a passive EBM practice.
Individual factors for evidence-based medicine practice
Preferences for information sources used in evidence-based medicine
The results from this study showed that the majority of MRTs (63.0%) preferred electronic databases as an evidence source, followed by medical textbooks (52.3%). Consulting radiologists and senior MRTs were the least preferred source (28.3%).
Awareness of information sources used in EBM
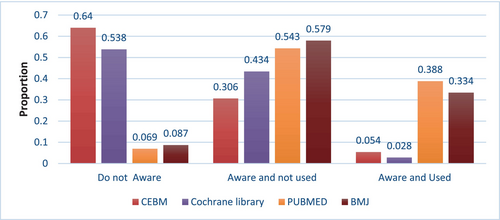
Regarding awareness of information sources, 93.1% of MRTs knew about the PUBMED database, but only 38.8% used it regularly. The Evidence-Based Medicine journal was known by 91.3% of MRTs, but only 33.4% had used it. The least known sources were the Cochrane Database (46%) and the Center of Evidence-Based Medicine (35.9%) (see Fig. 3).
Understanding of statistical terms used in EBM
Most participants understood statistical terms like ‘sensitivity’ (61.0%), ‘specificity’ (62.2%) and ‘confidence interval’ (67.9%). However, complete understanding was lower, with only 34.4%, 34.4% and 28.1%, respectively, claiming full comprehension of these terms. Overall, the majority of MRTs (57.9%) had a poor understanding of EBM statistical terms (see Table 2).
| Do not understand | Some understanding | Complete understanding | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Confidence interval | 16 | 4.1% | 266 | 67.9% | 110 | 28.1% |
| p-value | 136 | 34.7% | 185 | 47.2% | 71 | 18.1% |
| Sensitivity | 18 | 4.6% | 239 | 61.0% | 135 | 34.4% |
| Specificity | 13 | 3.3% | 244 | 62.2% | 135 | 34.4% |
| Likelihood ratio | 247 | 63.0% | 121 | 30.9% | 24 | 6.1% |
| Relatively risk | 228 | 58.2% | 144 | 36.7% | 20 | 5.1% |
Institutional factors for evidence-based medicine practice
The most frequently reported institutional factors for evidence-based practice were lack of free internet access (64.8%), lack of patient preference for EBM practice (61.0%), lack of patient belief for EBM practice (59.7%), lack of time to search and read research papers (51.5%) and lack of support from supervisor (52.3%) (see Table 3).
| The institutional factor for EBM practice | Yes | |
|---|---|---|
| n | % | |
| Lack of time to apply research evidence | 81 | 20.7% |
| Lack of access to research articles | 101 | 25.8% |
| Lack of support from a colleague of a different profession | 105 | 26.8% |
| Lack of support in the whole work environment | 106 | 27.0% |
| Lack of practice guidelines access | 122 | 31.1% |
| Lack of time to search and read research papers | 202 | 51.5% |
| Lack of support from a supervisor | 205 | 52.3% |
| Lack of patient belief for EBM practice | 234 | 59.7% |
| Lack of patient preference for EBM practice | 239 | 61.0% |
| Lack of free internet access | 254 | 64.8% |
Factors associated with evidence-based medicine practice
In a bivariate analysis, several factors were found to significantly correlate (p = <0.20) with EBM practice, including understanding of statistical terms, time availability for EBM practice, EBM knowledge and institutional support for EBM practice.
Hosmer and Lemeshow's test could not reject the hypothesis of model appropriateness due to the statistical insignificance of the Chi-square result (X2 = 11.065, p = 0.136). The variance inflation factor (VIF) was below 10 for all the selected variables, indicating that there is no multicollinearity issue among them. Finally, all the assumptions for binary logistic regression were met without forgetting to mention the dichotomous nature of the dependent variable.
During the multivariable analysis, the high performance of the full model was seen as it significantly predicts 82.4% of the observed respondents (X2 = 71.726, df = 7, p < 0.001). The variable's understanding of statistical terms, having time for EBM practice, EBM knowledge, accessibility to EBM resources and institutional support for EBM practice were significantly associated with EBM practice.
Thus, MRT who had moderate EBM knowledge was 1.95 times (AOR = 1.949, 95% CI = 1.155, 3.291) higher odds to have a good EBM practice compared to those who had poor EBM knowledge. The odds of having a good EBM practice were 1.82 times (AOR = 1.824, 95% CI = 1.135, 2.930) higher for MRTs who had a good understanding of statistical terms when compared with those individuals with a low understanding of statistical terms. MRTs who had enough time to search and apply research evidence were 1.89 times (AOR = 1.892, 95% CI = 1.140, 3.141) higher odds to have a good EBM practice compared to those who do not.
The odds of having a good EBM practice were 2.09 times (AOR = 2.093, 95% CI = 1.271, 3.440) higher for MRTs who have institutional support than those who do not have institutional support. MRTs who had access to EBM resources were 1.65 times (1.028, 2.656) more likely to practice EBM than others who did not have access to EBM resources (see Table 4).
| Variables | Response | EBM practice | COR (95%CI) | AOR (95%CI) | |
|---|---|---|---|---|---|
| Poor practice (%) | Good practice (%) | ||||
| Permanent workplace | PH | 63.2 | 52.5 | 1 | |
| PrH | 28.5 | 33.8 | 0.504 (0.256, 0.995)* | ||
| DC | 8.3 | 13.7 | 0.721 (0.351, 1.484) | ||
| Daily workload | Low | 5.5 | 6.5 | 1.623 (0.668, 3.946) | |
| Medium | 33.6 | 49.6 | 2.049 (1.327, 3.165)** | ||
| High | 60.9 | 43.9 | 1 | ||
| Educational level | BSC | 92.9 | 84.2 | 1 | |
| MSC | 7.1 | 15.8 | 2.455 (1.267, 4.755)** | ||
| Previous EBM training | No | 92.9 | 82.0 | 1 | |
| Yes | 7.1 | 18.0 | 0.349 (0.183, 0.666)** | ||
| Awareness of CEBM library | Unaware | 64.4 | 63.3 | 1 | |
| ANU | 32.4 | 27.3 | 0.858 (0.540, 1.365) | ||
| AU | 3.2 | 9.4 | 3.010 (1.202, 7.538)* | ||
| Awareness of BMJ library | Unaware | 7.1 | 11.5 | 1 | |
| ANU | 60.1 | 54.0 | 0.555 (0.268, 1.150) | ||
| AU | 32.8 | 34.5 | 0.651 (0.304, 1.393) | ||
| Awareness of Cochrane library | Unaware | 54.2 | 53.2 | 1 | |
| ANU | 43.9 | 42.4 | 0.984 (0.644, 1.504) | ||
| AU | 2.0 | 4.3 | 2.222 (0.656, 7.525) | ||
| EBM knowledge | Low | 47.8 | 21.6 | 1 | 1 |
| Moderate | 49.0 | 73.4 | 3.318 (2.057, 5.351)** | 1.949 (1.155, 3.291)** | |
| High | 3.2 | 5.0 | 3.529 (1.186, 10.500)* | 1.942 (0.580, 6.496) | |
| Institutional Support | No | 64.4 | 35.3 | 1 | 1 |
| Yes | 33.6 | 64.7 | 3.630 (2.350, 5.608)** | 2.093 (1.273, 3.440)* | |
| Having Time | No | 74.3 | 43.9 | 1 | 1 |
| Yes | 25.7 | 56.1 | 3.698 (2.387, 5.730)** | 1.892 (1.140, 3.141)** | |
| Understanding of Stat-Terms | Poor | 71.1 | 48.9 | 1 | 1 |
| Good | 28.9 | 51.1 | 2.575 (1.675, 3.956)** | 1.824 (1.135, 2.930)** | |
| Accessibility of EBM resource | No | 68.0 | 44.6 | 1 | 1 |
| Yes | 32.0 | 55.4 | 2.637 (1.722, 4.038)** | 1.653 (1.028, 2.656)* | |
- * Stands for p < 0.05.
- ** Stands for p < 0.01.
- ANU, aware but not used before; AOR, adjusted odds ratio; AU, aware and used before; BMJ, British Medical Journal; BSC, Bachelor of Science; CEBM, Center for Evidence-Based Medicine; COR, crude odds ratio; DC, diagnostic centre; EBM, evidence-based medicine; MSC, Master of Science; Ph, public hospital; Prh, private hospital; Stat-Terms, statistical terms.
Discussion
According to the findings of the current study, 57.7% of MRTs had moderate EBM knowledge, 38.5% poor and 3.8% high, with an average score of 3.14 + 0.86 SD. This aligns with a Malaysian study where most doctors (60.9%) had moderate EBM knowledge, followed by high (32.9%) and low (6.2%). They also concluded that the participants' overall knowledge of EBM was suboptimal.31 Similarly, a majority (64.9%) of physicians in Wuhan, China, had a moderate understanding of EBM.32
However, results from an international review of 57 studies found that healthcare professionals, including primary care practitioners, residents, specialists and subspecialists, generally have poor EBM knowledge in the awareness of EBM.33 Another local study also found that the majority of nurses (46.1%) had a poor level of knowledge.20 Similarly, in a survey at Debre Berhan Referral Hospital, 74.3% of physicians and nurses rated their EBM knowledge as low.21 This was also observed in radiology professionals. For instance, a study in Ghana revealed that only 43.2% of respondents were aware of how to critically appraise research literature, and 48.2% lacked understanding about meta-analysis and systematic reviews.8
Considering the above study results, the result of the current study is reasonably consistent with the studies which were done by similar methodologies. However, comparisons with other studies were challenging due to the methodological and scoring differences.
Furthermore, many local studies assessed EBM knowledge by the understanding of statistical and epidemiological terms only. So, comparisons with those studies would be worthless.
In summary, it can be concluded that the participants of this article had a moderate level of EBM knowledge. Thus, if they had provided comprehensive EBM training, either integrated into their undergraduate program or offered as an advanced course, they could potentially enhance their EBM knowledge significantly to a higher level.
Regarding MRTs attitude towards EBM, the current study reveals a highly positive attitude towards EBM as 94.9% of them scored above the mean value. A significant majority (62.2%) expressed interest in learning more about EBM, and 55.4% of MRTs did not view EBM as a threat to clinical practice. Furthermore, 56.9% of MRTs recognised its substantial value in radiology.
When compared to similar studies, both globally and locally, this study's attitude results were among the highest. Comparable results were found in a Ghana study where 91.1% believed in the enhancement of medical practice through recent evidence8 and a majority of Jordanian radiologists (>80%) acknowledged the importance of Evidence-Based Radiology (EBR) for clinical practice and patient care.10
Despite a relatively lower percentage values among local literature, most participants held favourable attitudes towards EBM. For instance, a Debre Berhan study reported that 62.9% of physicians and nurses had a positive attitude towards this approach.21
The relatively high attitude observed in the current study might be attributed to the participants' curiosity about this novel paradigm. Their professional background could potentially explain the high attitude result, as seen in the two aforementioned radiology-related studies. However, additional research is required to validate this association. Broadly speaking, this outcome could act as a go-ahead signal for policymakers, given that most MRTs would likely embrace the incorporation of EBM into clinical or academic sectors.
Our study also revealed a low level of EBM practice among the majority of MRTs, with 64.8% classified as poor practitioners. Roughly comparable findings were also discovered in previous local studies as well as in articles which were done among radiology professionals.
For instance, 60% of healthcare professionals in northwest Ethiopia23 and 55% in the Amhara region referral hospital were found to have poor EBM practice.20
However, a study in Wuhan, China reported 76% of physicians often or sometimes applied EBM, attributing this to organisational and managerial efforts.32
Generally, the low prevalence of EBM practice among MRTs is a matter of significant concern. It calls for immediate intervention from healthcare institutions, policymakers and professional bodies to provide necessary institutional support and resources for improved EBM practice. By doing so, they can create an environment that encourages continuous learning and application of EBM principles among MRTs. This will not only benefit the professionals and the institutions they represent, but it will also significantly contribute to the quality of patient care.
EBM competencies result of the present study indicates that most MRTs (61%) were aware of the need for critical appraisal of literature, which is an essential first step in practising EBM.1, 6 However, fewer respondents correctly answered questions about integrating patient values (42.6%) and clinical expertise (38%), which are also core principles of EBM.5, 6
This highlights a concerning gap, as evidence-based practice requires the integration of all three elements.1, 5, 6 The lack of understanding regarding patient-centred care and clinical judgement may stem from insufficient training and the poor EBM application observed in the current study results.34
In assessing EBM core competencies, 41.1% of MRTs correctly identified the Cochrane Library as a source of systematic reviews, yet only 49.7% of them actually searched journals to find evidence. This reveals a discrepancy between awareness and application of resources to acquire evidence, which is among the core competencies in EBM.5, 6
Similarly, in the ‘ask’ domain of EBM core competencies, though many (49%) knew of the PICO framework for asking clinical questions, just over half (47.7%) translated questions into PICO format in practice. Structured clinical questions using PICO are essential for searching literature in an evidence-based approach.5, 6 Thus, most of our participants had poor practice in organising clinical questions even if a slight majority were aware of the scientific format.
Additionally, 41.6% did not recognise meta-analyses as higher quality evidence than case–control studies. The practice assessment results revealed that most respondents (45.4%) do not routinely search for systematic reviews, which is concerning given that identifying and preferentially using higher levels of evidence is fundamental to EBM.5, 6
The knowledge gaps regarding core competencies likely contribute to the poor EBM application observed. Targeted training on constructing clinical questions, acquiring evidence from literature and appraising evidence quality could address these deficiencies.
In the present study, the key factors for EBM practice were lack of free internet access, having time for EBM practice, EBM Knowledge, institutional support for EBM practice and patient belief and preference for EBM practice. This result aligns with findings from previous research. A systematic review of 57 studies found that lack of resources, time, skills, access, knowledge and finances were frequently reported obstacles to practising EBM.33 Our multivariate analysis specifically highlighted five factors significantly associated with better EBM utilisation: moderate EBM knowledge, good understanding of statistics, sufficient time for searching and applying evidence, institutional support and access to EBM resources. Two similar local studies in Ethiopia corroborate some of these findings.
A study in Amhara hospitals found EBM training, knowledge, communication skills, internet access and evidence-based guidelines predicted better EBM utilisation.20 In another local study among lab technologists, knowledge, internet access, adopting EBP and being single were associated with superior EBM practice.22
The consistency of barriers and associated factors across diverse studies highlights opportunities for targeted interventions. Strategies that have improved EBM utilisation elsewhere could be adapted for radiology technicians in our setting. Key approaches may include integrating EBM training into curricula and lifetime education, providing resources and internet access, allotting dedicated time for searching and appraisal, fostering institutional leadership support and promoting a culture valuing current best evidence. Applying such multifaceted EBM-enabling initiatives could significantly enhance evidence-based radiology practice.
Limitations
The limitations of this study were the self-reported nature of the questionnaires, and its inability to measure the actual skill of the respondents as part of EBM competency. Therefore, causal relationships were not determined and MRTs opinions were captured by qualitative data. In addition to that, the dichotomisation of variables to facilitate the comparison across similar studies may limit the generalisability of the result across studies done on different design and settings.
Bivariate screening of the predictor may also be a potential source of modelling bias. So, future studies should attempt to determine a better way of measuring and analysing composite scores.
Despite the limitations, the study had several important strengths. The use of stratification and proportional allocation in the sampling strategy ensures a balanced representation across various workplace environments. The high response rate of 92.6% enhances the generalisability of the findings. Use of previously validated EBM measures (the Noor questionnaires) establishes the reliability of the instruments. Together, these strengths provide a rigorous approach to assess the current state EBM utilisation among MRTs.
Conclusions
This study revealed that the majority of MRTs possess a suboptimal understanding of EBM and a highly positive attitude towards it. However, the actual application of EBM was found to be low, with poor practice prevalent among most. Factors contributing to better EBM utilisation included having a moderate level of knowledge, understanding statistics, having enough time, receiving institutional support and having access to resources. Identified obstacles were the absence of internet, time limitations and insufficient support from the organisation.
MRTs recognise the importance of EBM but face challenges in effectively implementing it due to inadequate competency. Enhancing knowledge through training and creating a supportive environment could significantly improve EBM practice. These findings offer valuable perspectives to develop strategies that encourage EBM in daily radiological practice.
Conflict of Interest
The authors declare no conflict of interest.
Ethics Statement
Ethical approval for this study was obtained from the Institute of Health, Bule Hora University Review Board with Ref.no: BHU/RPD/808/14. Verbal consent was obtained from each study participants.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.