The impact of COVID-19 on Western Australian medical imaging clinical practice and workplace
Abstract
Introduction
Medical imaging plays a key role in the management of patients with coronavirus disease-2019 (COVID-19). This field is at risk from the impacts of the pandemic on the practice and workplace of medical imaging professionals (MIPs). Recent research has explored this impact internationally and in various states of Australia; however, the impact of the pandemic on Western Australian (WA) MIPs is yet to be examined.
Methods
This cross-sectional study aimed to address this issue by surveying clinically practicing WA MIPs on their experience of the impact of COVID-19. The survey was conducted online between the 1st and the 31st of May 2021 and encompassed 101 clinical sites.
Results
Fifty-one valid (17.1%) responses were recorded, and a majority (66.7%) of the participants were employed in public hospitals. The results showed that most participants (94.1%) perceived an impact on their clinical practice, with expressions of insufficient access to personal protective equipment (PPE). The use of all the appropriate PPE items were dependent on whether the participants were employed in a public hospital, private hospital, or a private practice (P = 0.001). Perceived imaging volume decrease across modalities did not differ significantly among the workplaces, except for interventional radiology (P = 0.006). The participants also expressed concerns about inadequate psychological support.
Conclusions
COVID-19 has enhanced infection control procedures and modified the routine imaging patterns. Specifically, WA medical imaging centres have altered their PPE and cleaning procedures based on updated health advice. Efforts should be taken to strengthen the support provided to the staff members and to ensure adequate access to PPE supplies.
Introduction
Coronavirus disease-2019 (COVID-19) has impacted the healthcare systems worldwide, with healthcare professionals across many disciplines adopting changes in their practice to minimise the infection risk.1-4 The discipline of medical imaging is at an increased risk for infection transmission as clinical practice involves close interaction with high volumes of vulnerable patients.2, 5-7 Medical imaging also assists in diagnosing complications secondary to COVID-19 and, therefore, involves interaction with patients who have tested positive for the disease.5 Ultimately, vulnerable patients and staff share an environment with patients who are positive or at a high risk for COVID-19 infection, which demonstrates the importance of adopting procedures to control infection transmission.1-4, 7-10
Understanding how medical imaging professionals (MIPs), including radiographers, branch managers and technical supervisors, have been impacted by COVID-19 in relation to their practice and workplace is important for the documentation of current practice, a foundation upon which improvements can be made to cultivate best practices. Documentation of current practice involves outlining and explaining the practices that are being implemented currently within the clinical environment, thereby facilitating the assessment of the MIPs' ability to fulfil their ethical and safety obligations as per their governing board.11 In Australia, this board is known as the Medical Radiation Practice Board of Australia (MRPBA). The board has outlined that it is within the scope of practice of a MIP to ensure patient safety in medical imaging centres and their responsibility to minimise the risk of infection transmission.12 Additionally, the MIPs' perspective of the impact of COVID-19 is important in ensuring that these frontline workers receive the necessary support and training to protect themselves and mitigate incidents in the workplace.
In the present pandemic scenario, several studies on COVID-19 have emerged. Most of the published articles are dominated by international studies, with the European and Asian countries making most of the contribution.8-10, 13, 14 Blažić et al2 explored in their study the perspective of MIPs on the utilisation of imaging methods during the COVID-19 pandemic. Their study involved 50 medical imaging centres, including one Australian institution. The researchers reported a perceived increase in the use of portable chest imaging owing to the accessibility of X-ray equipment and the focus on minimising patient transport.2 Only three articles have so far explored the perspectives of Australian MIPs on the impact of COVID-19, however these studies do not provide the Western Australian (WA) perspective.15-17 One of these studies has delved into the perspectives of MIPs and radiation therapists across Australia; however, this study has not stated how many WA participants were involved.15 The remaining two articles are commentaries which have described the impact of the pandemic within five Queensland (QLD) clinical sites and one New South Wales (NSW) clinical site, where the severity of the COVID-19 situation is different from that in WA.16, 17 Both articles are limited as they describe very specific impacts within a small sample of clinical sites, and, therefore, the findings cannot be generalised to the greater Australian population.16, 17 These three studies have reported that infection control procedures have been quickly implemented, including increased utilisation of portable imaging, enhanced cleaning procedures and implementation of personal protective equipment (PPE) protocols.15-17 Additionally, an Australasian study has explored the impact on sonographers, although the differences in sonographic practices limits the application of this study.18 Given the continued impact of COVID-19 worldwide and the lack of reports on its impact on imaging practice in WA, this research was accurately timed. This is the second year of the pandemic, and WA has so far experienced five outbreaks, including the ongoing one.19 The findings from this study are expected to assist in mitigating the challenges that the MIPs may face during future outbreaks.
This study explored the impact of COVID-19 on WA MIPs workplace and practice, with the intention of documenting the changes in practice related to infection control. Additionally, it has identified WA MIPs perception of workplace preparedness with a focus on PPE supplies and highlighting potential areas of improvement.
Materials and Methods
Study design
A cross-sectional online survey constructed and distributed via Qualtrics (Qualtrics LLC, Provo/Seattle, USA) was selected to maximise the population reach and ensure practicality in the complex environment created by the pandemic.20, 21 Pilot testing was done prior to survey distribution, with the involvement of six MIPs from both private and public sites and one statistician. The participants involved in the pilot testing were excluded from the formal study to avoid bias.
The survey collected both quantitative and qualitative data and comprised yes/no and comment-box type questions. The supplementary open-ended questions allowed the participants to elaborate on some answers, which aided in providing context and depth to the results.20, 21 The survey consisted of five key sections: (1) demographic information, (2) impact on practice, (3) impact on workplace, (4) infection control and (5) workplace preparedness. The survey questions were constructed based on surveys in similar studies (Supporting Information). 2, 8-10, 15-17, 22, 23
Study population and sampling
This study was approved by the Curtin University Human Research Ethics Committee (HRE2021-0186). The study population was determined using the total number of registered MIPs in WA (1339) as per the latest report of the MRPBA released in 2019/2020.24 Purposive sampling was used to invite clinically practicing WA MIPs to participate anonymously via a link shared through email with the university's 101 clinical placement contacts on the 1st of May 2021.20, 21 The participants were given 4 weeks' time to complete the survey (Supporting Information). Informed consent was obtained from all participants who agreed to participate in the study.
With a 95% confidence interval and 5% margin of error, the total sample size required for this study was 299. The total number of registered MIPs in WA (1339) was utilised as per the data available from the MRPBA resources.24 However, the actual total population would be less as not all registered professionals practiced during the COVID-19 pandemic and/or were practicing at the 101 clinical sites contacted. The responses were included in the data analysis if the participants answered all questions in the survey, while those that were incomplete and did not meet the eligibility criteria were excluded.
The survey recorded 71 responses, of which 51 were valid and were included in the data analysis. Twenty responses were excluded because they were either incomplete or were provided by participants who did not meet the eligibility criteria. Thus, the response rate was estimated to be 17.1%.
Data analysis
The data were analysed using Microsoft Excel v2109 (Microsoft Corp, Redmond, US) and SPSS Statistics v27 (IBM, Armonk, NY, USA). Descriptive and inferential statistics were utilised to analyse the quantitative data. A Fisher–Freeman–Halton exact test of independence was employed to determine whether the perceptions of the participants were independent of their workplace (i.e. public hospital, private hospital or private practice).25 Importantly, if the participants were engaged in private practice and if that practice operated within a public or private hospital, they were considered to belong to the hospital type they operated in. The two participants who selected ‘other’ as their workplace were assumed to belong to the public hospital group based on their comments. An independent samples t-test was applied to compare whether the mean percentage change between the group hospitals and private practice was different or the same for the perceived decrease in imaging volume per modality.26 A P-value of <0.05 was considered statistically significant.25, 26 Independent samples effect size was assessed using Cohen's d value, and a value of >0.8 was considered a ‘large’ effect size and of practical significance.27
The text responses from the open-ended questions in Section (5) were analysed using thematic analysis with a combination of deductive and inductive coding.28
Results
The demographic characteristics of the 51 respondents who provided valid responses are presented in Table 1. Six participants selected ‘other’ for modalities, and this included dual-energy x-ray absorptiometry (DEXA).
| Characteristic | Frequency | Percent (%) |
|---|---|---|
| Workplace | ||
| Public hospital | 34 | 66.7 |
| Private hospital | 5 | 9.8 |
| Private practice | 10 | 19.6 |
| Other | 2 | 3.9 |
| Capacity | ||
| Medical Imaging Supervisor | 14 | 27.5 |
| Branch Manager | 4 | 7.8 |
| Radiographer | 33 | 64.7 |
| Other | 0 | 0 |
| Years of experience | ||
| 0–9 years | 19 | 37.3 |
| 10–19 years | 15 | 29.4 |
| 20–29 years | 4 | 7.8 |
| 30–39 years | 9 | 17.7 |
| More than 39 years | 4 | 7.8 |
| Modalities offered by workplace | ||
| Emergency radiography | 37 | 72.6 |
| General radiography | 49 | 96.1 |
| Mammography | 24 | 47.1 |
| CTߙ | 50 | 98.0 |
| MRI‡ | 30 | 58.8 |
| Ultrasound | 42 | 82.4 |
| Nuclear medicine | 19 | 37.3 |
| PET§ | 16 | 31.4 |
| Interventional radiology | 42 | 82.4 |
| Other | 6 | 11.8 |
- ߙ Computed Tomography.
- ‡ Magnetic Resonance Imaging.
- § Positron Emission Tomography.
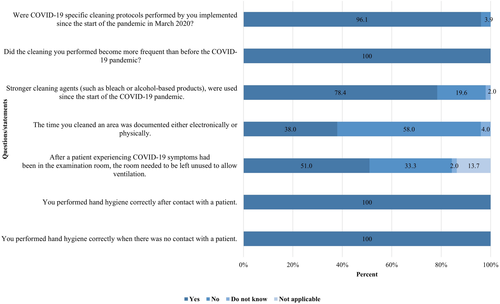
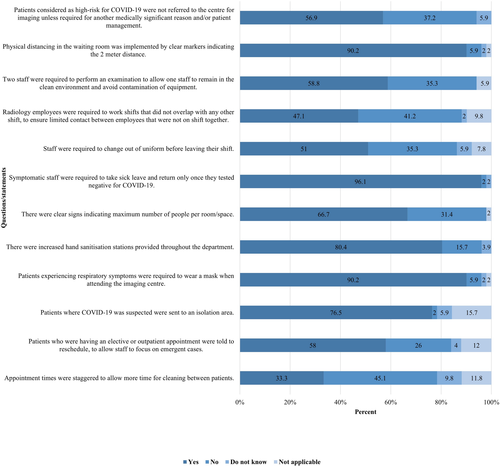
Infection control
Most respondents (48/51, 94.1%) stated ‘yes’ to their clinical practice being affected since the commencement of the COVID-19 pandemic, with multiple aspects of the practice being affected, including clinical environment (45/51, 88.2%) and patient interaction (34/51, 66.7%). The following areas of the practice were reported to be affected by fewer participants: physical and mental health (20/51, 39.2%), interaction among colleagues (17/51, 33.3%) and enthusiasm (17/51, 33.3%). Most participants (41/51, 80.4%) attributed these clinical practice changes to the protocols implemented to prevent the transmission of COVID-19, with 30 participants (58.8%) agreeing that their roles in the workplace had changed to accommodate more tasks specific for COVID-19 infection control. Figures 1-3 demonstrate the survey findings regarding the implementation of COVID-19-specific infection control procedures in medical imaging practice and workplace. The ‘not applicable’ option was available for centres that did not encounter high-risk COVID-19 cases. Figure 1 illustrates that most participants (74.5%) agreed with the listed PPE required to handle high-risk COVID-19 cases. However, there was a statistically significant difference among the workplace groups (P = 0.001).
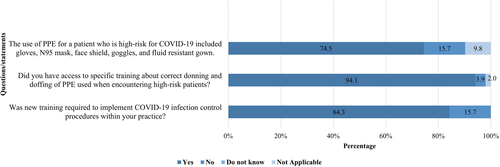
- ‘Initially, there was lack of direction, lack of coordinated information … all that did was create angst and a general distrust in the important people’. (50)
- ‘…lack of training on appropriate PPE usage’. (14)
- ‘…very few negative pressure rooms’. (15)
The participants' responses to changes in shift structure were significantly different among the workplace types (P < 0.001), and so were the responses to being required to change out of uniform before leaving their shift (P < 0.001). Furthermore, a statistically significant difference was noted among the workplace types in the response to requiring two staff members to perform high-risk examinations (P = 0.011). Analysis of the remaining infection control procedure questions did not reveal statistically significant differences among the groups.
Imaging volume
Sixty-one percent of the respondents reported an increase in demand for portable imaging, and the perceived increase depended on the workplace type (P < 0.001). Furthermore, 80% (4/5) of the private hospital group and 72.2% (26/36) of the public hospital group reported this increase, whereas only 10% (1/10) of the private practice group stated so. The respondents also provided their perceptions regarding the decrease in volume across several modalities, and the results are illustrated in Figure 4.
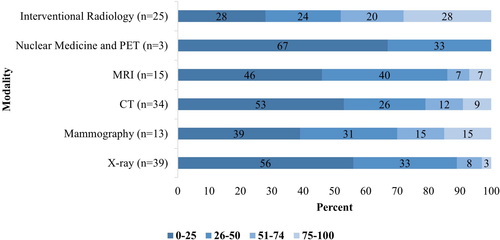
Table 2 lists the results from the independent samples t-test. The table highlights that an association was observed only between workplace type and interventional radiology (P = 0.006).
| Modality | Mean percentage decrease | Std Deviation | Std Error Mean | P-value | Cohen's d |
|---|---|---|---|---|---|
| X-ray | 22.889 | 14.190 | 4.730 | 0.376 | 0.273 |
| Mammography | 23.000 | 23.388 | 13.503 | 0.282 | 0.750 |
| CT ߙ | 22.500 | 14.000 | 4.950 | 0.168 | 0.420 |
| MRI‡ | 39.000 | 32.047 | 18.502 | 0.651 | −0.464 |
| Nuclear Medicine and PET§ | 50.000 | - | - | 0.000* | −22.863 |
| Interventional Radiology | 58.850 | 32.527 | 7.273 | 0.006* | 1.385 |
- Same abbreviations as shown in Table 1. *Significant at P < 0.05.
Workplace preparedness
Table 3 presents the participants' responses to the survey questions related to workplace preparedness. The participants' comments for these questions and the thematic analysis identified the following four themes: the prolonged nature of the COVID-19-specific protocols, increased physical demand, little or no support for the professionals and lack of supplies.
| Option question | Yes | No | Do not know | |||
|---|---|---|---|---|---|---|
| Freq | % | Freq | % | Freq | % | |
| Infection control procedures will remain? | 34 | 66.7 | 10 | 19.6 | 7 | 13.7 |
| Negative impact to physical and mental health? | 23 | 45.1 | 27 | 52.9 | 1 | 2.0 |
| Risk of infection has a negative impact to mental health? | 17 | 33.3 | 34 | 66.7 | 0 | 0 |
| More psychological support should have been provided? | 11 | 21.6 | 28 | 54.9 | 12 | 23.5 |
| WA healthcare system was prepared? | 8 | 15.7 | 39 | 76.5 | 4 | 7.8 |
| Your workplace was prepared? | 15 | 29.4 | 33 | 64.7 | 3 | 5.9 |
- ‘I'm not sure how to answer this as the pandemic will never be “over” as such’. (27)
- ‘There are some occasions where the shift is more stressful and strenuous because of spending extended time in PPE and performing X-ray examinations solo’. (29)
- ‘Wearing PPE is quite taxing on the body, especially breathing (i.e. wearing a well-fitted mask), and I could see that my interactions with the patients are not as effective/positive…’ (45)
- ‘More work to be done, mostly tedious cleaning regimes’. (50)
- ‘There was no mental support available as a radiographer’. (10)
- ‘Since there was zero support … a lot more could have been done’. (50)
- ‘There was a lack of PPE in the initial phase, which impacted the workflow. Once this was sourced, the system coped well’. (6)
- ‘More staff, more PPE, better mental health support’. (14)
- ‘Not enough cleaning agents and too few masks’. (47)
Discussion
To the best of our understanding, this is the first report on the perceptions of WA MIPs regarding the impact of COVID-19 on their practice and workplace. Previous studies have utilised surveys, interviews and field observations to investigate the impacts of COVID-19 on medical imaging centres.2, 8-10, 15-17 The results from this study provide valuable insights into the perceived impact of COVID-19 on MIPs. Three key areas were explored, namely, infection control, imaging volume and workplace preparedness, which have been discussed in the following sections.
Infection control
In Australia, it is the responsibility of the registered MIPs to adopt infection control procedures as mandated by the MRPBA; hence, it is interesting that only 80.4% (41/51) of the participants agreed to implementing COVID-19-specific cleaning protocols in their practice.12 This discrepancy could be because of the fact that some centres had protocols in place that minimised their services to patients who were considered to be at a high risk for COVID-19. The participants stated that such patients were not referred to their centre for imaging-based diagnosis unless required for other medically significant indications. This protocol meets the World Health Organisation's (WHO) guidelines for chest imaging.29 However, it is important to note that given it is known the virus can present asymptomatic, the risk of infection transmission within any centre is present, and it is important that all MIPs implement infection control procedures within their practice.1, 19 This finding indicates that further training is required to establish these cleaning protocols and the importance of them in all areas of medical imaging practice.
The QLD study suggests that isolation rooms and/or ‘no-waiting rooms’ be established in medical imaging centres where patients exhibiting respiratory symptoms could wait so as to reduce their contact with the waiting room environment.16, 17 Interestingly, in this study, the participants responded that whether the patients suspected to have COVID-19 were sent to an isolation area was dependent on the workplace type. There was a significant difference (P = 0.002) between the hospital groups, which agreed to the use of these rooms, and the private practice group, which found the use of these rooms ‘not applicable’. This finding is expected as hospitals have access to isolation areas designed specifically for patients with contagious respiratory conditions, whereas private practice generally does not have or need this facility.30 Inconsistencies in isolation facilities across centres in WA could pose a potential infection risk, and efforts are needed to determine whether isolation room use is warranted in WA medical imaging centres15-17.
The management of patients considered to be at a high risk for COVID-19 involves stringent adherence to PPE protocols and requirements.2, 29 According to the guidelines laid down by the WHO, the following should be used in such cases: gloves, N95 mask, face shield, goggles and fluid-resistant gown.29 The findings of this study and other Australian studies indicate that Australian MIPs follow this guideline; nevertheless, a significant difference was noted among the workplace types covered in this study (P = 0.001).15-17 While 79% (27/34) of the public hospital group and all (5/5) of the private hospital group agreed to the PPE listed, only half (5/10) of the private practice group agreed to it, which implies that PPE use is dependent upon workplace type. This inconsistency observed in WA workplaces may not be present in other states as they have experienced more COVID-19 cases, thereby necessitating the quick tightening of their infection control procedures.15-18 Furthermore, inadequate training may be the cause for inconsistencies because despite most participants (48/51, 94.1%) stating that they had access to PPE training, in the comments, they expressed that there was a ‘…lack of training on appropriate PPE usage’ (14) to perform their role safely. This highlights that although the training was available to participants, it was either unclear, insufficient and/or they were unable to retain the necessary information. Further investigation into the training methods may be necessary to identify how important COVID-19 information can be delivered effectively to MIPs.
Imaging volume
It is important to note that in this study, the imaging volume is an assessment of the participants' perception of changes and not the exact numerical changes. The perception of imaging volume changes is important to identify the modalities in which the MIPs experience increased pressure and in understanding whether this pressure is due to increased volume or the implementation of COVID-19 infection control procedures. An American study has suggested that imaging volumes have changed since the commencement of the COVID-19 pandemic. There has been an overall decrease (28%) across the modalities, with X-ray being the least impacted.6 Australian studies have indicated that the highest (80.1%) pressure is on portable imaging, and the results from the present study agree with this finding.15, 16 This observation is consistent with the recommendations of WHO that portable imaging is performed to reduce the movement of high-risk patients in medical imaging centres.30 However, this study noted a significant difference (P < 0.001) among the workplace types, with the private practice group experiencing the least change. This result could be ascribed to the fact that portable imaging is not often performed in private practice. The participants could not perceive a change because the service was not offered by them.2
The results of this study also reveal a statistically significant difference among the workplace types for interventional radiology, which suggests that the decrease in the imaging volume for this modality depends on the workplace of the respondent. The imaging volume decrease for interventional radiology based on the workplace type is expected as the medical urgency of procedures differs in accordance with the workplace.7 It is important to note that most participants (48/51, 94.1%) selected ‘not applicable’ for nuclear medicine (NM) and positron emission tomography (PET); hence, the result obtained for this modality may not be a true representation of the scenario. NM and PET are specialised imaging modalities and are not offered in all medical imaging centres.
Workplace preparedness
There has been a discussion in both academic literature and the media as to whether the WA healthcare system was well prepared to handle the COVID-19 pandemic. 2, 8-10, 15-17 An area of particular concern among the healthcare professionals in the initial months of the pandemic was access to PPE.2 The QLD study suggests that access to adequate PPE was limited during the initial 6 months of the pandemic, with the supplies improving over time.16 Shanahan and Akudjedu15 have reported contradictory results, with the participants stating that they had adequate PPE to perform their job safely. Another Australian study involving doctors, nurses and paramedics found that approximately half of the participants felt that they had adequate PPE supplies to perform their job safely; however, they felt that if the situation escalated, the supplies would be insufficient.31 The results of this study agree with those from the QLD study, according to which the healthcare system in WA and individual workplaces were not adequately prepared for the pandemic.16 It is clear that the WA healthcare system struggled in the initial phases of the pandemic during which there had been no stockpiling of PPE; however, the system was able to develop sustainable practices as the pandemic continued.19 The research by Shanahan and Akudjedu15 comprised a study sample that lacked the WA perspective, and the findings highlighted the need for studies exploring the impact of COVID-19 specifically in WA medical imaging centres.15, 31
Various investigations have examined the impact of COVID-19 on the workload of healthcare professionals, and the findings have suggested increased workload since the start of the pandemic.2, 15, 22, 23, 32 Interestingly, 54% of the participants in this study stated ‘no’ to being negatively impacted; however, the remaining participants and some of those who stated ‘no’ expressed an increased physical demand because of working extended hours, staff shortages and increased PPE use in their comments. Additionally, the participants opined that wearing PPE was ‘quite taxing on the body, especially breathing’ and that their ‘interaction with patients was not as effective/positive’ (45). These findings are consistent with those of Lewis and Mulla22 and demonstrate that although the COVID-19 infection control procedures are essential to achieve infection control, there are perceived impacts on the quality of care and the practitioner's health.15, 29, 32 This finding is of particular importance as the participants perceived that the protocols implemented in response to the pandemic will remain for a prolonged duration, with opinions that the pandemic ‘…will never be “over” as such’ (27).
The increased workload has raised questions about whether more support is required for the healthcare professionals at the frontline of the COVID-19 pandemic.2, 15, 23, 32 In this regard, 55% of the participants responded ‘no’ to believing that they required additional support; nevertheless, their comments suggested that support was not available when needed. In the study by Shanahan and Akudjedu,15 54.3% of the participants agreed that adequate psychosocial support structures were available, including redeployment, daily communication and virtual morning teas. However, none of the participants in the present study stated that these structures existed in WA. Hence, due consideration should be given to what kind of psychological services are available to MIPs in WA and how accessible these services are to the professionals.32
It is recommended that the impact of the new procedures on the professionals' ability to practice should be investigated. Moreover, how support can be offered to minimise the uncertainty of the professionals must be examined. Relevant improvements are needed to ensure that the physical and psychological safety of MIPs is maintained in the pandemic environment, starting with the provision of adequate access to the necessary supplies and support.
Limitations and further studies
This study has some limitations that need to be addressed. Firstly, with a 95% confidence interval and 13.5% margin of error, the sample size for this study was 51. This low response rate (17.1%) means that the results may not be inclusive of all perspectives and limits generalisability of the findings. The low response rate could be attributed to the difficult nature of the period during which the survey was conducted. The response would have been better if the timeframe for survey completion had been extended.19, 20 Second, to maintain a high level of anonymity, the location of the participants' workplace was not recorded, which means that whether the participants were located rurally or within the metropolitan area was unknown. As there are geographical variations in the severity of the COVID-19 situation, a comparison between rural and metropolitan groups could have been made.18 Further research investigating these differences is recommended. Third, the recorded data were self-reported and signify the perceptions of the participants.19, 20 The data may not reflect the actual volume changes during the pandemic, which is an area for further research.
Conclusion
This study explored the perceived impact of the COVID-19 pandemic on the practice of WA MIPs and the changes implemented within the workplace. The results demonstrate that WA MIPs have experienced an increased workload due to more cleaning procedures and changes in routine imaging, with the impact varying depending on the workplace. This study has provided insight into the WA experience with the COVID-19 pandemic, highlighting areas of concern for MIPs, such as PPE shortages and limited professional support. Medical imaging centres throughout WA should not only continue to refine their infection control procedures in response to the latest health advice but also attempt to improve the accessibility and availability of support to their staff.
Acknowledgements
The authors thank Mrs Anne D'Arcy-Warmington for assistance with the data analysis, Mr Gil Stevenson for advice on questionnaire construction and pilot testing and all the medical imaging professionals who participated in this project during the COVID-19 pandemic.
Conflict of Interest
The authors declare no conflict of interest.