Leksell Gamma Knife® – The first 1000 patients from the radiation therapist’s perspective
Correspondence
Michael Jenkins, 199 Ipswich road Woolloongabba 4102 Queensland, Australia. Tel: 3176 2695;
E-mail: [email protected]
Abstract
The Princess Alexandra Hospital (PAH) Gamma Knife® Centre of Queensland (GKCoQ) began operations in October of 2015 as a sub-specialty located within a larger radiation oncology service at PAH. It is uniquely positioned as the only Leksell Gamma Knife® (LGK) treatment unit available in the public hospital system in Australia, and the first and only service in Queensland. The GKCoQ treated the 1000th patient on 23 January 2019.
LGK is a non-invasive alternative to neurosurgery which uses radioactive cobalt sources to treat a variety of intracranial conditions ranging from tumours and metastases to functional disorders. It is a platform for stereotactic radiosurgery, a highly precise form of radiotherapy utilising very high doses to the target while maximally sparing surrounding normal brain. LGK enables patient planning and treatment to be done in one day as an outpatient procedure. This paper will outline our LGK service and provide insight into the expanded role that radiation therapists have within the multidisciplinary team required to deliver radiosurgery in a timely manner. The training programme and radiation licensing pathway that have been established for radiation therapists will also be described.
Introduction
Stereotactic radiosurgery (SRS) is a non-surgical highly precise form of radiation therapy that is used to treat various brain conditions including malignant and benign tumours, vascular and functional disorders. The biggest benefits for patients are that treatment involves less risk of complications, less side effects and a reduced impact on quality of life.1
The intracranial SRS programme began in August 2012 at Radiation Oncology, Princess Alexandra Hospital (PAH). The department is equipped with 5 linear accelerators and 2 computed tomography (CT) simulators. An Elekta Axesse linear accelerator fitted with a HexaPOD™ evo RT system (Elekta A.B., Stockholm, Sweden) and fully integrated ExacTrac including iPlan software (BrainLAB, Feldkirchen, Germany) was used to deliver these highly specialised treatments. As demonstrated in Figure 1, the intracranial SRS programme underwent rapid expansion in its first four years of operation.
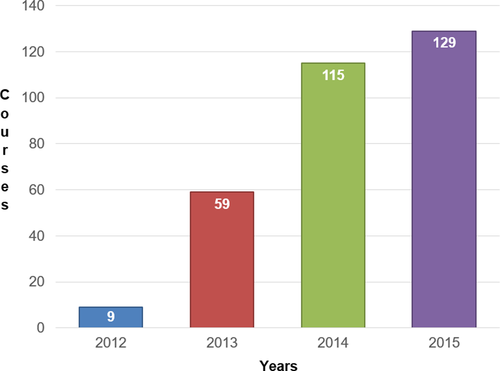
To accommodate this rapid expansion, the decision was made to acquire a Leksell Gamma Knife® (LGK) Perfexion unit (Elekta AB, Stockholm, Sweden) as a dedicated intracranial SRS platform.2 The Gamma Knife® Centre of Queensland (GKCoQ) was established as a state-wide service and commenced treatment on 26 October 2015. GKCoQ is located within Radiation Oncology PAH in a sixth bunker. At the time of establishing the GKCoQ, the department had a well-established linear accelerator-based stereotactic radiation therapy programme having treated approximately 500 intracranial and extracranial patients.
LGK is an established platform for treating intracranial targets. The LGK unit houses 192 cobalt-60 sources arranged in 8 sectors of 24 sources. These sources all converge at the isocentre to create complex treatment plans with a high degree of conformity delivered with submillimetre accuracy. The LGK precisely delivers dose with submillimetre accuracy, with a superior ability at limiting dose to healthy brain tissue.3-5
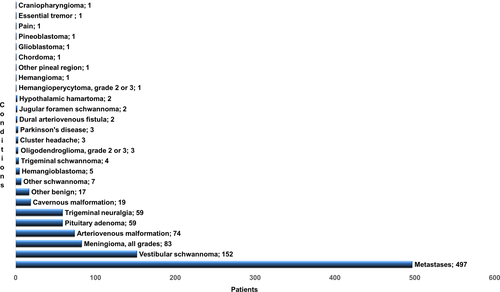
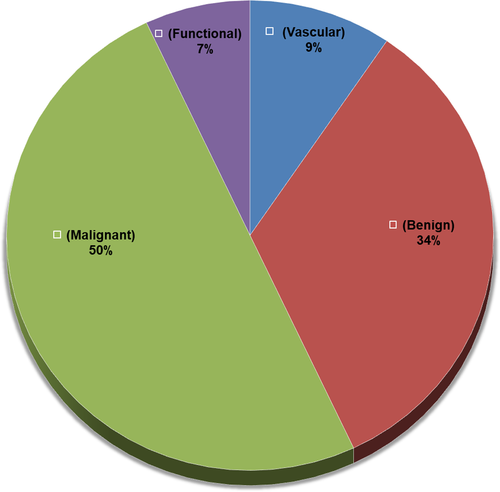
The GKCoQ service initially treated patients two days per week, but within three months this was increased to three days per week due to increasing demand. Initial estimates included the treatment of 100 patients in the first year and 250 in subsequent years. However, 100 patients were treated in the first six months (60 benign and 40 malignant diseases). Consequently, the service expanded to five days a week by June 2018. On the 23rd of January 2019, the GKCoQ treated the 1000th patient and these patients include a range of malignant, benign, vascular and functional neurosurgical conditions (Figures 2 and 3).
To successfully deliver the service, a multidisciplinary team including radiation oncologists (RO), neurosurgeons, neuroradiologists, radiation therapists (RT), radiation oncology medical physicists, nurses and diagnostic radiographers was formed. The unique role that was established for the RT within this model of care and associated patient clinical pathway as well as the supporting training programme and radiation licensing pathway that have been developed will be described. Ethics exemption was received.
Patient Clinical Pathway
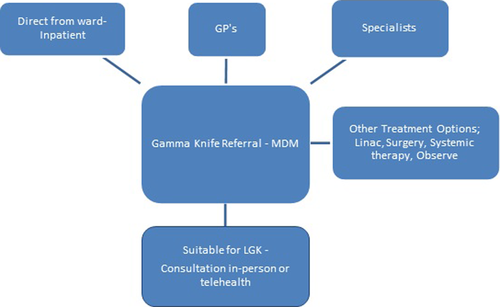
Patients are reviewed at a Gamma Knife Multidisciplinary Meeting (GKMDM) after referral to the GKCoQ from specialists and general practitioners. At this meeting, each patient’s history and imaging is evaluated and then a decision on an optimal patient pathway is determined (Figure 4). If LGK treatment is suitable, the patient attends an outpatient appointment at the PAH. This consultation can be carried out either in-person or via video-conference/telehealth to reduce the logistical burden on patients.
RT Role in Patient Treatment Workflow
Internationally, LGK centres generally consist of a standard treating team that includes a neurosurgeon and RO, working alongside a medical physicist and relevant nursing support. At the GKCoQ, our RT team are performing a unique role that is central to the progression of the patient through the treatment journey.
The treatment workflow for a LGK patient undergoing frame-based SRS is outlined in Figure 5. The RT is required to utilise a range of skills to manoeuvre a patient through all the technical steps essential to delivering LGK treatment. RTs play a key role in each step of the workflow to ensure the patient’s treatment path is as smooth and efficient as possible.
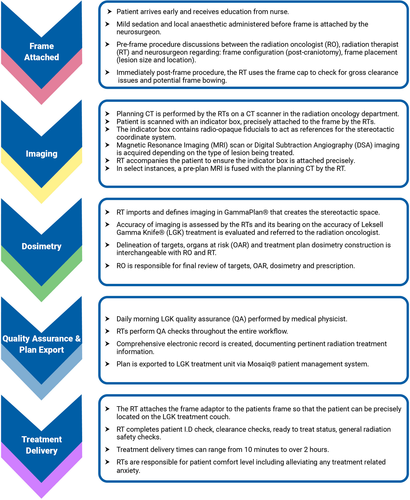
At the outset of the workflow, the RO and RT have discussions with the neurosurgeon regarding optimal frame placement for the patient’s lesion/s and location/s. The RTs are responsible for performing the spatial frame measurements and quality assurance (QA) checks to ensure the target location will be accommodated within the collimator cap to facilitate treatment delivery.
The RTs are responsible for the two-step process required to localise the stereotactic space. The first step is at pre-treatment imaging, which is used for target delineation and localisation, and dosimetry. The RTs are responsible for ensuring the indicator box used to create the stereotactic coordinates or space is aligned correctly. This could be performed at the patient’s computed tomography (CT), magnetic resonance imaging (MRI) or digital subtraction angiography (DSA) appointment/s. The second step is to import the acquired images into GammaPlan®. The RTs are responsible for the correct importation of images into GammaPlan®, and then, they perform what is termed image definition where the fiducials on the indicator box on each image are defined. This process creates the stereotactic space to ensure accurate treatment field (also referred to as shot) placement. Throughout these steps, the RTs are also performing image QA to detect if there have been any spatial distortions or frame shifts between images. The RTs working at LGK require a high-level understanding of the imaging used and can translate that knowledge to assess imaging factors which have a bearing on the accuracy of LGK treatment.
The ROs are responsible for the final dosimetry. To facilitate workflow efficiency, the RTs are able to perform contouring and generate a preliminary plan that can be finalised by the RO. Therefore, the RT must develop and maintain high-level skills in the use of the planning system to achieve the RO requirements.
The RTs have developed and maintained a comprehensive QA programme for the treatment workflow of the LGK patient. This includes a successful integration of MOSAIQ® and LGK where vital LGK treatment plan and beam information is reliably transferred to the MOSAIQ® patient record. The RTs have also developed multifaceted problem solving/ trouble shooting skills, becoming a resource to assist ROs and neurosurgeons in technical aspects of LGK in order to progress patients to treatment.
Training and Credentialing
In recognition of this extended scope RT role, only a small specialised group of four RTs were initially dedicated to the implementation of the LGK service.
During the implementation phase, RTs attended specialised vendor international training courses designed to equip staff with the necessary skills to operate the LGK. The RTs developed a detailed plan of the clinical workflow process that was used to help define the roles and responsibilities of each group.
- Safely docking and undocking the patient from the treatment unit, including patient identification and safe handling of equipment, and patient safety.
- Thorough understanding of emergency procedures required in the event of equipment failure or patient distress.
- Quality checks required for frame-based immobilisation.
- Understanding and assessment of imaging factors which have a bearing on the accuracy of LGK treatment. Such as image guidance, image co-registration assessment, immobilisation and fractionated treatment delivery.
- High-level skills in the specific requirements of the planning system to achieve the RO requirements.
- Acceptance of plan adaptations and replans.
- Understanding the flexibility of workflows and how they apply to the appropriate clinical situation.
- Use of the electronic prescription process and treatment delivery records.
In addition to the departmental training and competency programme, LGK RTs must also apply for the appropriate radiation licence. The law requires any person who uses a radiation source for therapeutic purposes must hold a use licence issued under the Radiation Safety Act 1999.6 The RT requires an amendment to the use licence that includes ‘Leksell Gamma Knife sealed source apparatus’ as an additional radiation source. For this amendment to take place, the RT initially holds a provisional use licence to work in LGK. The RT can apply for a full LGK licence once they have completed the previously described training and competency programme and the supervising LGK licensed RT is satisfied that the RT has a thorough comprehension of the radiation safety and clinical elements required to safely deliver LGK treatments.
RTs in the LGK team rotate into the LGK unit every 3 to 6 months to ensure skills are maintained to the high standard required.
Future directions
Currently, the PAH has a total of 65 full-time equivalent RTs. We have a specialised group consisting of 8 RTs that rotate through the LGK with 3 RTs rostered at LGK for any given time. The Assistant Director RT oversees and contributes to the day-to-day operations of the service. With increasing demands of the service, including departmental resources, the RTs will continue to play a pivotal role in the ongoing success of GKCoQ.
In May 2018, the LGK was upgraded to a Leksell Gamma Knife® Icon.7 The upgrade included integrated stereotactic cone beam CT, high definition motion management system and online dose evaluation. The Icon upgrade has facilitated increased flexibility within the intracranial radiosurgery patient workflow allowing for frame-based or frameless, image guided or fiducial-based, single-session or fractionated treatments. This upgrade has led to a considerable increase in the number of patients treated in LGK. We have treated over 550 patients in 2019 and expect these numbers to continue in future years.
The Icon upgrade has further expanded the RT role with the addition of traditional RT skills such as image guidance, image co-registration assessment and mask-based immobilisation. New skills have also been acquired such as acceptance of online plan adaptations in real time. The RT small-scale project management skills have been further enhanced due to the increased flexibility of available processes associated with the Icon upgrade.
We have reported on the novel and successful implementation of RTs as an integral and essential component to the delivery of LGK radiosurgery. This report highlights the specialised training and credentialing needed to become proficient in this extended scope role.
Acknowledgements
The authors wish to acknowledge the important contribution of the Gamma Knife Radiation Therapist team, the Medical Imaging Department and Dr Michael D Huo and also wish to acknowledge Gary Reichert who was the benefactor for the Icon upgrade.