Portal-Vein Compression Caused by Double-Pigtail Plastic Biliary Stent
Funding: The authors received no specific funding for this work.
ABSTRACT
Introduction
Reports of pseudoaneurysms associated with biliary self-expandable metallic stent (SEMS) placement have been increasing. Recently, cases of hepatic pseudoaneurysm rupture caused by double pigtail plastic stents (DPS) have also been reported. The symptoms of pseudoaneurysms are often non-specific, and many cases are diagnosed only after rupture. Therefore, early detection and appropriate treatment are required.
Case Presentation
A 45-year-old woman presented with obstructive jaundice caused by pancreatic head cancer, with imaging revealing common bile duct stenosis and intrahepatic bile duct dilation. Endoscopic retrograde cholangiopancreatography (ERCP) was performed to place a DPS in the left hepatic duct, relieving jaundice. However, follow-up contrast-enhanced computed tomography (CE-CT) revealed differences in arterial-phase blood flow between the liver lobes without reduction in portal vein blood flow. Therefore, the compression and stenosis of the left branch of the portal vein caused by the DPS were clearly identified using three-dimensional computed tomography (3D-CT). The DPS was replaced with a straight-type stent, preventing further complications. The patient subsequently underwent successful pancreaticoduodenectomy without any surgical complications.
Conclusion
This is a case of portal vein compression caused by double-pigtail plastic biliary stent. By promptly recognizing the differences in arterial-phase blood flow between the liver lobes and replacing the DPS with a straight-type plastic stent, complications, such as portal vein pseudoaneurysm formation, rupture, embolism, or thrombosis, were successfully avoided.
1 Introduction
Reports of pseudoaneurysms associated with biliary self-expandable metallic stent (SEMS) placement have been increasing. However, the symptoms of pseudoaneurysms are often non-specific, and many cases are diagnosed only after rupture. Recently, cases of hepatic pseudoaneurysm rupture caused by double pigtail plastic stents (DPS) have also been reported [1]. Here, we present a case of portal vein compression following DPS placement for bile duct stenosis secondary to pancreatic cancer.
2 Case Report
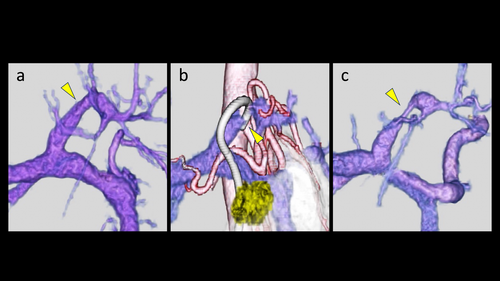
A 45-year-old woman was referred to our hospital for jaundice. Laboratory tests revealed elevated biliary enzymes and bilirubin levels with a direct-predominant pattern. A coronal section of contrast-enhanced computed tomography (CE-CT) demonstrated common bile duct stenosis caused by pancreatic head cancer, along with dilation of the intrahepatic bile ducts (Figure 1a). At that time, a three-dimensional computed tomography (3D-CT) showed no stenosis in the left branch of the portal vein (Figure 2a).
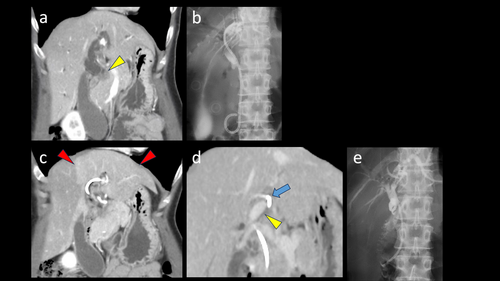
Endoscopic retrograde cholangiopancreatography (ERCP) was subsequently performed, and a 7-Fr × 7-cm double-pigtail plastic stent (DPS; Boston Scientific, Marlborough, MA, USA) was placed in the left hepatic duct (Figure 1b).
One month later, the obstructive jaundice had improved; however, an axial section of CE-CT revealed that the left lobe of the liver was primarily supplied by the left hepatic artery (Figure 1c). Coronal CE-CT and 3D-CT scans indicated that the proximal “pigtail” portion of the stent was compressing and obstructing the left branch of the portal vein (Figures 1d, 2b). At that time, the patient did not exhibit symptoms, such as abdominal pain, fever, or jaundice. Laboratory tests showed no abnormalities in bilirubin, bile duct enzymes, or inflammatory markers. Uniform enhancement of the left hepatic lobe in the arterial phase of CE-CT suggested that cholangitis due to stent obstruction was unlikely.
After ruling out other complications such as portal vein aneurysm, thrombosis, or embolism, ERCP was performed to replace the DPS with a 7-Fr × 7-cm straight-type stent (Olympus Co., Tokyo, Japan) (Figure 1e). Follow-up 3D-CT after stent replacement revealed persistent localized stenosis in the left portal vein (Figure 2c). By promptly replacing the stent, further complications were successfully avoided.
Two weeks later, the patient underwent a pancreaticoduodenectomy for pancreatic head cancer as scheduled, without any surgical complications.
3 Discussion
Reports of hepatic artery pseudoaneurysm formation and subsequent hemobilia caused by SEMS placement have been increasing. Additionally, cases of hemobilia resulting from portal vein pseudoaneurysm after SEMS placement have also been reported [2]. The mechanisms underlying hepatic pseudoaneurysm formation are thought to include vascular wall compression due to biliary stent placement, chronic biliary infections, and direct arterial invasion by malignant tumors [3-5]. SEMS are presumed to more readily compress blood vessels because of their greater thickness, hardness, and stronger axial force compared to plastic stents. Interestingly, recent reports have also described pseudoaneurysm formation associated with plastic stents [1, 6, 7].
In this case, while no reduction in portal vein blood flow was observed, differences in arterial-phase blood flow between the liver lobes were detected. This highlights the role of arterial-phase imaging in identifying early vascular changes caused by stent placement. The compression and stenosis of the left branch of the portal vein caused by the DPS in the left hepatic duct were clearly identified using 3D-CT. By promptly recognizing these changes and replacing the DPS with a straight-type plastic stent, complications, such as portal vein pseudoaneurysm formation, rupture, embolism, or thrombosis, were successfully avoided. Importantly, this intervention did not delay or interfere with the subsequent surgical management of pancreatic cancer.
The most common site for hepatic pseudoaneurysm formation during SEMS placement is the right hepatic artery [8]. However, when using a DPS, clinicians must consider that the position of the “pigtail” can influence the incidence and distribution of hepatic pseudoaneurysms. In the presented case, the sharp branching of the B3 bile duct and the proximity of the left portal vein branch to the bile duct are likely contributing factors. Proper stent positioning and timely intervention are critical to minimizing risks and ensuring successful patient outcomes.
Ethics Statement
The authors have nothing to report.
Consent
Consent obtained directly from the patient.
Conflicts of Interest
The authors declare no conflicts of interest.




