Attitudes of clinicians toward cardiac surgery and trisomy 18
Abstract
Trisomy 18 is an autosomal trisomy condition characterized by minor to major birth defects, severe disabilities, and high rates of pre- and postnatal mortality. Interventions for these infants have traditionally been withheld with focus instead on palliative support. The issues and attitudes surrounding corrective surgery of congenital heart defects, which is a birth defect that occurs in approximately 90% of infants with trisomy 18, is of our study's interest as recent literature has indicated that cardiac surgery is being performed and may lead to improved survival compared to palliative care. Thus, our study aimed to describe clinician attitudes toward cardiac surgery and trisomy 18. We surveyed 378 clinicians from multiple specialties, including genetic counselors, involved in the pre- and postnatal care of infants with trisomy 18. Descriptive statistics were performed to describe all clinicians' responses, and a secondary analysis with stratifications by clinician type was also performed. Forty-eight percent (n = 378) of clinicians felt it was appropriate to discuss the option of cardiac surgery. Ethical concerns and insufficient outcome data were the most agreed upon reasons for not offering cardiac surgery. Trisomy 18 not being uniformly lethal and expressed parental wishes were the most agreed upon justifications for offering surgery. Clinicians felt the discussion of the option of cardiac surgery is appropriate, however are hesitant due to ethical concerns and insufficient outcome data. Results from this study aim to promote discussion and collaboration among clinicians to improve consistency in patient care.
1 INTRODUCTION
Trisomy 18 (T-18) is an autosomal trisomy involving an extra copy of chromosome 18 with a prevalence of one in 3,000 to one in 8,000 live births. Children with T-18 have minor to major birth defects, severe psychomotor and cognitive disabilities, and an increased risk for pre- and postnatal mortality (Cereda & Carey, 2012; Embleton, Wyllie, Wright, Burn, & Hunter, 1996). Due to the presence of multiple anomalies, it is estimated that approximately 5%–10% of live born infants with T-18 live to the first year of life (Rasmussen, Wong, Yang, May, & Friedman, 2003). Medical care for infants with T-18 has traditionally been palliative care, focusing on symptom relief, control of pain, and limitation or withdrawal of life-sustaining medical treatment including surgical repair of birth defects, rather than aggressive measures (Care, 2000). However surgical repair of congenital heart defects (CHDs), found in approximately 90% of infants, is being considered and performed on infants with T-18. The majority of CHDs seen in infants with T-18 are ventricular septal defects (VSD), atrial septal defects (ASD), and patent arterial duct (PDA), defined in the literature as moderately complex heart defects. A minority of infants with T-18 have greatly complex heart defects such a hypoplastic left heart syndrome and transposition of the great arteries (Baty, Blackburn, & Carey, 1994; Bruns & Martinez, 2015; Kavarana, 2016; Van Dyke & Allen, 1990). Heart failure secondary to an unrepaired cardiac defect is considered one of the major causes of deaths in infants with T-18 along with respiratory failure or central apnea (Cereda & Carey, 2012; Embleton et al., 1996; Imai et al., 2015).
Justification for palliative care approaches over corrective cardiac surgery has been previously explored in the literature. Concerns raised included improper allocation of time and resources surgery, harm to infant during and after surgery, as well as ethical considerations including the quality of life after surgery, lack of data supporting improved prognosis, and the potential of providing false hope or unrealistic expectations for the families (Boss et al., 2013; Graham, 2016; Janvier, Farlow, & Wilfond, 2012; Janvier & Watkins, 2013). Despite these raised concerns, several studies in the last decade (Bruns & Martinez, 2015; Kaneko et al., 2008; Kobayashi, Kaneko, Yamamoto, Yoda, & Tsuchiya, 2010; Maeda et al., 2011; Yamagishi, 2010) have described outcomes following cardiac surgery on infants with T-18, most frequently on VSDs, ASDs, and PDAs. Two studies (Graham, Bradley, Shirali, Hills, & Atz, 2004; Yamagishi, 2010) published survival rates of infants with T-18 after undergoing cardiac surgery, reporting 45% 2-year survival and 86% hospital survival. One study (Costello et al., 2015) compared the outcomes of those infants with T-18 who underwent cardiac surgery versus those who had palliative care and concluded that cardiac surgery should be considered for all infants with T-18 who have moderately complex heart defects. While there are published recommendations regarding the importance of conversations between clinicians and families regarding the option of cardiac surgery (Janvier, Farlow, & Barrington, 2016), there is an overall lack of consensus in the literature on recommendations for corrective cardiac surgery versus palliative approaches for moderately complex heart defects (Costello et al., 2015; Graham et al., 2004). While corrective cardiac surgery may potentially help negate cardiac-related death and may improve the survival length, some argue that more data demonstrating clinical benefit of corrective cardiac surgery is needed before generalizations can be made on effectiveness (Graham, 2016; Kaneko et al., 2009; Kobayashi et al., 2010; Maeda et al., 2011; Muneuchi et al., 2011). Furthermore, it is important to carefully consider the limitations of the data available on the survival statistics of infants who undergo cardiac surgery including potential confounders such as selection bias as those undergoing surgery are most often less severely affected. Due to complexities surrounding this decision for clinicians and families, it may be unrealistic that a generalized approach to care will exist, as each infant with T-18 and family will need to be considered on an individual basis and not grouped into a syndrome or diagnosis (Andrews et al., 2016; Carey, 2012; Janvier, Okah, Farlow, & Lantos, 2011; Kavarana, 2016; Muneuchi et al., 2011; Wingate et al., 2014).
Previous research has examined the attitudes of physicians regarding the care and management of infants with T-18. Two different studies on the opinions of neonatologists regarding infants with T-18 found that the expressed wishes of the parents largely drove the decision to perform neonatal resuscitation (Jacobs et al., 2016; McGraw & Perlman, 2008). Other studies support this, reporting that the majority of physicians of varying specialties reported that they were likely to respect parental autonomy regarding management decisions such as fetal monitoring and cesarean delivery in conditions such as T-18 rather than making management decisions based solely on the diagnosis itself (Heuser, Eller, & Byrne, 2012; Janvier et al., 2016; Wilkinson et al., 2014; Yates, Hoffman, Shepherd, Boettner, & McBride, 2011; Young, Simpson, & Warren, 2017). Although there are some consistencies among physicians, these and other studies (Hurley, Krishnan, Parton, & Dozor, 2014; Yates et al., 2011; Young et al., 2017) have further identified differences in opinions regarding care and management, including consideration of cardiac surgery, among and between specialties. This reinforces that there is not a uniformly accepted standard approach for the care of infants with T-18. Additional research is warranted to add to previously described clinicians' attitudes toward this controversial topic in the interest of improving understanding of clinical approach and promoting consistency (Andrews et al., 2016). This study is designed to explore why and how certain clinicians choose to incorporate the option of cardiac surgery into their discussion with families with a pre- or postnatal diagnosis of T-18, and why others do not.
2 METHODS
Clinicians in the following specialties were eligible for participation and were chosen due to their primary role of care: prenatal physicians (obstetrics and gynecologists [OBGYNs], maternal fetal medicine specialists [MFMs], and neonatologists), postnatal physicians (medical geneticists, cardiologists, and cardiac surgeons), and genetic counselors. This study was approved by the Institutional Review Board of the University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences (HSC-MS-16-0454). Genetic counselors and physicians were recruited via a survey link electronically distributed to members of the National Society of Genetic Counselors listserv and via membership of the North American Fetal Therapy Network, respectively. Physicians were also recruited through genetic counselors affiliated with fetal centers across the United States obtained from a list of fetal centers on the NSGC website. Genetic counselors disseminated the survey link by emails to the eligible physicians at their respective institutions. Lastly, additional physicians were recruited using snowball sampling in which physicians who were reached by the methods listed above were given approval to distribute the survey link to their colleagues in the eligible specialties who had not already been reached through the previously implemented data collection methods (Goodman, 1961). The study consent was present in the form of a letter of invitation and completion of survey was considered consent. Responses were collected from August 2016 to December 2016.
2.1 Study instrumentation
The survey consisted of questions regarding demographics, general questions about knowledge of and experience with patients with T-18, and clinicians' attitudes toward reasons against and for offering cardiac surgery for infants with T-18. It was explicitly stated that all survey questions pertained to non-mosaic T-18. Question formatting consisted of multiple choice, “agree” or “disagree,” and Likert scale questions on a scale of 1 (strongly disagree) to 5 (strongly agree) including the option of “neutral.” A formal validated measure was not used as survey questions were uniquely developed by the authors for the purpose of this study and were reviewed by clinicians in each of the specialties of interest.
2.2 Data analysis
Responses were managed using Qualtrics and were stored at the McGovern Medical School. STATA 13.1 (College Station, TX) statistical software was used for data analysis. Descriptive statistics were used to describe the results of all clinicians, while quantitative statistical comparisons were analyzed between the following clinician types: prenatal physicians (including OBGYNs and MFMs), postnatal physicians (including neonatologists, medical geneticists, cardiologists, and cardiac surgeons), and genetic counselors. This latter comparison of grouped clinicians was chosen based on the substantial number of genetic counselor respondents compared to other specialties to account for the difference in number of respondents. Since each question was optional and clinicians were not required to answer every question, sample sizes between questions differ slightly throughout if a clinician accidently or intentionally did not answer a question. Statistically significant relationships for Likert scale variables were determined by analyzing the three comparison groups using Kruskal–Wallis tests and between two groups using Mann–Whitney ranked sum tests. Categorical variables were compared using contingency tests (Fisher exact or Chi-square). A p-value of <0.05 was considered statistically significant.
3 RESULTS
A total of 429 clinicians participated in this survey. After excluding 51 clinicians who completed only the demographic section of the survey, analyses are based on 378 clinicians, including genetic counselors (253/378), prenatal physicians (75/378), and postnatal physicians (50/378). Survey respondent numbers differed per question as some questions were left unanswered. The majority of clinicians were female (323/375, 86%), non-Hispanic white (345/378, 91%) working in university-based hospital practices (218/375, 58%) or non-university based hospital practices (108/375, 29%). The majority (262/378, 69%) of clinicians reported they see 1–5 patients with T-18 per year. Of the clinicians who indicated they see at least one patient with T-18 on average per year, 51% (165/321) reported they discussed the option of cardiac surgery with at least one of their patients, while 46% (149/321) indicated they did not have the discussion with any of the patients with T-18. Please see Table 1 for additional demographic information.
| n(%) | |
|---|---|
| Age (n = 371) | |
| 18–34 | 188 (50) |
| 35–54 | 147 (40) |
| 55 or older | 36 (10) |
| Gender (n = 375) | |
| Female | 323 (86) |
| Male | 52 (14) |
| Ethnicity (n = 378) | |
| Non-Hispanic white | 345 (91) |
| Asian | 11 (3) |
| African American | 4 (1) |
| Other | 18 (5) |
| Region of the United States (n = 370) | |
| South | 114 (31) |
| Midwest | 98 (27) |
| West | 75 (20) |
| Northeast | 66 (18) |
| Other | 17 (4) |
| Setting of Practice (n = 375) | |
| University-based | 218 (58) |
| Non-University based | 108 (29) |
| Private practice | 30 (8) |
| Other | 19 (5) |
| Specialty (n = 378) | |
| Genetic counselors | 253 (67) |
| MFMsa | 72 (19) |
| Medical geneticistsb | 22 (6) |
| Neonatologistsb | 14 (4) |
| Cardiologistsb | 8 (2) |
| Cardiac surgeonsb | 6 (1) |
| Obstetricians and gynecologistsa | 3 (1) |
| Patients with T-18 seen (on average/year) (n = 378) | |
| None | 40 (11) |
| 1–5 | 262 (69) |
| 6–10 | 59 (16) |
| 11 or more | 15 (4) |
| Not sure | 2 (0) |
| Patients (on average/year) with a diagnosis of non-mosaic T-18 with whom cardiac surgery was discussed (n = 321) | |
| None | 149 (46) |
| 1–5 | 156 (49) |
| 6–10 | 5 (2) |
| 11 or more | 4 (1) |
| Not sure | 7 (2) |
- MFMs: maternal fetal medicine specialists; OBGYNs: obstetrics and gynecologists
- a Indicates prenatal physicians (n = 75).
- b Indicates postnatal physicians (n = 50).
3.1 General knowledge and attitudes toward T-18 and cardiac surgery
Nearly half of all clinicians (171/357, 48%) agreed that discussing the option of cardiac surgery is appropriate with 74% (127/171) of this group indicating they themselves discuss the option and/or refer the patient to cardiac surgery. Clinicians were asked about their attitudes toward the following terms being used to describe individuals with T-18: “vegetative,” “incompatible with life,” “lethal anomaly,” and “life-limiting.” Most clinicians disagreed with the use of “vegetative” (242/356, 68%), while across all specialties most clinicians agreed with the term “life-limiting” (332/357, 93%). When stratified by clinician type, prenatal physicians were more likely to agree with use of “incompatible with life” (38/73, 52%) compared to postnatal physicians (14/48, 29%) and genetic counselors (75/235,32%) (p = 0.02).
Over half of all clinicians agreed with the following potential end benefits of cardiac surgery: parental autonomy is respected (314/345, 91%), potential extension of time with the infant (279/344, 81%), and the potential for improved quality of life (173/339, 51%). Thirty-seven percent (128/345) of clinicians felt there was no end benefit in performing cardiac surgery. When stratified by clinician type, prenatal physicians (44/75, 58%) were more likely to agree that cardiac surgery has “no end benefit” (p < 0.001) and disagree that cardiac surgery has the potential to extend time with the infant (28/75, 37%, p < 0.001) and could potentially improve the infant's quality of life (51/75, 68%, p = 0.01). Thirty percent (86/287) of clinicians reported their current approach with patients includes discussing cardiac surgery if brought up by parents, emphasizing it may be an option, and providing a referral to cardiac surgery, while 28% (83/295) indicated their current approach includes discussing if brought up by parents but emphasizing surgery is discouraged.
3.2 Attitudes regarding offering cardiac surgery
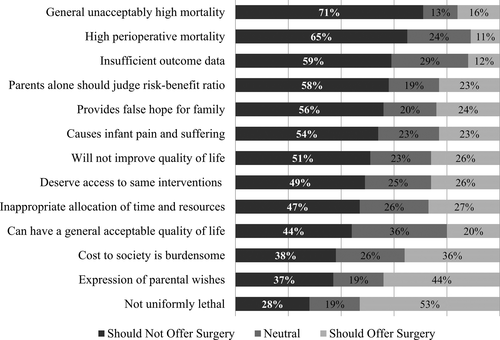
Over half of all clinicians agreed with the following reasons as justifications to not offer cardiac surgery for infants with T-18: condition has a general unacceptably high mortality (253/356, 71%), high-perioperative mortality (231/355, 65%), insufficient outcome data on risks and benefits of surgery (210/356, 59%), parents alone should judge risk-benefit ratio of surgery (201/347, 58%), provides false hope for the family (198/354, 56%), causes infant pain and suffering (192/355, 54%), and surgery will not improve the infant's quality of life (181/355, 51%) (Figure 1). When clinicians were asked about societal costs of cardiac surgery for these infants, 47% (167/355) agreed that surgery should not be offered due to an inappropriate allocation of the institution's time and resources and 38% (133/350) agreed that the cost of surgery to society is burdensome. Overall when stratified by clinician type, differences existed between prenatal physicians, postnatal physicians, and genetic counselors for all provided considerations regarding cardiac surgery with the exception of insufficient outcome data, the risks and benefits of surgery, parents alone should judge the risk-benefit of surgery, and surgery causes the infant pain and suffering. Please see Table 2 for additional information.
| Considerations surrounding offering cardiac surgery | Should not offer surgery (%) | Neutral (%) | Should offer surgery (%) |
|---|---|---|---|
| *General unacceptably high mortality (p < 0.001) | |||
| Prenatal physicians (n = 72) | 85 | 5 | 10 |
| Postnatal physicians (n = 48) | 54 | 17 | 29 |
| Genetic counselors (n = 236) | 71 | 14 | 15 |
| *High perioperative mortality (p < 0.001) | |||
| Prenatal physicians (n = 72) | 64 | 32 | 4 |
| Postnatal physicians (n = 48) | 42 | 31 | 27 |
| Genetic counselors (n = 235) | 69 | 21 | 10 |
| Insufficient outcome data (p = 0.26) | |||
| Prenatal physicians (n = 72) | 50 | 43 | 7 |
| Postnatal physicians (n = 48) | 54 | 17 | 29 |
| Genetic counselors (n = 236) | 63 | 26 | 11 |
| Parents alone should judge risk-benefit ratio (p = 0.32) | |||
| Prenatal physicians (n = 70) | 64 | 13 | 23 |
| Postnatal physicians (n = 46) | 78 | 7 | 15 |
| Genetic counselors (n = 231) | 52 | 24 | 24 |
| *Provides false hope for family (p < 0.001) | |||
| Prenatal physicians (n = 72) | 67 | 18 | 15 |
| Postnatal physicians (n = 48) | 61 | 10 | 29 |
| Genetic counselors (n = 234) | 52 | 22 | 26 |
| Causes infant pain and suffering (p = 0.09) | |||
| Prenatal physicians (n = 71) | 62 | 20 | 18 |
| Postnatal physicians (n = 48) | 58 | 19 | 23 |
| Genetic counselors (n = 236) | 51 | 24 | 25 |
| *Will not improve quality of life (p = 0.02) | |||
| Prenatal physicians (n = 71) | 58 | 27 | 15 |
| Postnatal physicians (n = 48) | 54 | 19 | 27 |
| Genetic counselors (n = 236) | 48 | 22 | 30 |
| *Deserve access to same interventions (p < 0.001) | |||
| Prenatal physicians (n = 70) | 71 | 20 | 9 |
| Postnatal physicians (n = 45) | 67 | 13 | 20 |
| Genetic counselors (n = 231) | 39 | 29 | 32 |
| *Inappropriate allocation of time and resources (p < 0.001) | |||
| Prenatal physicians (n = 71) | 76 | 13 | 11 |
| Postnatal physicians (n = 48) | 32 | 33 | 35 |
| Genetic counselors (n = 236) | 42 | 28 | 30 |
| *Can have a general acceptable quality of life (p < 0.001) | |||
| Prenatal physicians (n = 70) | 62 | 34 | 4 |
| Postnatal physicians (n = 46) | 44 | 26 | 30 |
| Genetic counselors (n = 231) | 39 | 38 | 23 |
| *Cost to society is burdensome (p < 0.001) | |||
| Prenatal physicians (n = 72) | 68 | 18 | 14 |
| Postnatal physicians (n = 42) | 28 | 36 | 36 |
| Genetic counselors (n = 236) | 31 | 26 | 43 |
| *Expression of parental wishes (p = 0.03) | |||
| Prenatal physicians (n = 70) | 57 | 20 | 23 |
| Postnatal physicians (n = 46) | 59 | 19 | 22 |
| Genetic counselors (n = 231) | 27 | 18 | 55 |
| *Condition is not uniformly lethal (p = 0.01) | |||
| Prenatal physicians (n = 70) | 53 | 17 | 30 |
| Postnatal physicians (n = 46) | 37 | 26 | 37 |
| Genetic counselors (n = 231) | 19 | 18 | 63 |
- * indicates a statistically significant result (p < 0.05)
Fifty-three percent (184/347) of clinicians across all specialties agreed that T-18 not being uniformly lethal is a reason to offer cardiac surgery (Figure 1). This was the sole consideration in support of offering surgery upon which the majority of clinicians agreed. Of all clinicians, 44% (153/347) agreed that surgery should be offered if parents express their wish to have “everything done” for their child. When stratified into clinician type, genetic counselors were twice as likely to agree (127/231, 55%) with surgery being offered due expression of parental wishes compared to prenatal (16/70, 23%) and postnatal physicians (10/46, 22%) (p = 0.03). Overall 26% (90/346) of clinicians felt surgery should be offered because infants with T-18 deserve access to the same interventions as chromosomally typical infants compared to 49% (170/346) who disagreed. Twenty percent (69/347) of clinicians agreed that individuals with T-18 having an acceptable quality of life were a reason to offer cardiac surgery, while 36% (125/347) were neutral. Postnatal physicians and genetic counselors were more likely to agree (14/46, 30% and 54/231, 23%) with this statement regarding quality of life as a justification to offer surgery than prenatal physicians (3/70, 4%) (p < 0.001). Please see Table 2 for additional information.
3.3 Cardiac surgeon approaches to determining candidates for cardiac surgery
Four out of six cardiac surgeons reported they had performed cardiac surgery on at least one infant with T-18; the two cardiac surgeons who had not performed surgery indicated they would be willing to do so. The majority of cardiac surgeons indicated they would be willing to perform surgery on an infant with T-18 for the following heart defects: VSD (5/6), PDA (5/6), coarctation of the aorta (5/6), and ASD (4/6) while none indicated willingness to perform surgery on infants with T-18 and hypoplastic left heart syndrome. In an infant with T-18 with a heart defect described to be moderately complex, most cardiac surgeons were still willing to perform surgery in the presence of additional anomalies including clubfoot (5/6), polydactyly (5/6), and cleft lip with or without cleft palate (4/6). Fewer reported willingness to perform surgery as the severity of the anomaly increased, with no cardiac surgeons (0/6) willing to perform surgery with the additional finding of a diaphragmatic hernia.
4 DISCUSSION
The appropriateness of offering cardiac surgery to families of infants with T-18 is undoubtedly complex and has been met with a wide range of opinions in the literature. Our results suggest that nearly half of clinicians in our study feel it is appropriate to discuss the option of cardiac surgery with postnatal physicians and genetic counselors feeling it is more appropriate for this discussion to take place than prenatal physicians. Of clinicians who feel this discussion is appropriate, the vast majority are discussing the option of surgery and/or referring the patient to cardiac surgery for such a discussion to take place. This clinical approach of discussing cardiac surgery supports recent literature pointing to the fact that cardiac surgery for infants with T-18 is occurring more frequently than previously reported (Yates et al., 2011). Interestingly, a quarter of clinicians felt the discussion was appropriate, however indicated that they do not discuss the option of cardiac surgery. This suggests there may be barriers that clinicians experience regarding the discussion of cardiac surgery; however, these potential barriers that may exist were not formally explored in our study. Although participants' responses were not systematically analyzed, we note that several respondents mentioned lack of accessibility to willing surgeons in the free response section when expanding on why the option is not offered to their patients; exploration of this and other barriers is warranted through formal study. Overall, our study provides evidence that there are clinicians across multiple specialties who feel the discussion of cardiac surgery is appropriate and report actually having such discussions with families and referring them to cardiac surgery. Moreover, all cardiac surgeons in our study (n = 6) were willing to perform surgery on infants with T-18 depending on the clinical picture of the infant. While limitations exist with the data obtained by the cardiac surgeons in our study, understanding the willingness and conditions in which cardiac surgeons will perform surgery is another important aspect to this complex topic that further points to an evolving attitude.
The differing opinions among clinicians regarding the discussion of cardiac surgery are most notable in our study when comparing prenatal physicians to postnatal physicians and genetic counselors. Prenatal physicians were more likely to agree with the use of a less patient friendly term (incompatible with life) and reported less support of the discussion of the option of cardiac surgery when compared to postnatal physicians and genetic counselors. Moreover, prenatal physicians were more likely to consider surgery to have no end benefit and less likely to consider surgery may have the potential to extend time with the infant or improve the infant's quality of life. The differing clinician opinions regarding aspects of T-18 and appropriateness of cardiac surgery point to the importance of open communication among the specialties to ensure that clinicians are educated on how their colleagues are discussing this option with patients. Families should be provided with a thoroughly considered team approach based on this communication to allow for balanced and consistent counseling on the decisions surrounding cardiac surgery to avoid misunderstanding and potential mistrust (Janvier et al., 2012).
In our study, clinicians' attitudes were examined surrounding common themes that have emerged in previous literature on this topic (Boss et al., 2013; Graham, 2016; Janvier et al., 2016, 2012; Janvier & Watkins, 2013). While our study provides evidence that there is clinician support of the discussion of the option cardiac surgery, many clinicians expressed disagreement with offering cardiac surgery in light of the lack of outcome data and ethical principles such as nonmaleficence, beneficence, and justice. These findings support and further validate previous studies (Boss et al., 2013; Graham, 2016; Janvier et al., 2012) that have identified the same concerns and were unsurprising, as the ethical nature of such surgery is an important and recurrent topic in discussions between clinicians and families when deciding if cardiac surgery is appropriate (Janvier et al., 2016). Many hospitals offer access to an ethics committee consult, which may be warranted to aid in parsing out these complex ethical issues. Interestingly, previous studies (Graham, 2016; Janvier et al., 2011) have pointed to the societal burden of performing cardiac surgery for these infants as a clear reason against offering surgery; in contrast, the majority of clinicians in our study felt surgery should still be offered or were neutral regarding societal burdens.
Trisomy 18 not being uniformly lethal was the sole consideration for offering cardiac surgery upon which more than half of clinicians agreed. This finding is consistent with a notable shift in the literature emphasizing that T-18 should not be presented as a lethal anomaly in the counseling of families given the known survivability, which further emphasizes the importance of individualized care considerations for infants with T-18 (Association, 2006; Cereda & Carey, 2012; Koogler, Wilfond, & Ross, 2003). Previous studies (Jacobs et al., 2016; McGraw & Perlman, 2008) have suggested that parental autonomy impacts management decisions made by clinicians; however, the results of our study demonstrated mixed feelings toward parental involvement. Over half of clinicians in this study disagreed or were neutral regarding expressed parental wishes as a reason to offer cardiac surgery; however, the great majority of clinicians in our study felt that an end benefit to performing surgery is that parental autonomy is respected. This implies clinicians in our study indicated that parental autonomy may be considered a potential benefit of surgery, but not adequate alone a reason for the clinician to discuss the option of cardiac surgery alone.
Our study also aimed to describe cardiac surgeons' approaches to determining candidacy for cardiac surgery among infants with T-18. Due to the small number of cardiac surgeons who participated, we are unable to draw conclusions, but can comment generally on the responses received from the surgeons in our study. Overall, the cardiac surgeons who responded were most willing to perform surgery on moderately complex heart defects in the absence of additional anomalies or presence of additional anomalies associated with lower morbidity rates. Further, our study found that all cardiac surgeons who responded (n = 6) have either performed surgery or are willing to perform surgery, confirming that the option exists at the respective institutions of the cardiac surgeons in our study.
4.1 Study limitations
A major strength of this study is the examination of attitudes of both prenatal and postnatal clinicians. However, several limitations exist. The sampling of physicians through fetal centers may have led to attitudes mostly representative of physicians in medical centers and is not representative of physicians at large. Sample sizes for some of our physician groups were a limitation as well. The prenatal physician group consisted mostly of MFMs (n = 72) and few OBGYNs (n = 3). Therefore, the results of this study and the attitudes of the prenatal physicians should be interpreted to be mostly representative of MFMs and cannot be extrapolated to the attitudes of OBGYNs. The six cardiac surgeons who responded to our survey were located in either Texas (n = 4) or Missouri (n = 2). Therefore, the attitudes of the cardiac surgeons in our study cannot be extrapolated to be representative of the attitudes and opinions of cardiac surgeons in general. Another limitation is selection bias. The clinicians who participated in our study may be those who feel most strongly about this topic and may not represent the average clinician. Lastly, at times the term “cardiac intervention” was used in the survey which was intended to be synonymous with cardiac surgery; however, upon closer consideration could have been interpreted as palliative surgical interventions, such as pulmonary artery banding, as opposed to exclusively surgical repair (Yuan & Jing, 2009). Overall, we do not feel this discrepancy in wording heavily impacted the results and conclusions drawn from our study.
4.2 Research recommendations
While our study was able to capture a variety of pre- and postnatal clinicians that are involved in care of these infants, the opinions of other clinicians such as pediatricians, nurses, and social workers and others would be a valuable addition to the literature in an effort to obtained inclusive data on the attitudes of the many clinicians involved to better understand the perspective of the different specialties and promote consistency among them as well. This would ultimately better serve families encountering this decision-making process in the future. Continued research is also needed on the cardiac conditions and influential variables impacting surgical treatment in a larger population of cardiac surgeons to better describe how these decisions are made. Finally, if current trends continue and more families are offered and pursue the option of surgery, longitudinal research should be done to assess these outcomes as well as the experiences of the families. This will provide necessary information to those clinicians still hesitant to broach this topic based on insufficient research on outcomes and will also provide better understanding of clinician and family interactions.
5 PRACTICE IMPLICATIONS
The goal of this study was not to provide recommendations for uniform care of all infants with heart defects and T-18, as an individualized approach to each patient is paramount. Results of this study may lead to a heightened appreciation for the complexity of this issue for clinicians who may perceive cardiac surgery as irrelevant or believe that the barrier to access cardiac surgeons who are willing to perform surgery is so great that it is simply not worth considering. Discussions may evolve to include the recognition of the option of cardiac surgery in the discussion of management of infants with T-18, including an acknowledgment that this may not be available based on the clinical picture or other center-specific criteria, and permission for families to not explore or choose this option. Appropriate referrals can be provided if the discussion is beyond the clinician's scope of practice, knowledge, or comfort. Additionally, genetic counselors involved in either or both the pre- and postnatal discussions regarding the care and management for families with a diagnosis of T-18 have the skills and training to explore with the family psychosocial issues surrounding their desire to pursue cardiac surgery. Through such conversations, the genetic counselor is often able ascertain the family's values and wishes for their child, and better understand the motivations behind the pursuit of aggressive interventions. Therefore, genetic counselors can serve important roles in multidisciplinary teams as healthcare professionals uniquely suited to explore the psychosocial needs of a patient and advocate for those needs to be met when possible, balancing patient autonomy, and further promote collaboration among the care team to make complex management decisions (“National Society of Genetic Counselors Code of Ethics,” 2018).
We hope the results of this study will be shared within and among multidisciplinary specialties involved in the care of infants with T-18 leading to further education and informed attitudes regarding this topic. We appreciate that while differing clinician opinions may always exist, it is reasonable to expect clinicians to collaborate with one another in the care of families of infants with T-18 in order to promote consistent patient care and open and honest discussions exploring families' goals and wishes (Supporting Information Data S1).
COMPLIANCE WITH ETHICAL STANDARDS
Conflict of interest
Meagan Kaulfus, Helena Gardiner, S. Shahrukh Hashmi, Hector Mendez-Figueroa, Blair Stevens, and Rebecca Carter declare no conflicts of interest. Victoria J. Miller is the Executive Director of the Trisomy 18 Foundation, a non-profit organization. She received no compensation for participation in this study.
Human studies and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Animal studies
No non-human animal studies were carried out by the authors for this article.
AUTHORSHIP CONTRIBUTIONS
Meagan Kaulfus, Helena Gardiner, S. Shahrukh Hashmi, Hector Mendez-Figueroa, Victoria J. Miller, Blair Stevens, and Rebecca Carter all made substantial contributions to this study as outlined by the International Committee of Medical Journal Editors (ICMJE). Every author made substantial contributions to the conception or design of the work, drafting the work, or revising it critically for important intellectual content, provided final approval of the version to be published, and agrees to be accountable for all aspects of the work.
ACKNOWLEDGEMENTS
We would like to thank the 18 fetal center genetic counselors, the National Society of Genetic Counselors, and Dr. Anthony Johnson and the North American Fetal Therapy Network for aiding in the dissemination of our survey. This research was performed with the support of Claire Singletary and the Genetic Counseling Program at The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences as partial fulfillment of the first author's M.S. degree requirements.