Virtual reality simulation of panoramic radiographic anatomy for dental students
Abstract
Purpose
This work aimed to utilize virtual reality (VR) in dental radiographic anatomical interpretation in junior dental students and test if it can enhance student learning, engagement, and performance.
Methods
VR software for panoramic anatomy was developed. Sixty-nine first-year dental students were divided into a control group (lecture-based) and an experimental group (VR) to learn panoramic radiographic anatomy. Both groups were then tested on knowledge via a 20-question quiz. Student feedback on VR experience was collected via an online survey.
Results
There was a statistically significant difference between lecture-based and VR students in the correct identification of anatomical landmarks. Lecture-based students scored higher in identifying the ear lobe, hyoid bone, condylar neck, and external oblique ridge, whereas VR students scored higher in identifying zygoma (Chi-squared test, p < 0.005). The VR group reported high evaluation on all perception items of the online feedback survey on their experience (Student t-test, p < 0.005).
Conclusions
Lecture-based students generally showed better performance in panoramic radiographic anatomy. Several structures were not correctly identified in both groups of novice students. The positive feedback of VR experience encourages future implementation in education to augment conventional methods of radiographic anatomy in dentistry with considerations to repeated exposures throughout undergraduate dental education.
1 INTRODUCTION
Panoramic radiographs are used by dental students and dentists in daily clinical practice. However, an accurate interpretation of panoramic radiographs is particularly challenging as many anatomical structures are superimposed in one image. Technical errors during image acquisition will result in image distortions. Additional challenges are created by ghost shadows, anatomical variation, artifacts, and anatomical structures outside the jaw depicted in the image. Therefore, enhancing the understanding and interpretation of a panoramic radiograph is necessary.1
Over the years, digital applications and technological advances have increased and become widely used in medical and dental disciplines. Virtual simulation gained attention and has been implemented in education, training, and patient experience in medicine.2
There are two areas of simulation technologies: virtual reality (VR) and augmented reality (AR). VR is a computer-generated artificial simulation of real-life situations where the user feels like experiencing the simulated situation as it is in real life. VR technology offers operator immersion and interaction.3 While AR is a computer-generated artificial virtual scenario using systems on mobile devices showing virtual simulation atop an existing reality and interact with it.4
To date, VR and AR have been applied and implemented in many medical and dental fields. Both showed great benefits and opened a new approach to education and treatment. Several studies have reported the use of VR in neurosurgical training, rehabilitation of stroke patients, treatment of phantom limb pain, endoscopy training, surgical planning, reducing many kinds of phobias in patients, and immersive education of the anatomy.5-10 Moreover, other wide applications render VR and AR promising tools in the medical and dental fields.11
Recently, the implementation of VR simulation in pre-clinical dental training has been facilitated by technological advances.12 Some dental schools have already applied the new sciences to dental education and become an integral part of dental practice.13 Previous studies showed that students are more interested when modern education methods are being used instead of traditional methods.14-16 Evidence showed that when VR simulation is being used, students learn faster and achieve better practical performance.17
Historically, simulation in dentistry started with a phantom head that simulates the patient's head. The first phantom head simulator was built in 1894 by Oswald Fergus. Restorative techniques were practiced using extracted natural teeth on the phantom head, but the major issue was the limitation of natural teeth and the increase in demand.18 The development of VR simulators in dentistry started in late 1990. One of the pioneering virtual systems is DentSim, where the learning mannequin is combined with 3D visuals. This system uses infrared technology to present 3D images to the student on the phantom setting's computer screen.19 Another system is Simodont (MOOG, the Netherlands), this technology uses the aircraft simulation industry and allows restoration of the 3D simulated tooth and finishing the restoration.20
VR technology reinforces the learned dental concepts and provides an automatic demonstration, and easy access to the data to the students.21 With the availability of virtual education in dental schools, students can have an independent nature of learning experience with high-quality images, freedom of navigation, and unlimited trials. However, establishing a virtual network system has limitations such as the high cost and unfamiliarity of these systems, which requires VR specialists.22
Dental students’ knowledge of panoramic anatomy, errors, or artifacts has been investigated and showed varying degrees of correct answers.23, 24 Implementing new methods in teaching radiographic anatomy was tested however, was based on senior students, utilized 2D digital techniques, or applied VR video for teeth morphology only.25, 26
This research aims to assess the effectiveness of utilizing VR in dental radiographic anatomical interpretation among novice dental students and whether it can enhance student learning, engagement, and performance.
2 METHODOLOGY
2.1 Workflow development for VR software
The main theme and structure of the user experience, including the models, characters, and way of interaction were determined by the oral and maxillofacial radiologist with the consensus of the authors.
The 3D assets were then designed and adapted using a 3D content creation application (Autodesk 3ds Max). Next, integration of the 3D assets, creation of the effects, implementing the avatars, and optimizing the products for VR hardware were done by working directedly on the 3D engine (Unreal engine). Finally, testing and debugging were done directly in the head-mounted display to assess the VR experience and get back to the 3D engine phase for correction if needed.
The VR interactive software was created to project two images: a panoramic radiograph and a 3D skull. This display allowed the user to view the anatomical structure on the panoramic radiograph and highlight it on the 3D skull simultaneously. The user could interact and rotate the 3D skull 360 degrees. The list of anatomical structures appeared on the left and a written description with explanatory audio for each structure appeared on the right (Figures 1 and 2). The software was developed by Black Dune Studio. (http://www.blackdunestudio.com). The content of the VR software was reviewed by the oral and maxillofacial radiologist for final approval.
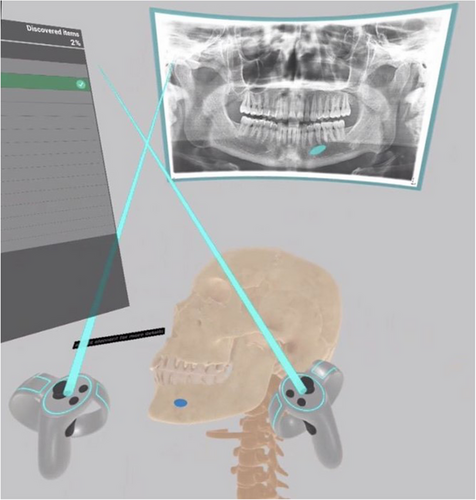
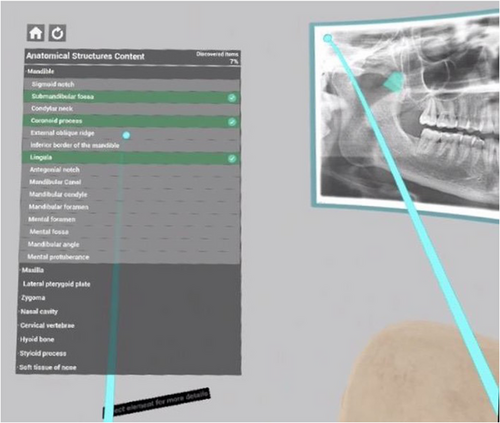
Virtual Reality headsets: Three VR headsets were used (Oculus Quest 2).
2.2 Study participants
The study included first-year dental students at the College of Dentistry, King Saud University, Riyadh, Saudi Arabia. A total of 72 students were invited to participate in the study. Three students withdrew before the commencement of the study for personal excuses. The remaining 69 students were randomly assigned into a control group of 35 students (21 male,14 female) and an experimental group of 34 students (21 males and 13 females). The following exclusion criteria were applied to participating students: previous history of VR experience, seizures, dizziness or vomiting, students with hearing aids or pacemakers, and pregnant females.
2.3 Study setting and design
This study was approved by the Institutional Review Board of King Saud University, Riyadh, Saudi Arabia (E-20-5585). The study was conducted in the College of Dentistry, King Saud University, Riyadh, Saudi Arabia. Before the commencement of the study, the purpose of the study and the required tasks were explained and clarified and written informed consent was obtained from all participants. According to the curriculum of the College of Dentistry, King Saud University, first-year dental students have finished the gross anatomy course but had no exposure to any dental radiology courses.
The control group received the conventional educational method of an in-person faculty-led presentation about the radiographic anatomical interpretation of panoramic radiography given as a lecture for 30 min. Whereas, the experimental group received the same educational material using VR interactive software viewed using VR headsets for 15–20 min. Immediately after the lecture and VR sessions, both groups were subjected to an online quiz that comprised 20 questions to identify different anatomical landmarks on dental panoramic radiograph. The questions were multiple choice questions with one correct answer among four options. The questions were evaluated by an oral and maxillofacial radiologist and statistician to assess the knowledge retention of both control and experimental groups. The experimental group received another online survey of 15 questions to assess the influence and acceptance of using VR technologies in dental education. The questionnaire was designed based on the Likert scale. The data was collected from the quiz and the online survey feedback.
The scores of the quiz were evaluated and compared between the control and experimental groups to assess the effectiveness and knowledge retention by utilizing VR interactive video compared to lecture-based presentation in the interpretation of the anatomical landmarks on dental panoramic radiographs.
One panoramic radiograph of an adult subject was used in the lecture-based and VR groups as well as the quiz. The panoramic radiograph was selected by the oral and maxillofacial radiologist depicting the landmarks clearly, with optimum contrast and brightness, and with no errors.
2.4 Data analysis
Data were analyzed using IBM SPSS Statistical software for Windows version 26.0 (IBM Corp., Armonk, N.Y., USA). Descriptive statistics (frequencies, percentages, mean, and standard deviation) were used to describe the categorical (gender, group, and dichotomized correct answers per landmark) and quantitative variables (age, answers per landmark, and Likert-scale for survey). Bivariate analysis was carried out using Student's t-test for independent samples, to compare the mean scores of correct responses of 20 structures in relation to the categorical study variables which have two options (groups [experimental & control], gender [male & female] and age groups [<20 and ≥20 years]). Student's t-test was used to assess the Likert scale for the VR questionnaire. Pearson's Chi-square test was used to compare the proportions of correct/wrong answers toward the 20 structures between experimental and control groups. A p-value of <0.05 was used to report the statistical significance of the results.
3 RESULTS
A total of 69 dental students were allocated into experimental (VR) and control (lecture-based) groups. The VR group consisted of 21 males and 13 females (17 were <20 years and 17 were 20 years or over). The lecture-based group consisted of 21 males and 14 females (18 were <20 years and 17 were 20 years or over). Normality testing of the data based on graphical methods and Shapiro–Wilk test revealed that the data was normally distributed. The mean scores of correct responses between males and females and between two age groups (<20 and ≥20 years) in each of the VR and lecture-based groups showed no statistically significant differences (p > 0.05).
The students’ responses toward the 20 structures were converted into scores, by allocating “1” for the correct option and “0” for the wrong options. The mean scores for the VR and lecture-based groups were 9.88 and 11.66, respectively. The difference in the mean scores of these two groups was statistically significant, where the lecture-based group had higher mean scores of correct responses when compared with the mean scores of correct responses of the VR group (p = 0.004) (Table 1). The responses for the 20 structures and their distribution across the VR and lecture-based groups are given in Table 2.
| Groups | Scores Mean ± SD | 95% confidence interval of the difference | t-value | p-value |
|---|---|---|---|---|
| Experimental (VR) | 9.88 ± 2.25 | Not applicable | ||
| Male | 9.76 ± 1.67 | (−1.96, 1.33) | −0.391 | 0.698 |
| Female | 10.08 ± 3.04 | |||
| <20 years | 9.65 ± 2.71 | (−2.06, 1.12) | −0.603 | 0.551 |
| ≥20 years | 10.12 ± 1.73 | |||
| Control (lecture-based) | 11.66 ± 2.69 | Not applicable | ||
| Male | 11.14 ± 2.85 | (−3.15, 0.58) | −1.40 | 0.169 |
| Female | 12.43 ± 2.31 | |||
| <20 years | 12.28 ± 2.11 | (−0.54, 3.10) | 1.426 | 0.163 |
| ≥20 years | 11.00 ± 3.12 | |||
| Difference of mean VR versus lecture-based | 1.775 | (0.58, 2.97) | 2.967 | 0.004* |
- * Statistically significant.
| Identification of the anatomical structure | VR group N (%) |
Lecture-based group N (%) |
X2-value | p-value |
|---|---|---|---|---|
| 1. Structure (A) | ||||
| A. Maxillary tuberosity | 8 (23.5) | 8 (22.9) | ||
| B. Zygomatic process of maxilla** | 8 (23.5) | 15 (42.9) | 2.899 | 0.089 |
| C. Maxillary sinus | 14 (41.2) | 6 (17.1) | ||
| D. Zygoma | 4 (11.8) | 6 (17.1) | ||
| 2. Structure (B) | ||||
| A. Zygomatic arch | 20 (58.8) | 2 (5.7) | ||
| B. Maxillary sinus | 3 (8.8) | 5 (14.3) | ||
| C. Pterygomaxillary fissure** | 9 (26.5) | 21 (60.0) | 7.890 | 0.005 |
| D. Superior Orbital fissure | 2 (5.9) | 7 (20.0) | ||
| 3. Structure (C) | ||||
| A. Zygoma or malar bone** | 6 (17.6) | 1 (2.9) | ||
| B. Zygomatic process of maxilla | 11 (32.4) | 4 (11.4) | ||
| C. Hard palate | 15 (44.1) | 26 (74.3) | 4.138 | 0.042* |
| D. Coronoid process | 2 (5.9) | 4 (11.4) | ||
| 4. Structure (D) | ||||
| A. Artifact | 0 | 0 | ||
| B. Earlobe** | 18 (52.9) | 34 (97.1) | ||
| C. Hyoid bone | 9 (26.5) | 1 (2.9) | 18.148 | <0.0001* |
| D. Ossified stylohyoid ligament | 7 (20.6) | 0 | ||
| 5. Structure (E) | ||||
| A. Hard palate | 13 (38.2) | 2 (5.7) | ||
| B. Maxillary sinus** | 7 (20.6) | 7 (20.0) | ||
| C. Tongue | 2(5.9) | 0 | 0.004 | 0.952 |
| D. Coronoid process | 12 (35.3) | 26 (74.3) | ||
| 6. The horizontal opacity apical to the maxillary teeth | ||||
| A. Cervical spine | 7 (20.6) | 10 (28.6) | ||
| B. Pharyngeal airspace | 4 (11.8) | 3 (8.6) | ||
| C. Hard palate** | 21 (61.8) | 19 (54.3) | 0.396 | 0.529 |
| D. Enlarged impacted tooth | 2 (5.9) | 3 (8.6) | ||
| 7. The opacity labeled (F) | ||||
| A. Hyoid bone** | 22 (64.7) | 32 (91.4) | ||
| B. Sialolith | 2 (5.9) | 1 (2.9) | ||
| C. Ghost image | 2 (5.9) | 1 (2.9) | 7.239 | 0.007* |
| D. Collar bone | 8 (23.5) | 1 (2.9) | ||
| 8. Structure (G) | ||||
| A. Hyoid bone | 1 (2.9) | 1 (2.9) | ||
| B. Cyst | 2 (5.9) | 2 (5.7) | ||
| C. Condylar neck** | 17 (50.0) | 27 (77.1) | 5.499 | 0.019* |
| D. Superior wall of maxillary sinus | 14 (41.2) | 5 (14.3) | ||
| 9. Structure (T) | ||||
| A. Nasal septum** | 34 (100) | 33 (94.3) | ||
| B. Mastoid process | 0 | 1 (2.9) | – | 0.493 |
| C. Floor of the middle cranial fossa | 0 | 0 | ||
| D. Fracture | 0 | 1 (2.9) | ||
| 10. Structure (H) | ||||
| A. Mental foramen | 1 (2.9) | 2 (5.7) | ||
| B. Inferior alveolar nerve canal** | 8 (23.5) | 9 (25.7) | 0.044 | 0.833 |
| C. External oblique ridge | 11 (32.4) | 14 (40.0) | ||
| D. Mandibular foramen | 14 (41.2) | 10 (28.6) | ||
| 11. Structure (I) | ||||
| A. Lingula | 7 (20.6) | 0 | ||
| B. Submandibular fossa** | 26 (76.5) | 26 (74.3) | 0.044 | 0.833 |
| C. Ghost image | 0 | 2 (5.7) | ||
| D. Sigmoid notch | 1 (2.9) | 7 (20.0) | ||
| 12. Structure (J) | ||||
| A. Mandibular angle** | 33 (97.1) | 31 (88.6) | ||
| B. Mental fossa | 0 | 1(2.9) | 1.848 | 0.174 |
| C. Ghost image | 0 | 0 | ||
| D. Antegonial notch | 1 (2.9) | 3 (8.6) | ||
| 13. Structure (K) | ||||
| A. Coronoid process | 10 (29.4) | 4 (11.4) | ||
| B. Mylohyoid ridge | 6 (17.6) | 1 (2.9) | 4.248 | 0.039* |
| C. External oblique ridge** | 16 (47.1) | 25 (71.4) | ||
| D. Condylar neck | 2 (5.9) | 5 (14.3) | ||
| 14. Structure (L) | ||||
| A. Coronoid process | 11 (32.4) | 11 (31.4) | ||
| B. Mandibular condyle** | 15 (44.1) | 17 (48.6) | 0.138 | 0.711 |
| C. Glenoid fossa | 4 (11.8) | 5 (14.3) | ||
| D. Articular eminence | 4 (11.8) | 2 (5.7) | ||
| 15. Structure (M) | ||||
| A. Coronoid process | 4 (11.8) | 2 (5.7) | ||
| B. Hamulus | 11 (32.4) | 9 (25.7) | 1.748 | 0.186 |
| C. Cranial base | 2 (5.9) | 1 (2.9) | ||
| D. Maxillary tuberosity** | 17 (50.0) | 23 (65.7) | ||
| 16. Structure (N) | ||||
| A. Sigmoid notch** | 25 (73.5) | 20 (57.1) | ||
| B. Articular eminence | 5 (14.7) | 7 (20.0) | 2.041 | 0.153 |
| C. Coronoid process | 2 (5.9) | 7 (20.0) | ||
| D. Lingula | 2 (5.9) | 1 (2.9) | ||
| 17. Structure (O) | ||||
| A. Mylohyoid ridge | 2 (5.9) | 4 (11.4) | ||
| B. Inferior border of mandible** | 27 (79.4) | 28 (80.0) | 0.004 | 0.952 |
| C. External oblique ridge | 3 (8.8) | 3 (8.6) | ||
| D. Hyoid bone | 2 (5.9) | 0 | ||
| 18. Structure (P) | ||||
| A. Anterior nasal spine | 14 (41.2) | 12 (34.3) | ||
| B. Incisive foramen** | 15 (44.1) | 21 (60.0) | 1.743 | 0.187 |
| C. Infraorbital canal | 2 (5.9) | 2 (5.7) | ||
| D. Intermaxillary suture | 3 (8.8) | 0 | ||
| 19. Structure (Q) | ||||
| A. Pterygoid plate | 10 (29.4) | 6 (17.1) | ||
| B. Coronoid process** | 2 (5.9) | 6 (17.1) | 2.133 | 0.144 |
| C. Maxillary tuberosity | 8 (23.5) | 9 (25.7) | ||
| D. Pterygomaxillary fissure | 14 (41.2) | 14 (40.0) | ||
| 20. Structure (R) | ||||
| A. Nasopharynx | 3 (8.8) | 1 (2.9) | ||
| B. Ramus | 7 (20.6) | 5 (14.3) | 0.464 | 0.496 |
| C. Ear lobe | 14 (41.2) | 16 (45.7) | ||
| D. Styloid process** | 10 (29.4) | 13 (37.1) | ||
- ** Correct answer.
- * Statistically significant.
3.1 Perception toward VR experience
The VR group study subjects completed a total of 15 positive statements with a 5-point scale to assess the effectiveness of virtual education, as shown in Table 3.
| Responses No. (%) | |||||||
|---|---|---|---|---|---|---|---|
| Perception items | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | t-value | p-value |
| 1. Using Virtual Reality applications improves my performance in my courses | 25 (75.8) | 6 (18.2) | 1 (3.0) | 1 (3.0) | – | 47.36 | <0.0001* |
| 2. Using Virtual Reality applications will increase my productivity in my courses | 21 (63.6) | 11 (33.3) | 1 (3.0) | – | – | 18.18 | <0.0001* |
| 3. Using Virtual Reality applications will increase my motivation in my courses | 23 (69.7) | 10 (30.3) | – | – | – | 5.12 | 0.024* |
| 4. Using Virtual Reality applications will make it easier to do assignments in the future | 27 (81.8) | 5 (15.2) | 1 (3.0) | – | – | 35.64 | <0.0001* |
| 5. I find the use of Virtual Reality applications will be beneficial in my radiology course | 23 (69.7) | 9 (27.3) | 1 (3.0) | – | – | 22.54 | <0.0001* |
| 6. I find the use of Virtual Reality applications will be beneficial in other courses | 24 (72.7) | 9 (27.3) | – | – | – | 6.82 | 0.009* |
| 7. Using Virtual Reality applications will enable the learning process to be effective in my courses | 21 (63.6) | 11 (33.3) | 1 (3.0) | – | – | 18.18 | <0.0001* |
| 8. I can easily use Virtual Reality applications | 25 (75.8) | 7 (21.2) | 1 (3.0) | – | – | 28.36 | <0.0001* |
| 9. It takes less time to complete a task when I use Virtual Reality applications | 20 (60.6) | 5 (15.2) | 5 (15.2) | 3 (9.1) | – | 22.64 | <0.0001* |
| 10. I feel comfortable while using Virtual Reality applications | 20 (60.6) | 7 (21.2) | 5 (15.2) | 1 (3.0) | – | 24.58 | <0.0001* |
| 11. I can detect any structure I want with Virtual Reality applications | 22 (66.7) | 10 (30.3) | 1 (3.0) | – | – | 20.18 | <0.0001* |
| 12. I have the essential knowledge to use Virtual Reality applications effectively | 20 (60.6) | 9 (27.3) | 4 (12.1) | – | – | 12.18 | 0.002* |
| 13. I can get help when I have difficulty using Virtual Reality applications | 21 (63.6) | 9 (27.3) | 1 (3.0) | 2 (6.1) | – | 30.88 | <0.0001* |
| 14. Using Virtual Reality applications is Similar to using other computer applications | 16 (48.5) | 5 (15.2) | 5 (15.2) | 5 (15.2) | 2 (6.1) | 17.76 | 0.001* |
| 15. People around me think it's important that I use Virtual Reality applications effectively | 14 (42.4) | 9 (27.3) | 8 (24.2) | 2 (6.1) | – | 8.82 | 0.032* |
- * Statistically significant.
The ordinal responses of 15 perception items were converted into total scores. There was no statistically significant difference in the mean scores of perceptions between the age groups and gender. The majority of VR group participants strongly agreed that VR applications were a positive experience in all 15 statements, this finding was statistically significant (Table 3).
4 DISCUSSION
The current integration of computer-based and digital learning in education has been widespread in both medical and dental fields. Virtual simulation is one of the applications that gained popularity and was incorporated into medical education, training, and patient experience.2 Evidence showed that the utilization of VR simulation in education allows students to learn faster and achieve superior practical results.17, 27
Current undergraduate students, especially “Millennials”, are more responsive to new methods of e-learning and e-teaching. To educate these young dentists for their everyday work lives, dental curricula must account for this trend toward digitalization and continuous advances. To do this, it is essential to offer these new ways while keeping in mind how students will engage and learn from them.25, 28, 29
The identification and interpretation of radiographic anatomy may pose a challenge. Particularly panoramic radiography, where technical aspects of projection and superimposition intervene continually. This research introduces a new, innovative, and interactive method for enhancing the quality of learning and overcoming these challenges. In the current study, the conventional lecture-based group scored better than the VR group (Table 2). This finding is in contrast to the study by Vuchkova et al.25 This might be due to the time spent with the educational material. The lecture-based group had a 30-min lecture with the oral and maxillofacial radiologist, whereas the VR students spent 15 min navigating the virtual video, which possibly affected their answers. However, the headset manufacturer recommends that the first use should not exceed 25 min. We recommend training the students with the device before starting the demonstration. This, however, as with interactive educational modalities, renders time a factor in the efficiency and effectiveness of the teaching tool.25 Although VR requires more time for the student, it can decrease faculty time by fivefold.30-32 Alterations to update the dental curriculum can be justifiable given the benefits and improved experience by the student.
Generally, both student groups showed high frequency in the correct identification of landmarks except for the maxillary sinus, zygoma, inferior alveolar nerve canal, coronoid process, and styloid process (Table 2). The maxillary structures (maxillary sinus and zygoma) were easily confused with adjacent structures such as the coronoid process or hard palate. The depiction of maxillary structures on panoramic radiography is challenging due to the intricate and smaller anatomy, and superimposition of soft tissues compared to mandibular structures. The inferior alveolar nerve canal was mostly identified as mandibular foramen or external oblique ridge, the coronoid process as the maxillary tuberosity, and the styloid process as the earlobe as these structures can overlap, superimpose, or are similar in outline.
When comparing the lecture-based and VR groups, the former showed higher frequency in the correct identification of most anatomical landmarks. Statistical significance in the landmark identification was marginal (p = 0.005) in pterygomaxillary fissure and reached statistical significance (p < 0.005) in five structures: zygoma, earlobe, hyoid bone, condylar neck, and external oblique ridge. The zygoma was incorrectly identified, for the most part, but the lecture-based group showed higher frequency of incorrect answers as the hard palate. It is possible that a surface anatomy such as the zygoma was better depicted using VR rather than lecture-based methods. The remaining four structures were more erroneously identified by the VR group compared to the lecture-based as other anatomical structures that are nearby or with similar outlines: earlobe mistaken for hyoid or ossified stylohyoid ligament, hyoid mistaken for collar bone, condylar neck with the superior wall of maxillary sinus, and external oblique ridge with the coronoid process.
Incorrect answers in panoramic anatomy identification were observed in senior and recently graduated dental students.23, 24 The errors are mostly in the maxillary, nasal, and cervical spine areas, or air/soft tissue shadows. Previous work identified lecture/hour training and whether the student took panoramic radiographs or not as possible factors, and recommended repeated exposures to panoramic anatomy training. In the context of a one-time exposure to panoramic radiography in novice students, some errors in anatomical identification are not entirely unexpected in our study, even if the structure seems straightforward.
The assessment survey revealed that students had a positive attitude toward VR as a learning resource, as shown in Table 3. This survey was designed by Usten et al., according to different themes: “Performance Expectancy,” “Effort Expectancy,” “Facilitating Conditions,” and “Social Influence.”33 Regarding the “Performance Expectancy,” questions 1–7, the majority of students reported that the use of VR technologies in dental radiology education enables the work to be completed more quickly, improves their performance, increases their productivity and motivation, improves the quality of their learning in radiology and the other courses, and makes it more effective and efficient, similar findings were found in Vuchkova et al. and Liebermann et al. studies.25, 26 Furthermore, regarding the “Effort Expectancy”, questions 8–11, the students believed that they could use VR technology with minimal effort and with little difficulty. This result might be seen as increasing students' acceptance and use of VR technology in future dental education. Concerning “Facilitating Conditions”, questions 12–14, most students responded that they had the knowledge necessary to utilize VR technologies, there are individuals from whom they may seek assistance if they encounter difficulties, and the usage of VR is comparable to the use of other computer applications. Finally discussing the “social influence” in question 15, we found that most students believed that there are social impacts associated with the usage of VR technology in education.
Using VR alone in the classroom requires more investigation, but it currently has limitations that prohibit it from fully replacing faculty-guided lectures. Traditional lecture-based presentations are still beneficial to the dental curriculum. However, the students report that using VR for oral radiographic anatomy seems to enhance the learning experience by allowing effective interaction with the course material. Before introducing VR into the formal education curriculum, students must be adequately prepared and trained. Unfortunately, developing the hardware and software, as well as modification, maintenance, and repair have a significant expense that must be considered.
This work has some limitations. One was not including senior participants to compare the possible effects of experience and previous knowledge. The time limit to conduct this work limited the allocated duration of VR training and exposure. The hardware and software were not readily accessible, very costly, and time-consuming. Furthermore, the VR video lacks audio commentary for some structures that we assumed would be self-explanatory. Including dental students from different year levels must be conducted to discover the rationale for incorrect answers, particularly those that have no shape similarity or are anatomically far from one another. Before beginning the experiment, we propose introducing the student to the VR experience for some time. Comparing advanced courses versus early courses, and adding a third sample group that engages in both VR and lecture-based lectures would be interesting future explorations.
Within the limitations of this study, it can be concluded that lecture-based students generally showed better performance in panoramic radiographic anatomy compared to VR. Several structures were not correctly identified in both groups of novice students.
ACKNOWLEDGMENTS
The Authors would like to acknowledge the “Researchers Supporting Project” number (RSP2023R234), King Saud University, Riyadh, Saudi Arabia. The Authors would like to thank “Black Dune Studio” for their assistance and technical efforts.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.




