Association between serum levels of bone turnover markers and bone mineral density in men and women with type 2 diabetes mellitus
Abstract
Background
In patients with type 2 diabetes mellitus (T2DM), higher risks of impaired bone metabolism are widely reported. To evaluate bone metabolism, bone mineral density (BMD) and bone turnover levels should be included. In this article, we analyzed the relationship between them in T2DM.
Methods
We conducted a hospital-based cross-sectional study enrolling 1499 patients hospitalized for T2DM between October 2009 and January 2013. Multivariate linear regression models were used to identify the relationship between bone turnover markers (BTMs) and BMD levels. A two-sided P-value < .05 was considered statistically significant.
Results
After adjusting for confounding factors, osteocalcin (OC) showed a negative relationship with total lumbar, femur neck, and total hip BMD in men and women. N-terminal propeptides of type I collagen (P1NP) and alkaline phosphatase (ALP) showed a negative association with BMD at three sites in men and total lumbar BMD in women, whereas in the femur neck and total hip in women, the relationship was only found for P1NP with total hip. For β-C-terminal telopeptides of type I collagen (β-CTX), a negative relationship was also found in all three sites for BMD in men and total lumbar BMD in women, whereas β-CTX was not associated in the femoral neck and total hip in women.
Conclusion
In patients with T2DM, serum levels of OC, P1NP, β-CTX, and ALP were negatively correlated with BMD levels in men in three sites and with total lumbar BMD in women. The relationship varied in femur neck and total hip BMD in women.
1 INTRODUCTION
In patients with type 2 diabetes mellitus (T2DM), the incidence of osteoporosis and related fractures is common, which results in a great economic and social burden, especially in the elderly.1 It was reported that a history of diabetes is an independent risk factor of low-energy subtrochanteric and diaphyseal fractures.2 In two large systematic reviews, the association between T2DM and hip fractures incidence was found to be consistent (relative risk [RR] = 1.7, 95% confidence interval [CI]: 1.3-2.2; RR = 1.38, 95% CI = 1.25-1.53).3, 4 Consequently, more intensive management of bone health in type 2 diabetic patients was brought into focus.
To evaluate bone health in people with T2DM, bone strength, including bone mineral density (BMD) and bone quality, should be comprehensively assessed. Among various evaluation methods, determination of BMD and bone turnover levels is most commonly adopted. BMD, tested by dual-energy X-ray absorptiometry (DXA) examination, is still the mainstay for bone metabolism evaluation, especially for osteoporosis.5 Testing of serum levels of bone turnover markers (BTMs), a noninvasive method in evaluating bone turnover status, is useful in the treatment process, including timing of pharmacological intervention initiation, evaluation of therapeutic response, and assessment for treatment regimen modification. Furthermore, BTMs could be used in monitoring treatment adherence.6 Currently, BTMs are recognized as promising tools in the evaluation of bone metabolism and quality by the National Osteoporosis Foundation.7 BTMs are classified as bone formation markers (eg, N- and C-terminal propeptides of type I collagen [P1NP and P1CP], alkaline phosphatase [ALP] or bone-specific ALP, and osteocalcin [OC]) and as bone resorption markers (eg, C- and N-terminal telopeptides of type I collagen [CTX and NTX], pyridinoline, and deoxypyridinoline).8 Although OC used to be considered as a bone formation marker, it was reported to represent bone resorption process as well, and it may consequently represent the levels of bone turnover.9 Some bone metabolic hormones also influence bone metabolism, such as parathyroid hormone (PTH) and 25-hydroxyvitamin D (25[OH]D).10 In people with T2DM, BMD might controversially increase, decrease, or even change insignificantly, but more studies tended to report normal or even increased BMD.3, 11-13 In terms of bone turnover levels, it has been proposed that bone formation is suppressed in the diabetic state while bone resorption levels are unclear.14, 15 In a meta-analysis, a state of low bone turnover was determined in patients with diabetes as both markers of bone formation and bone resorption decreased.16 Thus, in people with T2DM, steady BMD levels and suppressed BTM levels might be concluded.
However, with an aim to comprehensively evaluate bone metabolism in T2DM by adopting both BMD and BTM examination, we need to further clarify the relationship between them and to find out if they interact with each other. Furthermore, in clinical practice, the use of BMD examination was always restricted by limited number of instruments, relatively longer follow-up period, etc, while BTM testing is rather more convenient. What is more, the changes in serum levels of BTMs are usually faster than levels of BMD. Consequently, the analysis of the relationship between BTMs and BMD in patients with T2DM might contribute to prediction of changes in BMD levels according to variation in serum levels of BTMs in clinical practice. Ten studies have reported on a relationship between BTMs and BMD.12, 17-25 Among them, three studies were conducted in Asia, including two articles in Japan that failed to show a significant relationship in men and women and one article in China that revealed different relationships in different kinds of BTMs in postmenopausal women (negative or positive). Studies from other continents also reported controversial results.
In this study, we aimed to evaluate the levels of BMD and BTMs in men and women with T2DM and analyze the relationship between bone turnover (serum levels of BTMs indicating bone formation and bone resorption levels) and BMD levels at three different sites (including total lumbar, femur neck, and total hip), in which men and women would be considered separately.
2 MATERIALS AND METHODS
2.1 Participants
In this hospital-based cross-sectional study, we identified all Chinese patients aged ≥18 years, who were hospitalized for T2DM, and were not in a hyperosmolar hyperglycemic state or in a state of diabetic ketoacidosis between October 2009 and January 2013 at the Department of Endocrinology and Metabolism in Zhongshan Hospital, Fudan University. Exclusion criteria included a history of lethal cardiovascular, liver, or renal disease. Patients also had no regular or past history of medication that might have influence bone metabolism, such as calcium, vitamin D, antiresorptive, or anabolic treatment and had no tumor disease or other endocrinological disease. Both written and informed consents were obtained from all study participants, and the study protocol was approved by the appropriate ethics review board of Zhongshan Hospital, Fudan University. Patients without serum BTM and BMD data and those who had repeated hospitalization were excluded. A total of 1499 patients were included in the final analysis.
2.2 Data collection
Data for basic personal information, serum biochemical tests, and BMD results of included patients were obtained. Basic personal information included age, sex, diabetes duration, and body mass index (BMI). Information regarding T2DM treatment included diet or newly diagnosed, insulin, oral medicine, or insulin plus oral medicine; oral medicines included insulin-secreting agents, metformin, alpha-glucosidase inhibitors, and insulin-sensitizing agents. Other information included smoking history, drinking, hypertension, cerebrovascular disease, dyslipidemia, and kidney disease. Patients with kidney diseases were considered as having a definite history of diagnosis and treatment for any kidney disease. Body weight and height were measured, with patients wearing light clothing and no shoes. BMI was defined as weight in kilograms divided by height in meter squared. Blood pressure was obtained after a 5-min rest using an electronic sphygmomanometer. Serum biochemical tests during hospitalization included determination of fasting blood glucose (FBG), glycosylated hemoglobin (HbA1C), high-sensitivity C reactive protein (hsCRP), total cholesterol, triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), 25(OH)D, PTH, calcium (Ca), and magnesium (Mg) levels and the estimated glomerular filtration rate (eGFR, using the Modification of Diet in Renal Disease [MDRD] equation calculated from serum creatinine levels). Serum levels of OC, P1NP, β-CTX, and ALP were also determined. Blood samples were collected after an overnight fasting of at least 8 hours. Each participant had BMD measurement by DXA (Hologic Discovery). The measurement sites were the total lumbar area, femur neck area, and total hip area.
2.3 Diagnostic criteria of T2DM
We defined T2DM on the basis of the American Diabetes Association criteria as follows: fasting plasma glucose ≥ 126 mg/dL (7.0 mmol/L) (fasting was defined as at least 8 hours of no caloric intake); 2-hour plasma glucose ≥ 200 mg/dL (11.1 mmol/L) during oral glucose tolerance test; and random plasma glucose ≥ 200 mg/dL (11.1 mmol/L) with classic hyperglycemia symptoms, including polydipsia, polyuria, and unexplained weight loss. Without unequivocal hyperglycemia symptoms, the three criteria were reevaluated on a different day.26 By measuring insulin levels and auto-antibodies, patients diagnosed as type 1 diabetes mellitus with absolute insulin deficiency risk of ketoacidosis, or with positive markers for the immune destruction of β-cells, were excluded.26
2.4 Statistical analyses
We performed the analyses separately for men and women. We used the number and proportion to describe the categorical variables and mean ± standard deviation (SD) to describe continuous variables. We used one-way analysis of variance (ANOVA) for normally distributed continuous variables, Kruskal-Wallis test for skewed continuous variables, and the chi-square test for categorical variables. We used multivariate linear regression models for the relationship between BTM levels and total lumbar, total hip, and femur neck BMD levels. Multivariate-adjusted model 1 was adjusted for age, diabetes duration, DM treatment, smoking, drinking, hypertension, cerebrovascular disease, dyslipidemia, kidney disease, and BMI; multivariate-adjusted model 2 was adjusted for age, diabetes duration, DM treatment, smoking, drinking, hypertension, cerebrovascular disease, dyslipidemia, kidney disease, FBG, HbA1C, hsCRP, 25(OH)D, PTH, Ca, Mg, eGFR, and BMI. A two-sided P-value < .05 was considered statistically significant. Statistical analyses were performed using R packages (http://www.r-project.org) and Empower (R) (www.empowerstats.com, X&Y solutions, Inc.).
3 RESULTS
3.1 Characteristics of patients
After excluding patients without serum BTM and BMD data or with repeated hospitalizations (n = 309), a total of 1499 patients with T2DM were included in the analysis. Table 1 shows the characteristics of the patients stratified by men and women. Of the 1499 patients, 884 were men and 615 were women. There were no significant differences between men and women in most of variables except for age, diabetic duration, HbA1C, eGFR, smoking history, drinking history, and hypertension history (all P < .05). In particular, BMD levels in total lumbar, femur neck, and total hip were not different between men and women.
| All patients | Men | Women | Men vs Women (P-value) | |
|---|---|---|---|---|
| N | 1499 | 884 | 615 | |
| Age, year | 58.37 ± 13.19 | 56.19 ± 13.62 | 61.51 ± 11.87 | <.001 |
| Diabetic duration, year | 7.53 ± 6.94 | 6.56 ± 6.54 | 8.92 ± 7.27 | <.001 |
| BMI, kg/m2 | 24.97 ± 3.67 | 24.92 ± 3.60 | 25.04 ± 3.78 | .529 |
| FBG, mmol/L | 8.64 ± 3.06 | 8.66 ± 2.93 | 8.61 ± 3.23 | .732 |
| HbA1C, % | 9.31 ± 2.32 | 9.47 ± 2.31 | 9.09 ± 2.32 | .002 |
| hsCRP, mg/L | 4.72 ± 10.56 | 4.77 ± 10.52 | 4.65 ± 10.63 | .844 |
| TC, mmol/L | 4.58 ± 1.07 | 4.58 ± 1.08 | 4.59 ± 1.05 | .860 |
| TG, mmol/L | 1.90 ± 1.31 | 1.97 ± 1.41 | 1.81 ± 1.15 | .073 |
| HDL-C, mmol/L | 1.12 ± 0.32 | 1.11 ± 0.32 | 1.12 ± 0.32 | .377 |
| LDL-C, mmol/L | 2.64 ± 0.90 | 2.63 ± 0.92 | 2.66 ± 0.89 | .615 |
| PTH, pg/ml | 36.40 ± 14.49 | 36.49 ± 14.63 | 36.26 ± 14.29 | .763 |
| 25(OH)D, nmol/L | 35.26 ± 17.09 | 34.68 ± 17.08 | 36.11 ± 17.08 | .119 |
| Ca, mmol/L | 2.23 ± 0.11 | 2.22 ± 0.12 | 2.23 ± 0.11 | .802 |
| Mg, mmol/L | 0.86 ± 0.09 | 0.85 ± 0.09 | 0.86 ± 0.09 | .090 |
| eGFR, mL/min/1.73 m2 | 103.75 ± 38.17 | 92.47 ± 32.69 | 119.91 ± 39.65 | <.001 |
| Total lumbar BMD, g/cm2 | 0.96 ± 0.16 | 0.96 ± 0.16 | 0.96 ± 0.16 | .890 |
| Femur neck BMD, g/cm2 | 0.76 ± 0.13 | 0.76 ± 0.13 | 0.76 ± 0.13 | .979 |
| Total Hip BMD, g/cm2 | 0.90 ± 0.14 | 0.90 ± 0.14 | 0.90 ± 0.14 | .950 |
| Treatment of DM | ||||
| Diet or newly diagnosed | 218 (14.54%) | 145 (16.40%) | 73 (11.87%) | .089 |
| Insulin | 390 (26.02%) | 229 (25.90%) | 161 (26.18%) | |
| Oral medicine | 600 (40.03%) | 347 (39.25%) | 253 (41.14%) | |
| Insulin and OM | 291 (19.41%) | 163 (18.44%) | 128 (20.81%) | |
| Smoking | ||||
| Never | 1101 (73.45%) | 499 (56.45%) | 602 (97.89%) | <.001 |
| Current or ever | 398 (26.55%) | 385 (43.55%) | 13 (2.11%) | |
| Drinking | ||||
| Never | 1310 (87.39%) | 701 (79.30%) | 609 (99.02%) | <.001 |
| Current or ever | 189 (12.61%) | 183 (20.70%) | 6 (0.98%) | |
| Hypertension | ||||
| No | 718 (47.90%) | 464 (52.49%) | 254 (41.30%) | <.001 |
| Yes | 781 (52.10%) | 420 (47.51%) | 361 (58.70%) | |
| Cerebrovascular disease | ||||
| No | 1347 (89.86%) | 792 (89.59%) | 555 (90.24%) | .681 |
| Yes | 152 (10.14%) | 92 (10.41%) | 60 (9.76%) | |
| Dyslipidemia | ||||
| No | 1230 (82.05%) | 727 (82.24%) | 503 (81.79%) | .823 |
| Yes | 269 (17.95%) | 157 (17.76%) | 112 (18.21%) | |
| Kidney disease | ||||
| No | 1361 (90.79%) | 807 (91.29%) | 554 (90.08%) | .426 |
| Yes | 138 (9.21%) | 77 (8.71%) | 61 (9.92%) | |
- Abbreviations: 25(OH)D, 25-hydroxyvitamin D; BMD, bone mineral density; BMI, body mass index; Ca, calcium; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; FBG, fasting blood glucose; HbA1C, glycosylated hemoglobin; HDL-C, high-density lipoprotein cholesterol; hsCRP, high-sensitivity C reactive protein; LDL-C, low-density lipoprotein cholesterol; Mg, magnesium; OM, oral medicine; PTH, parathyroid hormone; SD, standard deviation; TC, total cholesterol; TG, triglyceride.
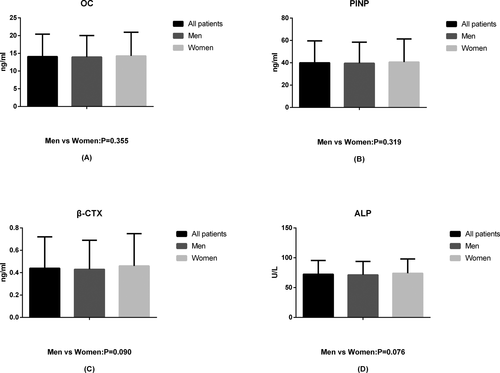
Serum levels of BTMs were also similar in men and women (all P > .05), which are shown in Figure 1.
3.2 The relationship between bone turnover and BMD in multivariate linear regression models
Tables 2-5 show the multivariate regression for effect of serum levels of BTMs (per SD increase) on different sites of BMD levels. We also divided men and women into <55 years old and ≥55 years old after adjusting for the factors in model 2 except for age (Table S5). We also added results of the multivariate regression for effect of BTMs (in quartiles) on BMD in Tables S1-S4.
| OC, ng/mL Per SD | Crude model | Multivariate-adjusted model 1 | Multivariate-adjusted model 2 | |||
|---|---|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | β (95% CI) | P | |
| Total lumbar BMD, g/cm2 | ||||||
| All patients | −0.030 (−0.038, −0.022) | <.001 | −0.030 (−0.038, −0.022) | <.001 | −0.038 (−0.047, −0.028) | <.001 |
| Men | −0.032 (−0.042, −0.021) | <.001 | −0.032 (−0.043, −0.021) | <.001 | −0.039 (−0.052, −0.025) | <.001 |
| Women | −0.029 (−0.041, −0.017) | <.001 | −0.028 (−0.041, −0.016) | <.001 | −0.036 (−0.051, −0.021) | <.001 |
| Femur neck BMD, g/cm2 | ||||||
| All patients | −0.023 (−0.030, −0.017) | <.001 | −0.023 (−0.030, −0.016) | <.001 | −0.026 (−0.034, −0.017) | <.001 |
| Men | −0.025 (−0.034, −0.015) | <.001 | −0.025 (−0.034, −0.015) | <.001 | −0.025 (−0.037, −0.014) | <.001 |
| Women | −0.022 (−0.032, −0.012) | <.001 | −0.022 (−0.032, −0.011) | <.001 | −0.025 (−0.037, −0.012) | <.001 |
| Total hip BMD, g/cm2 | ||||||
| All patients | −0.029 (−0.036, −0.022) | <.001 | −0.029 (−0.036, −0.022) | <.001 | −0.036 (−0.044, −0.027) | <0.001 |
| Men | −0.029 (−0.039, −0.020) | <.001 | −0.030 (−0.040, −0.021) | <.001 | −0.036 (−0.048, −0.025) | <0.001 |
| Women | −0.029 (−0.039, −0.018) | <.001 | −0.028 (−0.039, −0.017) | <.001 | −0.033 (−0.047, −0.020) | <0.001 |
Notes
- Crude model adjusts for none.
- Multivariate-adjusted model 1 adjusts for age; diabetic duration; treatment of DM; smoking; drinking; hypertension; cerebrovascular disease; dyslipidemia; kidney disease; BMI.
- Multivariate-adjusted model 2 adjusts for age; diabetic duration; treatment of DM; smoking; drinking; hypertension; cerebrovascular disease; dyslipidemia; kidney disease; FBG; HbA1C; hsCRP; PTH; 25(OH)D; Ca; Mg; BMI; eGFR.
- Abbreviations: 25(OH)D, 25-hydroxyvitamin D; BMD, bone mineral density; BMI, body mass index; Ca, calcium; CI, confidence interval; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; FBG, fasting blood glucose; HbA1C, glycosylated hemoglobin; hsCRP, high-sensitivity C reactive protein; Mg, magnesium; OC, osteocalcin; PTH, parathyroid hormone; SD, standard deviation.
| P1NP, ng/mL Per SD | Crude model | Multivariate-adjusted model 1 | Multivariate-adjusted model 2 | |||
|---|---|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | β (95% CI) | P | |
| Total lumbar BMD, g/cm2 | ||||||
| All patients | −0.029 (−0.037, −0.020) | <.001 | −0.028 (−0.036, −0.020) | <.001 | −0.030 (−0.039, −0.020) | <.001 |
| Men | −0.032 (−0.043, −0.021) | <.001 | −0.031 (−0.043, −0.020) | <.001 | −0.036 (−0.049, −0.023) | <.001 |
| Women | −0.024 (−0.037, −0.012) | <.001 | −0.024 (−0.037, −0.011) | <.001 | −0.021 (−0.035, −0.007) | .003 |
| Femur neck BMD, g/cm2 | ||||||
| All patients | −0.021 (−0.028, −0.014) | <.001 | −0.021 (−0.028, −0.014) | <.001 | −0.022 (−0.030, −0.014) | <.001 |
| Men | -0.027 (−0.036, −0.018) | <.001 | −0.027 (−0.036, −0.017) | <.001 | −0.030 (−0.041, −0.019) | <.001 |
| Women | −0.014 (−0.024, −0.003) | .010 | −0.013 (−0.024, −0.003) | .014 | −0.011 (−0.023, 0.000) | .058 |
| Total hip BMD, g/cm2 | ||||||
| All patients | −0.026 (−0.033, −0.019) | <.001 | −0.026 (−0.033, −0.018) | <.001 | −0.028 (−0.036, −0.020) | <.001 |
| Men | −0.031 (−0.041, −0.022) | <.001 | −0.031 (−0.041, −0.022) | <.001 | −0.037 (−0.048, −0.025) | <.001 |
| Women | −0.019 (−0.030, −0.008) | <.001 | −0.019 (−0.030, −0.008) | .001 | −0.016 (−0.029, −0.004) | .010 |
Notes
- Crude model adjusts for none.
- Multivariate-adjusted model 1 adjusts for age; diabetic duration; treatment of DM; smoking; drinking; hypertension; cerebrovascular disease; dyslipidemia; kidney disease.
- BMI Multivariate-adjusted model 2 adjusts for age; diabetic duration; treatment of DM; smoking; drinking; hypertension; cerebrovascular disease; dyslipidemia; kidney disease; FBG; HbA1C; hsCRP; PTH; 25(OH)D; Ca; Mg; BMI; eGFR.
- Abbreviations: 25(OH)D, 25-hydroxyvitamin D; BMD, bone mineral density; BMI, body mass index; Ca, calcium; CI, confidence interval; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; FBG, fasting blood glucose; HbA1C, glycosylated hemoglobin; hsCRP, high-sensitivity C reactive protein; Mg, magnesium; P1NP, N-terminal propeptides of type 1 collagen; PTH, parathyroid hormone; SD, standard deviation.
| β-CTX, ng/mL Per SD | Crude model | Multivariate-adjusted model 1 | Multivariate-adjusted model 2 | |||
|---|---|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | β (95% CI) | P | |
| Total lumbar BMD, g/cm2 | ||||||
| All patients | −0.030 (−0.038, −0.022) | <.001 | −0.029 (−0.038, −0.021) | <.001 | −0.029 (−0.038, −0.019) | <.001 |
| Men | −0.036 (−0.047, −0.025) | <.001 | −0.035 (−0.046, −0.023) | <.001 | −0.033 (−0.047, −0.020) | <.001 |
| Women | −0.023 (−0.036, −0.011) | <.001 | −0.023 (−0.036, −0.010) | <.001 | −0.024 (−0.038, −0.010) | <.001 |
| Femur neck BMD, g/cm2 | ||||||
| All patients | −0.013 (−0.020, −0.005) | <.001 | −0.012 (−0.019, −0.005) | .001 | −0.011 (−0.019, −0.003) | .008 |
| Men | −0.020 (−0.030, −0.011) | <.001 | −0.019 (−0.029, −0.009) | <.001 | −0.017 (−0.028, −0.005) | .005 |
| Women | −0.004 (−0.015, 0.007) | .469 | −0.004 (−0.014, 0.007) | .525 | −0.005 (−0.017, 0.007) | .393 |
| Total hip BMD, g/cm2 | ||||||
| All patients | −0.020 (−0.028, −0.013) | <.001 | −0.020 (−0.027, −0.012) | <.001 | −0.021 (−0.029, −0.012) | <.001 |
| Men | −0.028 (−0.039, −0.018) | <.001 | −0.028 (−0.038, −0.017) | <.001 | −0.029 (−0.041, −0.017) | <.001 |
| Women | −0.011 (−0.022, 0.000) | .056 | −0.010 (−0.022, 0.002) | .094 | −0.012 (−0.025, 0.000) | .054 |
Notes
- Crude model adjusts for none.
- Multivariate-adjusted model 1 adjusts for age; diabetic duration; treatment of DM; smoking; drinking; hypertension; cerebrovascular disease; dyslipidemia; kidney disease.
- BMI Multivariate-adjusted model 2 adjusts for age; diabetic duration; treatment of DM; smoking; drinking; hypertension; cerebrovascular disease; dyslipidemia; kidney disease; FBG; HbA1C; hsCRP; PTH; 25(OH)D; Ca; Mg; BMI; eGFR.
- Abbreviations: 25(OH)D, 25-hydroxyvitamin D; BMD, bone mineral density; BMI, body mass index; Ca, calcium; CI, confidence interval; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; FBG, fasting blood glucose; HbA1C, glycosylated hemoglobin; hsCRP, high-sensitivity C reactive protein; Mg, magnesium; PTH, parathyroid hormone; SD, standard deviation; β-CTX, C-terminal telopeptides of type Ⅰ collagen.
| ALP, U/L Per SD | Crude model | Multivariate-adjusted model 1 | Multivariate-adjusted model 2 | |||
|---|---|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | β (95% CI) | P | |
| Total lumbar BMD, g/cm2 | ||||||
| All patients | −0.024 (−0.032, −0.016) | <.001 | −0.024 (−0.032, −0.016) | <.001 | −0.024 (−0.033, −0.015) | <.001 |
| Men | −0.024 (−0.035, −0.014) | <.001 | −0.023 (−0.034, −0.012) | <.001 | −0.026 (−0.038, −0.013) | <.001 |
| Women | −0.025 (−0.037, −0.012) | <.001 | −0.025 (−0.038, −0.012) | <.001 | −0.023 (−0.037, −0.009) | .001 |
| Femur neck BMD, g/cm2 | ||||||
| All patients | −0.017 (−0.024, −0.010) | <.001 | −0.017 (−0.024, −0.010) | <.001 | −0.017 (−0.024, −0.009) | <.001 |
| Men | −0.018 (−0.027, −0.009) | <.001 | −0.018 (−0.027, −0.009) | <.001 | −0.020 (−0.031, −0.010) | <.001 |
| Women | −0.015 (−0.026, −0.005) | .003 | −0.014 (−0.025, −0.004) | .008 | −0.010 (−0.022, 0.002) | .090 |
| Total hip BMD, g/cm2 | ||||||
| All patients | −0.020 (−0.027, −0.013) | <.001 | −0.020 (−0.028, −0.013) | <.001 | −0.022 (−0.030, −0.014) | <.001 |
| Men | −0.023 (−0.033, −0.014) | <.001 | −0.024 (−0.034, −0.014) | <.001 | −0.029 (−0.039, −0.018) | <.001 |
| Women | −0.016 (−0.027, −0.005) | .004 | −0.016 (−0.027, −0.005) | .006 | −0.011 (−0.023, 0.002) | .095 |
Notes
- Crude model adjusts for none.
- Multivariate-adjusted model 1 adjusts for age; diabetic duration; treatment of DM; smoking; drinking; hypertension; cerebrovascular disease; dyslipidemia; kidney disease; BMI.
- Multivariate-adjusted model 2 adjusts for age; diabetic duration; treatment of DM; smoking; drinking; hypertension; cerebrovascular disease; dyslipidemia; kidney disease; FBG; HbA1C; hsCRP; PTH; 25(OH)D; Ca; Mg; BMI; eGFR.
- Abbreviations: 25(OH)D, 25-hydroxyvitamin D; ALP, alkaline phosphatase; BMD, bone mineral density; BMI, body mass index; Ca, calcium; CI, confidence interval; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; FBG, fasting blood glucose; HbA1C, glycosylated hemoglobin; hsCRP, high-sensitivity C reactive protein; Mg, magnesium; PTH, parathyroid hormone; SD, standard deviation.
3.2.1 The relationship between bone turnover and BMD
Osteocalcin was recently considered to be a serum marker of bone turnover levels. Table 2 shows the relationship between OC and BMD levels after adjusting for factors in the three kinds of models (crude model, model 1, and model 2), which were previously described.
In men with T2DM, each SD increase in OC was significantly related to a decrease in BMD in all sites (total lumbar, femur neck, and total hip), which showed consistent results in the three models (model 2; total lumbar, β = −0.039, 95% CI = −0.052 to −0.025, P < .001; femur neck, β = −0.025, 95% CI = −0.037 to −0.014, P < .001; and total hip, β = −0.036, 95% CI = −0.048 to −0.025, P < .001). The negative correlation was maintained when men were divided into <55 years old and ≥55 years old after adjusting for the factors in model 2 except for age (Table S5).
In women with T2DM, each SD increase in OC was still associated with decreased BMD levels of all three sites in the three models (all P < .05). When we divided women into <55 years old and ≥ 55 years old, the results remained significant except for the relationship between the femoral neck and BMD levels in women <55 years old (Table S5).
3.2.2 The relationship between bone formation and BMD
Tables 3 and 5 show the relationship between serum bone formation markers (P1NP, ALP) and BMD levels after adjustment for factors in three kinds of models.
In men with T2DM, each SD increase in these two kinds of BTMs (P1NP and ALP) related to bone formation was negatively associated with BMD in all sites (all P < .05), which was consistent for all three models. The negative correlation was maintained when men were divided into < 55 years old and ≥ 55 years old, except in relationship between ALP and femur neck BMD in men < 55 years old (Table S5).
In women with T2DM, each SD increase in P1NP and ALP was related to lower BMD levels in three models (model 2; P1NP, β = −0.021, 95% CI = −0.035 to −0.007, P = .003; ALP, β = −0.023, 95% CI = −0.037 to −0.009, P = .001) for total lumbar. Each SD increase in P1NP and ALP for the femoral neck was not significantly negatively related to BMD levels after adjusting for the factors in model 2 despite the results being significant in crude model and model 1. In total hip, higher serum levels of P1NP were related to lower BMD levels (model 2; β = −0.016, 95% CI = −0.029 to −0.004, P = .010), while ALP was no longer significant in model 2. When women were divided into < 55 years old and ≥ 55 years old, the results differed between the two groups. In women ≥ 55 years old, each SD increase in P1NP and ALP correlated significantly with lower levels of BMD in total lumbar and total hip, while in femoral neck, there was a relationship with ALP but not for P1NP. In women <55 years old, conversely, the relationship was only significant in P1NP with BMD levels in total lumbar (Table S5).
3.2.3 The relationship between bone resorption and BMD
Table 4 showed the relationship between serum bone resorption marker (β-CTX) and BMD levels after adjusting for factors in the three kinds of models.
In men with T2DM, each SD increase in β-CTX was negatively associated with BMD in all sites (all P < .05) in three models. The negative correlation was maintained when men were divided on the basis of age into <55 years and ≥ 55 years, except in the relationship between β-CTX and femoral neck BMD in men both <55 years old and ≥55 years old (Table S5).
In women with T2DM, higher levels of β-CTX were found to be negatively related only to total lumbar BMD in three models (model 2; β = −0.024, 95% CI = −0.038 to −0.010, P < .001). In the femoral neck and total hip, the relationship was insignificant in three models (all P > .05). When women were divided into <55 years old and ≥55 years old, the results again varied between the two groups. In women ≥ 55 years old, the results were similar as the results for all women. In women <55 years old, there was no significant association between any sites with β-CTX (Table S5).
4 DISCUSSION
In this hospital-based, cross-sectional study, OC indicating bone turnover levels was negatively correlated with all three sites and BMD levels in men and women. For bone formation markers, after adjusting for potential confounding factors, P1NP and ALP showed a consistently negative association with total lumbar, femur neck, total hip BMD in men, and total lumbar BMD in women, while in women in terms of femur neck and total hip, the relationship was only observed in P1NP with total hip. For bone resorption markers in terms of β-CTX, the results were also consistently negative in all three sites for BMD in men and total lumbar BMD in women, while in women, β-CTX was not associated with the femur neck and total hip. We also further analyzed the relationship between BTMs and BMD in patients <55 and ≥55 years old. In men, consistent results were observed in the two groups, in which a negative relationship was shown. Menopause and levels of sex hormones influence on female bone metabolism. However, it is unfortunate that due to logistical reasons there were insufficient related data for analysis. So according to previous researches,27-30 to further analyze the relationship between BTMs and BMD in women with T2DM, we divided women into <55 years old which might be premenopausal, and ≥55 years old which might be postmenopausal. In particular, results obviously varied between women < 55 and ≥55 years old. In women <55 years old, the relationship was hardly shown, while in women ≥55 years old, despite the fact that a relationship was shown with the four BTMs with total lumbar BMD, the results were varied in femur neck and total hip BMD.
There were several previous studies on the relationship between BTMs and BMD in patients with T2DM, even though the results remain controversial. In terms of bone formation, it has already been proposed that P1CP could be a determinant of bone mass.19 However, it was also reported that no correlation between P1CP and BMD in femoral neck and lumbar spine exists in T2DM patients.21 And several other studies also revealed that the concentration of bone formation markers might be not associated with BMD levels in T2DM. In 137 diabetic hemodialysis patients, bone formation markers failed to show a negative relationship between P1NP and BMD.23 The results were consistent for P1NP in 46 postmenopausal Japanese women with T2DM.22 Other markers, such as ALP or bone-specific ALP, no correlation was found in three studies, although the sample sizes were small.17, 18, 25 In our results, serum levels of P1NP and ALP were negatively associated with BMD levels in men and women except that the results varied in women for femur neck and total hip. In accordance with our results, bone ALP was proven to be a predictor of BMD reduction in hemodialysis patients with diabetes.23 Additionally, ALP was negatively correlated with femoral neck BMD in 890 postmenopausal Chinese patients with T2DM.12 In terms of bone resorption, the results were also controversial. In postmenopausal Japanese women with T2DM, CTX was not related to BMD levels.22 The same relationship was also shown in diabetic hemodialysis patients.23 In 32 Japanese patients with T2DM, NTX was not related to any sites and changes in BMD even after adjusting for age, duration of diabetes, sex, body height, weight, waist circumference, serum creatinine, and HbA1c.18 However, in our present study, we also made several models for multiple adjustments and had a relatively larger sample size. It demonstrated that in women with femur neck and total hip, β-CTX was also not related to BMD levels even after patients were stratified according to <55 and ≥55 years old. In men, a negative correlation was found for all three sites and this negative correlation was found in women for total lumbar. This negative relationship was also supported by research including 890 postmenopausal Chinese patients with T2DM wherein urinary NTX/creatinine was significantly negatively related to BMD in the lumbar spine, femoral neck, trochanter, and the Ward triangle.12 In another cross-sectional study that included T2DM men and women, CTX was found to be inversely related to BMD levels in the femoral neck, total hip, and lumbar spine.24 OC was considered to represent bone turnover levels (both bone formation and bone resorption levels) in recent years; however, previous studies also declared varied relationship between OC and BMD levels. Some studies considered there was no significant relationship between them.18, 21, 23 However, in a prospective cohort of elderly women, OC was negatively correlated with BMD levels in a stepwise regression analysis, though these sites were the radius and phalanx, which are not the main sites used for bone health evaluation.20 The same negative relation was also shown in another study.17 In our present results, OC was consistently related to lower BMD levels in men and women in total lumbar, total hip, and femur neck. On the contrary, in 890 postmenopausal Chinese patients with T2DM, OC was positively related to BMD in the hip and lumbar spine. However, in our study, the negative relationship was concluded through a multivariate linear regression model, and both men and women were included. In summary, we reported that BTMs were negatively related to BMD levels in different sites, which was in accordance with a part of previous study results, but was still controversial. Further intensive analysis should be conducted in the future.
In our multivariate regression analysis, we adjusted for several related factors that might influence the judgment of the relationship between BTM and BMD levels. In particular, we adjusted 25(OH)D and PTH in model 2 and presented the relationship between BTMs and BMD independent of these two factors. Vitamin D is supposed to play pleiotropic roles in bone metabolism,31 and low PTH levels are related to decreased bone formation.32
From our results, with the increase in serum levels of BTMs, the degree of changes in BMD levels tended to vary in different sites in a central way (total lumbar > total hip > femur neck). First, it might be associated with variations in different sites of bones in diabetic patients. Compared with non-diabetic people, patients with T2DM tended to have higher BMD levels in a central fashion (spine > hip>femoral neck possibly).3, 33 Second, the results may be associated with different proportions of cortical and trabecular bone in different sites. It was inferred that bone metabolism in diabetic patients has a stronger association with trabecular bone than cortical bone according to our results, which was also found similarly in another study.34 However, some other studies reported an opposite tendency.35, 36 More data are needed to further clarify variation in bone metabolism in the different sites in patients with T2DM.
Moreover, the differences between men and women were shown in our study. In men with total lumbar, femur neck, and total hip, the relationship between BTM and BMD levels was consistently shown; however, the results varied in women with femur neck and total hip despite the significant results in total lumbar BMD. The first possible reason for explaining this difference might be sex hormones, especially estrogen, which plays important roles in both bone formation and bone resorption. Estrogen can suppress osteoblast apoptosis and prolong their lifespan.37 It also regulates gene expression, proliferation, and differentiation of osteoblasts.38 Estrogen also inhibits bone resorption by reduction in osteoclastogenesis39 and regulation of the lifecycle of mature osteoclasts.40 It can therefore be inferred that in women with T2DM, the relationship between BTMs and BMD might be influenced by sex hormones. It is unfortunate that there were insufficient data for the serum levels of sex hormones due to logistical reasons and we could not evaluate their effect in this study. However, our results obviously varied between women < 55 and ≥55 years old. In women <55 years old, the relationship was hardly shown, while in women ≥55 years old, the results still varied in the femur neck and total hip BMD; thus, the presence of sex hormones might be not enough to clarify this issue even though the relationship was shown in four BTMs with total lumbar BMD. Another possible reason might be that bone structures and metabolism vary according to gender. It was supposed that the process of hip geometry impairment differed in women and men, which was that women showed more impaired bone structure with aging compared to men in the femoral neck and intertrochanteric region.41 Additionally, though the results varied in women with total hip and femur neck, it was notable that the relationship in P1NP (with femur neck BMD) and ALP (with total hip and femur neck BMD) was not significant even after adjusting for the factors in model 2 even though the results were significant in the crude model and model 1. In addition, we further adjusted for glycemia status including HbA1C and FBG levels among the adjusted factors in model 2. It was reported in a previous study that in women alone, impaired glucose tolerance and T2DM were negatively related to bone mineralization and bending strength.42 Consequently, explicit reasons and mechanisms were not defined in the current data; thus, more studies are needed to further analyze differences according to gender in the future.
However, this study still has some limitations. First, our study is a retrospective, cross-sectional study; thus, a causal relationship could not be obtained. Second, among enrolled patients in our study, the number of patients with history of fractures was very small, which cannot be our outcome factor in multivariate regression analysis in this study. BMD was generally considered as an important factor for evaluation of risk of fractures, which might help us in early treatment of impaired bone health and early prevention of bone fractures. Before carrying out our study, our research team have made a careful discussion and considered it was suitable to take BMD as our outcome factor. However, in order to directly evaluate the incidence of fractures and further examine our results, we plan to take up a large sample size cohort study in the future. Third, some confounding variables were possibly omitted due to logistical reasons, such as serum levels of some sex hormones, thyroid hormones, and adrenal hormones, which may also have some effects on BTMs and BMD. Fourth, the type of oral antidiabetic therapy also partly influences on our results; however, not all of patients can provide all details of antidiabetic drugs they used. In order to avoid recall bias, we did not take this factor into our multivariate analysis. Nonetheless, our study included 1499 men and women with T2DM, which is a big sample size. Moreover, we showed an elaborate analysis of different BTMs and different sites of BMD levels. Furthermore, in our multivariate linear regression analysis, we presented the relationship between BTMs and BMD independent of 25(OH)D and PTH.
In conclusion, increased serum levels of OC, P1NP, β-CTX, and ALP were correlated with decreased BMD levels independent of 25(OH)D and PTH in men with three sites and women with total lumbar BMD, while the relationship varied in women with femur neck or total hip BMD.
ACKNOWLEDGMENTS
No current funding source was received.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AUTHOR CONTRIBUTIONS
The authors’ responsibilities were as follows—QXH and YMX designed the research; ZCH, LJing, YYQ, and QXH conducted the research; XGP, ZY, YXL, LJing, YYQ, and YYL provided the essential materials; ZCH, LGW, and QXH analyzed the data or performed the statistical analyses; ZCH and LGW wrote the article; LGW, LJun, MC, QXH, and YMX critically revised the article.