Research status and prospect of peri-extubation delirium
Abstract
Peri-extubation delirium is a clinical syndrome caused by multiple factors, and it is not a simple disease. It occurs within a period of time after extubation when the effect of general anesthesia is reduced. And the incidence is different in disparate populations, and it is more common in elderly patients. Current studies have shown that iatrogenic factors and patients' own factors are the main risk factors for the syndrome. Early identification of risk factors can help clinicians make early diagnosis. The earlier the diagnosis and treatment begin, the more significantly the prognosis of patients can be improved. At present, the treatment of perioperative delirium is based on non-drug therapy, supplemented by drug therapy. This review will introduce in detail the risk factors, population status and prevention measures of delirium during peri-extubation, and look forward to the new research direction in the future.
Introduction
Delirium is an etiologically non-specific acute brain syndrome, which is characterized by disorders of body consciousness, attention, perception, memory, thinking, mood and sleep cycle, abnormal psychomotor behavior, and the duration can be long or short, the severity can be light or severe (Aldecoa, et al., 2017). Peri-extubation delirium refers to the symptoms of delirium after general anesthesia, which mainly occurs at the end of the operation after the anesthetic effect is reduced to extubation for a period of time, with relatively clear time characteristics. Peri-extubation delirium can be divided into mental inhibition type: decreased alertness, reduced activity and lack of pleasure, mental excitement type: agitation and belligerence, or a mixture of the two symptoms. Among them, the prognosis of inhibitory delirium is relatively poor, which may be related to the delay of treatment due to the fact that its symptoms are not easy to attract the attention of medical staff (Aldecoa, et al., 2017). How to make the patient go through the peri-extubation period smoothly and avoid the occurrence of delirium will be a great challenge for anesthesiologists. This article will review the research status and future research direction of delirium during peri-extubation, in order to provide reference for clinical prevention and treatment in the future. The flow chart of this article in Figure 1.

The flow chart of this review
Risk factors
The related risk factors of peri-extubation delirium include many factors, such as iatrogenic factors and patients' own conditions, among which age and preoperative cognitive impairment are known independent risk factors (Zaal, et al., 2015). If the patient has peri-extubation delirium, if there is no timely intervention, it may evolve into secondary cognitive impairment, resulting in further loss of body function and socio-economic loss. Therefore, the risk factors of delirium should be evaluated and appropriate preventive and therapeutic measures should be taken.
Iatrogenic factors
The occurrence of delirium is the result of the joint action of many factors, in which iatrogenic factors play a leading role. Accurate identification of iatrogenic factors, active correction of inducement and effective intervention against risk factors are important prerequisites for the prevention of peri-extubation delirium, which can significantly reduce the incidence of peri-extubation delirium.
Type of operation
Delirium is a common and serious complication after extensive surgery, different types of surgery cause different injuries to patients, and the incidence of delirium during peri-extubation is also different, and the incidence increases with the increase of surgical risk. In a study involving 293 patients, Booka E et al found delirium in 17.1% of patients undergoing major head and neck surgery (Booka, et al., 2016), the incidence of delirium in hip fracture surgery was 10 - 50% (Lee, et al., 2011), incidence of delirium after cardiac surgery reached 20 - 30 % (Lopez, et al., 2017), incidence of spinal surgery over 15% (Tan, et al., 2011), and when the prognostic nutritional index < 49.7 and age > 68.5, we should be alert to the occurrence of peri-extubation delirium after spinal surgery (Oe, et al., 2019), the study also found that prolonged operation time and general anesthesia were associated with peri-extubation delirium (Ravi, et al., 2019).
Hospital environment
Hospital environment is characterized by strangeness (especially when patients wake up from anesthesia), tension and confusion (noise, light, etc) (Liu, et al., 2020). Special hospital environment can lead to disorder of sleep-wake cycle and induce delirium. Noise and light are very important factors (Malas, et al., 2017). World Health Organization (WHO) recommended that hospital daytime noise levels should be less than 35 decibels and nighttime noise levels should be less than 30 decibels, China's Ministry of Health Comprehensive Medical Management Standard (Trial) stipulates that operating room noise should be less than 38 decibels (Wang, et al., 2012), but the actual peak noise level often exceeds 90 decibels (Kawai, et al., 2019). Reducing noise can reduce anxiety and fear, intraoperative crisis and postoperative complications in patients undergoing surgery (Wang, et al., 2012). In addition, continuous lighting makes it difficult for patients to distinguish between daytime and nighttime turnover, which is also an important cause of delirium (Wei, et al., 2019), sleep-wake cycle disorder is one of the core characteristics of delirium, which is exacerbated by complex hospital environments and forms a vicious cycle. Other researchers measured particulate matter (PM) in hospital ambient air and found that short-term exposure to PM 2.5 (fine particles, particles with aerodynamic equivalent diameter ≤ 2.5μm) > 47.5μg/m3 ambient air on the day of surgery increased the incidence of delirium in surgical populations during hospitalization (Che, et al., 2017).
Premedication
Penehyclidine hydrochloride, as a new type of anticholinergic drug, has been widely used in the perioperative period. However, with the expansion of its application, the problems are gradually increasing. Perioperative use of penehyclidine hydrochloride increases the incidence of postoperative cognitive dysfunction and postoperative mental disorders in elderly patients with lung cancer undergoing thoracoscopic surgery under general anesthesia (Hong, et al., 2019). The results of this study suggest that the clinical application of penehyclidine hydrochloride should be carefully evaluated to maximize its efficacy.
Perioperative hypoperfusion
Previous studies have found that intraoperative hypotension (< 80 mmHg) is considered a valuable predictor of delirium (Jiang, et al., 2017). However, Clemmesen CG et al in a prospective study on the measurement of regional cerebral oxygen saturation (RSO2) before and during recovery found that in elderly patients undergoing hip fracture surgery, compared with blood pressure measurement, preoperative RSO2 < 55%, lasting at least 2 minutes (min) had a better correlation with 30 days (d) mortality (Clemmesen, et al., 2017). A total of 40 elderly patients with hip fracture (age > 65 years) were included in this study, 10 patients (25%) had low RSO2 during recovery period, and postoperative delirium occurred within 7 d before operation. It is suggested that more attention should be paid to the perfusion of important organs in the preoperative and peri-extubation study of general anesthesia in patients with hip fracture, rather than limited to traditional hemodynamics.
Anesthesia factor
It has been reported that in elderly patients over 65 years old who received general anesthesia or subarachnoid anesthesia respectively, the choice of anesthesia methods does not seem to affect the occurrence of postoperative delirium in elderly patients with hip fracture surgery (Tzimas, et al., 2018). This study shows that anesthesia is not a risk factor for peri-extubation delirium, but anesthesia is accepted and is related to the selection of anesthetic drugs. Goins AE et al found in a study on transcatheter aortic valve replacement under general anesthesia that total intravenous anesthesia can reduce peri-extubation delirium compared with volatile anesthetics, suggesting that total intravenous anesthesia may be an attractive alternative to volatile anesthetics (Goins, et al., 2018). Anesthesia exhaust gas will be produced during the use of inhaled anesthetics. Exposure to anesthesia exhaust gas can increase the risk of anxiety among medical staff (Qian, et al., 2017). Similarly, patients and medical staff exposed to the same environment, the risk of anxiety increased, and the incidence of peri-extubation delirium increased. Therefore, actively improving the air environment in the operating room and taking effective protective measures are conducive to ensuring the physical and mental health of medical staff and patients. Patients may experience inadequate recovery after general anesthesia, which will prolong hospital stay and increase the incidence of postoperative complications. Longer anesthesia time, inhalation anesthesia time and ASA ≥ III were significantly associated with inadequate recovery (Wiinholdt, et al., 2018). Other studies have confirmed that the faster the anesthesia wakes up, the higher the incidence of peri-extubation delirium, and the incidence of delirium will decrease by 7% for every 1 min extension of the wake-up time (Bong, et al., 2015).
Patient factors
Although delirium is reversible, the adverse prognosis following the occurrence of delirium is difficult to reverse. The patient’ s own conditions are the basic conditions for determining whether the patient can reverse delirium. If there are patients with related comorbidities before surgery, the probability of peri-extubation delirium also increases.
Preoperative cognitive impairment
In a clinical trial of 317 veterans with post-traumatic stress disorder (PTSD), Umholtz M et al found that 15 (4.7%) of the 317 veterans had delirium after anesthesia, and their postoperative recovery was lower than expected, indicating that PTSD independently predicted the occurrence of delirium. In addition, the study also found that the post anesthesia care unit (PACU) stay time of PTSD patients was relatively long, which may reflect the increased awareness of medical staff of this debilitating mental disorder (Umholtz, et al., 2016). The preoperative mental health declines, and the postoperative quality of life will also deteriorate, so preoperative mental health screening is very important (Watanabe, et al., 2020).
Alcohol dependence
The WHO pointed out that drinking 53° liquor and drinking up to 240 ml is “very dangerous drinking” (Zhu, et al., 2017). However, Chinese wine culture permeates the entire 5,000 years history of Chinese civilization and occupies an important position in daily life. Personal drinking is far more than that. Based on this, Chinese researchers believe that preoperative symptoms of alcohol dependence will increase the incidence of peri-extubation delirium in elderly patients after surgery (Zhu, et al., 2017).
Preoperative comorbidities
Studies have shown that thoracic surgery patients with obstructive sleep apnea syndrome before surgery are more likely to experience confusion and coma after surgery, leading to longer hospital stays (Wang, et al., 2018). Preoperative anxiety has a strong predictive effect on the occurrence of postoperative delirium, and preventing preoperative anxiety may become a new target for preventing postoperative delirium (Wada, et al., 2019).
Research status of different ages
Peri-extubation delirium is a common postoperative complication. From children to the elderly, it can occur in all age groups, and the incidence of each age group is not the same. Current research shows that the incidence of delirium in elderly patients is higher.
Children
Before general anesthesia, it is necessary to go through fasting for as short as 2 hours (h) and as long as 8 h. On the operation days when there are more elective operations, the fasting time is longer. Long-term hunger will breed preoperative anxiety in patients, which is especially significant in children. With the prolongation of the preoperative fasting and drinking time, the anxiety of the children will become more and more obvious, which will eventually lead to the occurrence of delirium in the peri-extubation period. Some literature points out that it is safe and feasible to drink clear drink (clear water, 5 % glucose solution) 2 h before elective surgery, which can effectively reduce children's hunger and thirst, relieve preoperative anxiety, and effectively reduce the occurrence of delirium during the peri-extubation period of general anesthesia (Lu, et al., 2019). Preoperative visits to the operating room, use of the game room, VR games, effective analgesia, no short-acting volatile anesthetic application, and parental companionship during the recovery process can minimize the occurrence of preoperative anxiety. In peri-extubation period to improve the degree of awakening of children and reduce the occurrence of delirium (Hayhoe, et al., 2018, Zhong, et al., 2018, Eijlers, et al., 2019). For children undergoing eye surgery, the use of visual preconditioning (covering the eye to be operated with an eye mask for ≥ 3 h on the day before the operation) can effectively reduce the occurrence of delirium, anxiety and pain during the peri-extubation period (Lin, et al., 2018, Pan, et al., 2018).
Prevention of delirium during peri-extubation is still an important challenge in the field of pediatric anesthesia. The early negative behaviors of children after general anesthesia include sudden delirium and acute pain, which are difficult to distinguish in a short time, but the treatment strategies of the two are completely different. In a retrospective analysis, the researchers found that children with peri-extubation delirium after general anesthesia showed “no eye contact” and “not aware of the surrounding environment”, while “abnormal facial expressions” and “crying” “Sadness” indicates that the child has acute pain in the early postoperative period (Somaini, et al., 2016). Therefore, in clinical work, anesthesiologists need to more carefully observe the status of the child during the entire peri-extubation period in order to perform personalized treatment more timely and accurately. Kim J et al found that during the peri-extubation period of general anesthesia, the low-frequency (δ) frontal Electroencephalogram (EEG) activity increased, and the high-frequency (α and β) activity decreased, which can predict the occurrence of delirium during the peri-extubation period in children (Kim, et al., 2021).
Elderly patients
As the global population aging crisis further intensifies, the number of elderly patients undergoing surgery continues to increase and their age continues to grow. Delirium is gradually becoming the most common postoperative complication in elderly patients, and it is associated with an increase in postoperative mortality. In Italy, 38% of surgical patients are over 65 years old, and in the United States, those over 65 years old account for half of the surgical patients (Aldecoa, et al., 2017). Old age usually means various complications, such as Alzheimer's disease, depression, cardiovascular and cerebrovascular diseases, metabolic-related diseases, etc, which are all related to the occurrence of delirium. Compared with younger patients, the reason for the increase in postoperative complications in the elderly is preoperative comorbidities, rather than age itself, and preoperative risk assessment must be optimized to reduce complications (Andreozzi, et al., 2020). Early recognition of the disease and multi-dimensional intervention can prevent the occurrence of delirium in the elderly, thereby reducing postoperative mortality and improving the quality of life in later years. The results of multivariate analysis showed that age > 70 years old is an important risk factor for delirium after surgery (Booka, et al., 2016). For patients over 70 years old, special attention should be paid to the possibility of delirium in the first 3 d after surgery. It has been reported in the literature that postoperative serum S100 A12 levels are closely related to inflammation, and are an independent risk factor for postoperative cognitive dysfunction, suggesting that serum S100 A12 can be used as a potential biomarker for predicting postoperative delirium in elderly surgical patients (Li, et al., 2019). Studies have confirmed that a comprehensive review of preoperative medications is essential for postoperative outcomes (such as delirium, death) in elderly patients (Ottesen, et al., 2018). Elderly patients usually have a long-term medication history, which requires the anesthesiologist to be sufficiently familiar with the patient's medical history to ensure the safety of the patient during the peri-anaesthetic period.
Early diagnosis
Knowing the risk factors of peri-extubation delirium can better help clinicians in early diagnosis and timely treatment. Early diagnosis is the key to the treatment of peri-extubation delirium. The European Society of Anesthesiology's postoperative delirium guidelines (Aldecoa, et al., 2017) recommend that patients should be screened regularly from the time they enter the PACU using delirium scoring standards. Once the patient is found to have symptoms of delirium, the cause and symptomatic treatment should be started immediately. The later the treatment is started, the more severe the subsequent cognitive impairment. The Richmond agitation-sedation scale (RASS score) (Table 1) was used in all studies for the immediate postoperative “recovery delirium”, while the pediatric anesthesia emergence delirium scale (Table 2) was commonly used in children. The assessment time of RASS score is short and easy to operate. Medical staff only need simple observation, communication and stimulation to accurately evaluate the patient's sedation state, which can effectively ensure the airway safety of patients with mechanical ventilation and reduce the occurrence of related complications. The use of RASS score for sedation evaluation can prevent the occurrence and progress of delirium. In a multi-center study, it was found that experts who independently assessed exactly the same information had considerable divergence in the classification of delirium, showing the difficulty of the diagnosis of delirium (Numan, et al., 2017). Other scholars through pupil, Glasgow Coma Scale (GCS score), sedation score (Ramsay score), Canadian Neurological Scale (CNS), Nursing Delusional Screening Scale (Nu-DESC) and Bispectral Index Score (BIS) combined application can improve the early detection of PACU neurological complications after elective craniotomy (Herrero, et al., 2017). It is reported in the literature that when the patient stops inhaled anesthetics, 15 min after entering the PACU, and before leaving the PACU, the infrared pupil measurement is performed to observe the pupil reflex and compare the pupil parameters, which can effectively identify the patients with delirium in the PACU (Yang, et al., 2018), so that the patients can be timely effective treatment. In addition, studies have found that specific EEG patterns are related to delirium during the peri-extubation period in PACU (Kim, et al., 2021, Hesse, et al., 2019). The appeal findings provide valuable information for researchers in future studies of the brain's response areas to surgery and anesthesia.
| Score | Performance | Symptom |
|---|---|---|
| 4 | Combative | Violent, immediate danger to staff |
| 3 | Veryagitatd | Pulls or removes tube (tubes) or catheter (catheters); aggressive |
| 2 | Agitated | Frequent non-purposeful movement, fights ventilator |
| 1 | Restless | Anxious, apprehensive but movements not aggressive or vigorous |
| 0 | Alert and calm | |
| -1 | Drowsy | Not fully alert, but has sustained awakening to voice (eye opening and contact for more than or exactly 10 s) |
| -2 | Light sedation | Brieflfly awakens to voice (eye opening and contact for <10 s) |
| -3 | Moderate sedation | Movement or eye opening to voice (but no eye contact) |
| -4 | Deep sedation | No response to voice but movement or eye opening to physical stimulation |
| -5 | Unrousable | No response to voice or physical stimulation |
- Note: 0 and-1 points need to be vigilant. The table is adapted from Aldecoa, et al., 2017.
| Score | Performance |
|---|---|
| 1 | The child makes eye contact with the caregiver |
| 2 | The child’s actions are purposeful |
| 3 | The child is aware of his/her surroundings |
| 4 | The child is restless |
| 5 | The child is inconsolable |
- Note: The first three items are reverse scoring, with the following rules: 4 points = no, 3 points = a little, 2 points = some, 1 point = very, 0 point = extremely. The last two positive scoring rules are as follows: 0 point = no, 1 point = a little, 2 points = some, 3 points = very, 4 points = extremely. The total PAED score was obtained by adding each score. The higher the score was, the heavier the degree of delirium was.
Prevention measures
The non-drug treatment of delirium is still the cornerstone of the prevention and treatment of delirium. The use of non-drug methods to prevent delirium has been proved to be effective, while the drug prevention and treatment of delirium still needs further research.
Non-drug treatment (Figure 2)
Acupuncture
Studies have found that the application of peripheral nerve stimulators electrical stimulation of bilateral Heart 7 (HT7) acupoint points can significantly reduce the emergence of agitation in children after general anesthesia (Hijikata, et al., 2016). However, the disadvantage of this method is that it requires the use of two neuromuscular transmission monitoring equipment, which presents certain difficulties in clinical practice. In order to facilitate clinical use, the researchers tested in a subsequent study using a single electrical stimulation of one side (right) HT7 acupoint during the operation. The results showed that unilateral electrical stimulation of HT7 had no effect on the incidence of agitation in children during the recovery period. The results of bilateral stimulation of HT7 are opposite (Nakamura, et al., 2018). This conclusion shows that in order to better recover patients, it is still necessary for researchers to develop more convenient instruments and equipment to better serve the majority of patients.
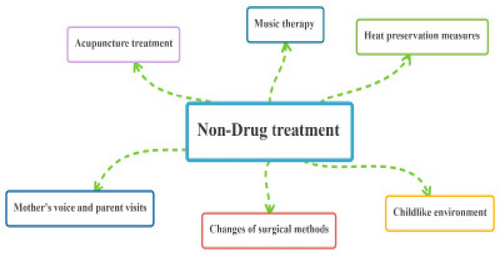
The flow chart of non-drug treatment
Mother's voice and parent visits
Familiar voices and the company of family members are the source of everyone's sense of intimacy and security. It has been reported in the literature that compared with the voice of strangers, the mother's voice reduces the delirium score and the incidence of delirium during the peri-extubation period, and promotes the recovery from general anesthesia (Song, et al., 2017, Byun, et al., 2018). In the PACU environment, parental visits after surgery can effectively improve the incidence of delirium during the peri-extubation period (In, et al., 2019). The results of this study will help the hospital to reformulate the PACU visit policy.
Music therapy
Music therapy is a new frontier discipline. As an intervention method to relieve pain and anxiety, it has been widely studied in perioperative period. A document published in 2019 described that after providing personalized music therapy for elderly patients undergoing elective surgery, the mood and pain of the patients improved, and the incidence of delirium was lower (Sharda, et al., 2019). The program provides a cheap, patient-centred treatment for perioperative teams, especially frontline nurses, to relieve postoperative pain and anxiety. We believe that it can be easily implemented in various hospital systems.
Heat preservation measures
Hypothermia can trigger a series of stress reactions in the body and delay the postoperative recovery and recovery time of patients. Perioperative heat preservation is conducive to maintaining the stability of vital signs of patients and effectively reducing the damage of postoperative cognitive function (Ma, et al., 2020). Perioperative hypothermia should be highly valued by anesthesiologists. Prevention and treatment of perioperative hypothermia is an important measure to improve the quality of perioperative anesthesia management and reduce postoperative complications.
The establishment of a childlike environment
The surgical cap worn by the medical staff in the operating room has changed from white to blue at first, and now it has evolved into different colors and patterns. Operating room wallpaper has become a child's favorite cartoon and game patterns, instead of the previous operating room only monochrome, to reduce the visual fatigue of surgical patients, alleviate their tension (Zhou, et al., 2011), is conducive to the smooth development of surgery and postoperative rehabilitation. Colorful surgical caps and wallpaper add a warm tone to the cold operating room environment to bring the distance between the doctor and the patient closer, so that the patient's mood is soothed and relaxed, reducing the patient's fear of surgery, reducing the occurrence of delirium, and improving the patient's prognosis.
Changes of surgical methods
In one study, Jeong DM et al found that the incidence of postoperative peri-extubation delirium in thoracoscopic esophagectomy was 0.55 times lower than that in traditional thoracotomy (Jeong, et al., 2016). Thus, that with the continuous development and popularization of minimally invasive surgery, the incidence of delirium in the peri-extubation period may further decrease in the near future.
Drug Treatment (Figure 3)
Dexmedetomidine
Dexmedetomidine has sedative, analgesic and anti-anxiety effects and is considered to be a promising drug for the treatment of delirium. Some scholars have found that dexmedetomidine is an effective drug for the treatment of delirium after non-cardiac surgery (Lee, et al., 2018, Choi, et al., 2016). For elderly patients, perioperative application of dexmedetomidine can reduce the incidence of peri-extubation delirium after cardiac surgery, delay the onset time and shorten the course of the disease (Shi, et al., 2019). Dexmedetomidine can also reduce peri-extubation delirium after sevoflurane anesthesia in preschool children, and 0.5 μg/kg/min can be safely used to prevent postoperative negative behavior (Shi, et al., 2019).
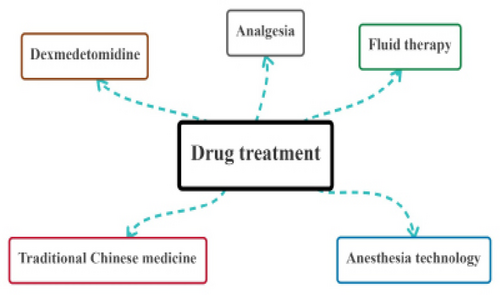
The flow chart of drug treatment
Analgesia
There is no clear answer to the “gold standard” for preventing delirium during peri-extubation. Pain was considered to be an important cause of delirium. Choi EK et al confirmed that maintaining a small dose of remifentanil (0.05μg/kg/min) for continuous pump infusion during the peri-extubation period after general anesthesia can reduce the incidence of peri-extubation delirium after surgery (Choi, et al., 2018). Compared with fentanyl, hydromorphone can prevent the occurrence of delirium in the peri-extubation period to the same extent, and can even significantly reduce the incidence of severe delirium, postoperative pain relief is more obvious, and the incidence of nausea and vertigo is lower (Chu, et al., 2018). However, it should be noted that the use of hydromorphone should pay attention to the occurrence of tongue retropulsion and excessive sedation.
Fluid therapy
The traditional idea is that restrictive transfusion can reduce surgical-related complications and shorten hospitalization time. However, fluid restriction can increase the risk of tissue hypoperfusion, reduce renal and others important organ perfusion, resulting in organ dysfunction (Shin, et al., 2018). At the same time, hypoperfusion is also a risk factor for peri-extubation delirium. Compared with restrictive infusion, target-directed infusion based on pulse mutation rate can maintain perioperative hemodynamic stability, improve cardiac index, increase cerebral perfusion, maintain stable cerebral oxygen supply and demand, and reduce the incidence of delirium (Wang, et al., 2021). Some researchers have found that the risk of delirium caused by perioperative use of hypotonic maintenance solution (sodium: 35 mmol/L) was higher than that caused by the use of isotonic maintenance solution (sodium: 140 mmol/L) (Nagae, et al., 2019). Therefore, it is believed that the use of isotonic maintenance fluid in the perioperative period will have broader prospects in the future.
Anesthesia technology
In recent years, ultrasound-guided nerve block technology has been widely popularized and developed rapidly. Preoperative ultrasound-guided continuous iliac fascia space block can improve perioperative sleep quality of elderly patients with hip fracture, reduce the incidence of postoperative delirium and shorten the duration of delirium (Xu, et al., 2020). Intraoperative ultrasound-guided lumbosacral plexus block combined with intraoperative mild sedation can also reduce the incidence of postoperative mental disorders and cognitive decline, and the postoperative analgesic effect is accurate (Mei, et al., 2017, Zeng, et al., 2016). The peri-extubation period after general anesthesia, especially during extubation, can easily cause severe hemodynamic fluctuations and increase the risk of delirium. Ultrasound-guided stellate ganglion block can effectively reduce the cardiovascular response during extubation (Pei, et al., 2021). The above research results indicate that ultrasound-guided nerve block has become a new option for peri-anesthesia analgesia and reduction of complications.
Traditional Chinese medicine
In recent years, Chinese scholars have found that the use of traditional Chinese medicine technology and methods can reduce the incidence of delirium and delay its development. Chinese herbal medicines such as ginseng (Sun, et al., 2019), berberine (Chen, et al., 2021) and gastrodin (Shi, 2021) may play a key role in the prevention, treatment or improvement of delirium.
Others
Other prevention and treatment measures that have been proved to be effective in reducing perioperative delirium include psychological intervention (Packiasabapathy, et al., 2019), oral probiotics (Wang, et al., 2021), infusion of magnesium sulfate (Xie, et al., 2016), maintenance of Hb > 11.1 g/dL (Kijima, et al., 2020), early preventive application of haloperidol (Fukata, et al., 2017), use of ulinastatin (Lin, et al., 2019).
Summary and outlook
The best treatment for peri-extubation delirium is prevention and early diagnosis, as well as active treatment of potential risk factors. Clarifying the risk factors of surgery and anesthesia will help improve the effectiveness of delirium treatment in patients during the peri-extubation period and improve the prognosis of patients. Although a large number of clinical studies have been done on delirium, the existing research results cannot completely prevent the occurrence of delirium in the peri-extubation period, and the incidence is still increasing year by year. This requires that anesthesiologists must abandon the traditional of the past, not just the “patron saint” in the operating room, but actively and effectively participate in each node of the patient's diagnosis and treatment process with a new concept of “perioperative medicine”. In order to accelerate the early completion of enhanced recovery surgery, all medical personnel and family members of patients involved in the diagnosis and treatment were combined to form a closely connected prevention chain from preoperative evaluation to postoperative follow-up. At the same time, in the future research, we can fully rely on the advantages of traditional Chinese medicine, in-depth study of traditional Chinese medicine and acupuncture in the treatment of delirium, formulate a set of more in line with China's national conditions of diagnosis and treatment plan, in order to reduce the incidence of peri-extubation delirium, accelerate the early rehabilitation of patients, shorten hospitalization time, improve the quality of life after operation.
Ethical statement
Not applicable.
Acknowledgments
Not applicable.
Conflict of interest
No conflicts of interest were declared.
Funding
This study was supported by Research Fund for the National Natural Science Foundation of China No. 81960214.
Transparency statement
The authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Authors' contribution
Rui Jiang contributed to conceiving the study and collect ingthe all the literatures, writing the paper, drawing; Yi Zhu assisted to finish this paper; Zhao-Qiong Zhu contributed to guidance and inspection.