Utilization of MRI in Fetal Surgery
Liqun Sun and Qiong Luo contributed equally to this work as co-corresponding authors.
Funding: This work was supported by Zhejiang Provincial Natural Science Foundation of China (Grant No. ZCLTGY24H0401) and Technology Program of Jiaxing (Grant No. 2024AD30125).
Wei Bian and Weizeng Zheng contributed equally to this work and share the first authorship.
ABSTRACT
Advances in fetal surgery techniques have enabled the treatment of certain congenital defects before birth. A critical area of focus is the role of perinatal imaging in optimizing prenatal interventions within the precision medicine framework. Magnetic resonance imaging (MRI) is emerging as an indispensable tool for guiding these intricate procedures with the potential to significantly enhance the standard of care and outcomes for affected fetuses. This review begins with an overview of the classification and indications for fetal surgical interventions. It then explores the detailed applications of prenatal MRI scanning and diagnostic techniques across various categories of fetal surgery. A key focus is how fetal MRI provides critical insights into specific lesion characteristics and tissue involvement, thereby aiding healthcare professionals in selecting the optimal surgical strategies for prenatal and postnatal interventions. Fetal MRI offers detailed visualizations that complement traditional ultrasound findings, enhancing the precision of radiological planning for fetal surgery. Finally, the review highlights how integration of fetal MRI into the decision-making process enables healthcare providers to make well-informed choices, ultimately improving the prognosis and outcomes for both the mother and fetus.
Abbreviations
-
- 2D
-
- 2-dimensional
-
- 3D
-
- three-dimensional
-
- CCAM
-
- congenital cystic adenomatoid malformation
-
- CHAOS
-
- congenital high airway obstruction sequence
-
- CDH
-
- congenital diaphragmatic hernia
-
- EXIT
-
- ex utero intrapartum treatment
-
- FETO
-
- fetal endoscopic tracheal occlusion
-
- MRI
-
- magnetic resonance imaging
-
- OFS
-
- open fetal surgery
-
- SSFSE
-
- single shot fast spin echo
-
- SSR
-
- super-resolution tracheal reconstruction
-
- TRAP
-
- twin-reversed arterial perfusion
-
- TTTS
-
- twin-twin transfusion syndrome
1 Introduction
Fetal or maternal–fetal surgery refers to specific procedures conducted to correct prenatally detected congenital abnormalities. These interventions address conditions that present substantial risks to fetal viability and development, where postponing treatment until the postnatal period may significantly increase the likelihood of fetal mortality or severe postnatal morbidity [1].
As a pioneering discipline in modern medicine, this field focuses on performing intricate surgical procedures in utero to optimize long-term pediatric outcomes [2, 3]. A particularly significant development is the synergistic integration of magnetic resonance imaging (MRI) with conventional ultrasound which revolutionized the diagnosis and clinical management of congenital anomalies [4]. Although ultrasound remains the primary imaging tool for fetal evaluation, MRI provides superior tissue contrast, multiplanar imaging, and detailed anatomical visualization, facilitating more precise surgical planning. Fetal MRI improved the identification of complex anomalies, enabling clinicians to assess disease severity, evaluate treatment options, and optimize intervention timing. By complementing ultrasound, MRI enhances decision-making in fetal surgery by aiding assessments of the feasibility and necessity for in utero interventions versus postnatal management [5]. MRI is also crucial in guiding labor planning and neonatal resuscitation strategies, further improving perinatal outcomes [6].
Despite the advances in this field, the decision to perform fetal surgery requires a complex risk-benefit analysis that weighs the potential fetal benefits against the maternal risks. A multidisciplinary approach incorporating advanced imaging modalities like MRI enables personalized intervention strategies. Continued refinement of these integrated imaging techniques is driving progress in fetal surgery and improving outcomes for both mother and fetus.
2 Literature Search Method
A comprehensive literature search was conducted across multiple databases, including PubMed, Web of Science, Embase, and Cochrane. The search utilized the following keywords and their associated free terms (“fetus”) AND (“magnetic resonance imaging”) AND (“ex-utero intrapartum treatment procedures” OR “fetoscopies” OR “endoscopic” OR “minimal surgical procedure” OR “fetal therapies”). After completion of the searches, duplicate records were removed, and the following types of publications were excluded: systematic reviews, meta-analyses, animal studies, conference proceedings, guidelines, patents, any articles not relevant to the specified disease criteria, and case reports. Ultimately, a total of 198 articles were selected for analysis and review (Figure 1).
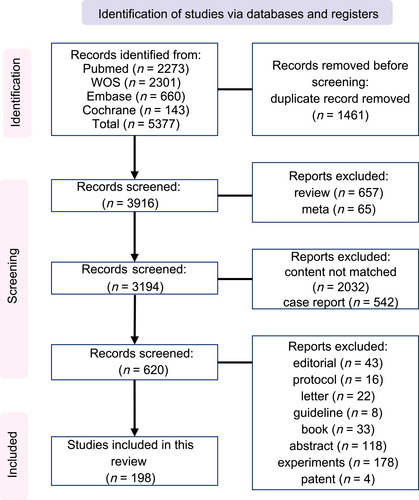
Flowchart of the literature search process.
3 Classification and Indications for Fetal Interventions
Over the past several decades, the landscape of medical interventions for certain conditions evolved dramatically, marked by the establishment of highly specialized healthcare centers boasting unparalleled expertise in fetal surgery. These cutting-edge facilities pioneered a range of sophisticated procedures, including ex utero intrapartum treatment (EXIT) procedures, open fetal surgery (OFS), fetoscopic surgery, and percutaneous interventions [1]. The timeline and specific indications for these groundbreaking surgical approaches are meticulously detailed in Figure 2, serving as a comprehensive guide for practitioners navigating this complex field.
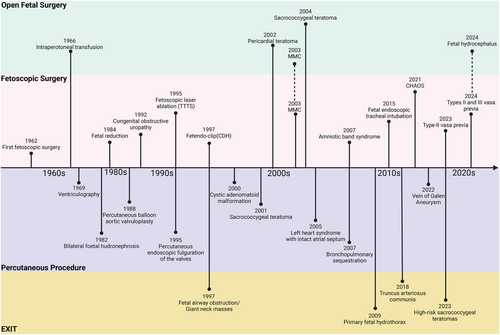
By integrating functional and anatomical data, fetal MRI plays a pivotal role in determining the optimal timing for interventions, ensuring that surgery occurs at the gestational stage that most likely preserves fetal organ function while minimizing maternal risk. The EXIT procedures are performed during cesarean delivery, with the fetus partially delivered but still connected to the placenta, to secure the fetal airway or address other life-threatening conditions. OFS involves accessing the fetus in utero through incisions in the maternal abdomen and uterus and is typically reserved for severe congenital anomalies requiring immediate intervention, whereas fetoscopic surgery employs minimally invasive methods, utilizing small incisions to insert a camera and specialized instruments, and is suitable for a range of fetal conditions. Meanwhile, percutaneous interventions rely on needle-based techniques to access the fetus via the maternal abdomen and are commonly applied in procedures like fetal shunt placement, laser ablation, and other highly targeted treatments.
3.1 Ex utero Intrapartum Treatment
The EXIT concept was proposed in 1982 and successfully implemented in fetal surgery in 1997 [7, 8, 38]. An EXIT procedure is a specialized delivery strategy used to manage fetal airway compromise or other life-threatening congenital anomalies. Unlike standard cesarean delivery, an EXIT procedure involves partial delivery of the fetus, with preservation of the placental circulation and stabilization of the airway (e.g., intubation, tracheostomy, or tumor resection). This technique helps ensure the safety of the neonate before full delivery [39]. These procedures have proven particularly beneficial in cases with fetal airway obstruction such as giant cervical teratomas, enabling safe control and management of the airway and improved outcomes [40, 41]. Nowadays, EXIT procedures are widely used when the prenatal diagnosis indicates potential problems with neonatal airway compromise or cardiopulmonary instability [39]. These procedures can maintain the uteroplacental circulation during cesarean section, avoiding crises and allowing a stable transition from placental to neonatal circulation [42].
3.2 Open Fetal Surgery
OFS is a sophisticated and highly advanced procedure that involves a direct surgical intervention on the fetus while still in the womb. Over the years, OFS has undergone significant advances, establishing itself as a viable approach for managing severe fetal diseases and congenital anomalies. The procedure requires a hysterotomy—an incision through the maternal abdominal wall and uterus—to gain direct access to the fetus [43, 44]. This approach provides optimal visualization and ample space for precise surgical repair. Initially, OFS was primarily targeted at conditions such as spina bifida, producing significantly superior outcomes compared with postnatal surgery [45, 46]. However, it has since been extended to other conditions including pulmonary hypoplasia, congenital heart defects, and tumors [47, 48]. OFS is typically performed during the later stages of pregnancy to optimize fetal growth and development. This type of intervention was shown to improve survival rates and long-term quality of life for affected fetuses. Historically, OFS was reserved for life-threatening conditions or severe fetal anomalies. However, emerging evidence from preclinical studies has suggested that it may confer neurodevelopmental benefits, potentially enhancing fetal brain development. Consequently, the medical community is increasingly exploring the application of this procedure to repair spinal meningeal malformations and other congenital defects with the potential to significantly improve the fetal prognosis [49, 50].
3.3 Fetoscopic Surgery
Fetoscopic surgery is a transformative, minimally invasive alternative to conventional open maternal–fetal surgery. By eliminating the need for large incisions, this technique markedly reduces maternal complications and minimizes the risk of preterm birth, making it a highly favorable option for both maternal and fetal outcomes. Fetoscopic techniques have become standard practice in the treatment of conditions such as twin–twin transfusion syndrome (TTTS) and congenital diaphragmatic hernia [51, 52]. For TTTS, fetoscopic laser surgery using the Solomon technique is particularly effective. This method corrects vascular connections between the twins, balancing blood flow and improving perinatal outcomes [53-55]. Fetoscopy is also utilized to treat amniotic band syndrome by releasing constrictive bands and to remove herniated intestines in cases of diaphragmatic hernia [56, 57]. Compared with OFS, fetoscopic repair of myelomeningocele lesions carries a lower risk of complications such as uterine rupture and preterm birth [58].
The versatility of fetoscopic surgery continues to expand, enabling interventions such as tracheal decompression and tracheotomy in cases of vocal cord fusion and laryngeal atresia [59]. More recently, fetoscopic laser photocoagulation is utilized in the management of vasa previa, effectively mitigating the risk of rupture and facilitating successful vaginal delivery [36]. Overall, the minimally invasive nature of fetoscopic surgery offers significant benefits over traditional open procedures for both the mother and fetus.
3.4 Percutaneous Procedures
Advances in imaging and surgical technology significantly propelled the growth of percutaneous fetal interventions, addressing a wide range of congenital anomalies. These minimally invasive procedures are now considered standard practice at specialized centers [48, 60]. Ultrasound-guided techniques, such as the placement of vesico-amniotic shunts for lower urinary tract obstruction, were performed since the 1980s [48, 61]. Similarly, thoracic shunts play a critical role in the management of conditions such as congenital diaphragmatic hernia and fetal hydrothorax by facilitating the drainage of excess fluid, thereby alleviating pressure on the developing lungs [48, 62].
Radiofrequency ablation emerged as an effective technique for the treatment of vascular lesions and tumors, thus reducing the risk of fetal hydrops and other complications [63, 64]. Intracardiac catheter procedures are also gaining traction for correcting or alleviating congenital heart defects, including the use of fetal aortic valvuloplasty, to prevent the progression of aortic valve stenosis to hypoplastic left heart syndrome [65].
Innovations such as transuterine ultrasound-guided fetal embolization of vein of Galen malformations highlight the remarkable progress in the field of fetal interventions. This procedure enables elimination of the postnatal pathophysiology, offering significant benefits [66]. The minimally invasive nature of these percutaneous procedures allows targeted treatment while minimizing the risks to both the mother and fetus.
EXIT procedures involve partial delivery of the fetus while maintaining placental support for critical interventions, such as airway management, whereas OFS requires direct access to the fetus via a larger abdominal incision to correct major congenital defects. In contrast, fetoscopic surgery is minimally invasive, utilizing small instruments for targeted procedures such as laser treatment, and percutaneous procedures employ needle access for interventions such as cyst drainage.
4 Role of Fetal MRI in Fetal Surgery
Recent advances in prenatal diagnostics, particularly fetal MRI, have become instrumental for the evaluation of various fetal abnormalities, including tumors, structural airway anomalies, and other conditions with poor prognostic outcomes. To minimize motion artifacts and optimize image quality, fetal MRI routinely employs rapid acquisition sequences, thereby improving diagnostic reliability [67, 68]. The typical imaging planes include axial, sagittal, and coronal views of the fetus. These techniques facilitate precise preoperative planning and an enhanced understanding of fetal anatomy which is crucial for successful surgical outcomes.
4.1 EXIT
Fetal MRI has been a critical diagnostic tool for the evaluation of complex fetal conditions, particularly those involving airway obstruction, since 1983 [69, 70]. This advanced imaging technique provides essential diagnostic and anatomical information about large fetal neck masses and the surrounding airways which is crucial for planning EXIT procedures. By utilizing multiple MRI pulse sequences, the full extent of a mass can be delineated, offering significant advantages over ultrasound. These sequences enable detailed characterization of the nature of the mass and assessment of airway compression. Specifically, a single-shot fast spin-echo (SSFSE) sequence minimizes motion artifacts from fetal movement, enabling clear visualization of high T2 signals in liquid-filled fetal airways, including the oropharynx and larynx. If the airway is encased or displaced by a neck mass, fetal MRI can precisely localize the tracheal position and contour, aiding airway management planning and identifying the optimal site for tracheostomy during the EXIT procedure (Figure 3) [69, 71, 72].
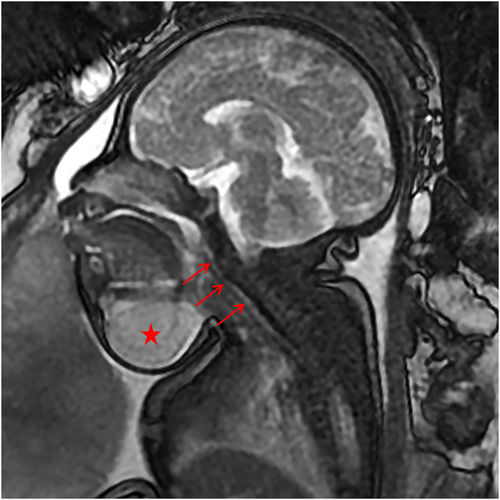
Fetal MRI showing compression of the airway (arrows) by a cervical mass (star), facilitating early surgical planning.
Advanced MRI techniques, such as super-resolution tracheal reconstruction (SSR), MRI-based 3D modeling, 3D navigation, and virtual bronchoscopy, were applied to evaluate fetal neck masses and adjacent airways [72-74]. SSR, combined with conventional 2D MRI, offers higher image clarity and further delineation of anatomical details. The 3D technologies enhance prenatal airway assessment, patient counseling, and perinatal management. Moreover, because of the strong associations between fetal head and neck lesions and central nervous system abnormalities, fetal MRI facilitates detailed brain structure assessments that detect coexisting pathological changes [75-77].
Fetal MRI has proven effective in the visualization of chest tumors and their surrounding structures, offering a more accurate basis for prenatal counseling and surgical planning [78, 79]. In cases with congenital high airway obstruction syndrome (CHAOS), fetal MRI can confirm ultrasound findings and localize the obstruction site, guiding decision-making for fetal or neonatal interventions via an EXIT procedure [80, 81]. The MRI findings in CHAOS include dilated airways, increased lung signals, flattened hemidiaphragms, ascites, heart compression, and placentomegaly. Prenatal MRI is useful for determining the likelihood of a successful EXIT procedure, because low tracheal obstruction is associated with failed airway access. In CHAOS cases, 2D MRI and sequence-registered reconstruction techniques can clarify the obstruction levels, such as laryngeal communications, that are missed by ultrasound. This information is critical for surgical planning and optimization of an EXIT procedure [74, 82]. 3D virtual bronchoscopy further aids in CHAOS diagnosis and management [83].
When combined with fast T1-and T2-weighted imaging, MRI can qualitatively and quantitatively analyze the thoracic contents as well as the lung and liver volumes in CDH (congenital diaphragmatic hernia) patients, thereby predicting the clinical outcomes [84-86]. Metrics like the fetal pleural effusion-to-lung tissue volume ratio and mediastinal displacement can guide EXIT procedures [87, 88]. Recent advances in 3D printing and pre-procedure simulations using 3D modeling have enhanced team collaboration and improved EXIT procedure management [89].
Overall, MRI provides invaluable information for EXIT procedures, enabling accurate fetal anatomy assessment and tailored surgical planning for complex airway or congenital abnormalities. Its detailed imaging capabilities are essential for visualizing fetal structures and identifying optimal interventions, ensuring safe delivery and effective postnatal management.
4.2 Open Fetal Surgery
In cases with open neural tube defects, fetal MRI can not only depict the extent of the spinal dysraphism and the protruding spinal cord/meninges to guide the open surgical repair but also characterize the composition of the herniated tissues. Importantly, sagittal T2-weighted imaging can demonstrate the presence and degree of cerebellar tonsillar herniation as well as any associated hydrocephalus. Conversely, closed dysraphism exhibits a more continuous sac wall transition, fewer posterior fossa anomalies, and a higher association with the omphalocele-exstrophy complex than open defects [90]. This information is valuable for prenatal neurosurgical consultations, assessing the potential benefits of interventions, and guiding the decision-making regarding surgery [91-93]. MRI enhances the diagnostic accuracy of fetal neuroimaging and improves the management in a high proportion of neural tube defect cases [94, 95].
Fetal MRI can delineate the location of sacrococcygeal teratoma and characterize the tumor type by revealing whether the mass is cystic or solid. It can also evaluate any associated findings such as the mass effect on the displaced vagina and bladder, bilateral hydroureteronephrosis, vaginal distension, ascites, pulmonary compression, and oligohydramnios [17]. The high T1 signals in the meconium can help to differentiate a type IV cystic teratoma from a cloacal malformation. Multiplanar imaging can clarify the relationship between the mass and the spinal canal, aiding in distinguishing sacrococcygeal teratoma from a myelomeningocele [41, 96].
For fetal open brain procedures, such as ventriculo-amniotic shunt placement, fetal MRI can assess the degree of ventriculomegaly, the integrity of the septum pellucidum and ependymal lining, and the development of the cerebral cortex. Postoperative fetal MRI can not only evaluate the shunt position but also monitor the recovery of the underlying brain pathology such as the improvement in ventriculomegaly and progressive cortical thickening [18].
Because fetal MRI provides a detailed visualization of the fetal anatomy, it plays a crucial role in OFS planning and guidance. The integration of high-resolution MRI data enhances the precision and safety of these surgical procedures, enabling clinicians to make more informed decisions and optimize the surgical approaches.
4.3 Fetoscopic Surgery
Fetal MRI has multiple critical roles for TTTS. It can precisely depict the growth disparities between the fetuses (Figure 4), identify any pathological placental changes, such as increased thickness and heterogeneous signal characteristics, and enhance preoperative planning [97, 98]. Advanced deep learning techniques can simulate fetoscopic views and laser ablation, optimizing surgical strategies and training [99]. The deep Q-CapsNet reinforcement learning framework further refines preoperative planning by generating accurate placental and cavity models [100]. Postoperatively, fetal MRI can assess the placental infarction extent and detect central nervous system complications via diffusion-weighted imaging [101, 102].
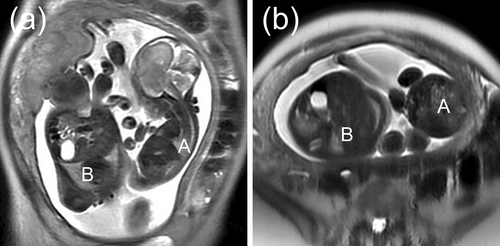
MRI showing TTTS causing growth discrepancy between the twins, with Fetus A (donor) significantly smaller than Fetus B (recipient). (a) Maternal uterus, SSFSE sequence, coronal plane, (b) Maternal uterus, SSFSE sequence, axial plane. MRI, magnetic resonance imaging; SSFSE, single shot fast spin echo; TTTS, twin-twin transfusion syndrome.
For CHAOS cases, in situ fetoscopic laser ablation of the obstructing lesion emerged as an alternative to an EXIT procedure, altering the natural history and improving the long-term survival. Fetal MRI can not only highlight the advantages of the EXIT procedure but also delineate the length of the obstructing segment, providing critical guidance to determine the fetoscopic access and ablation distance [103].
Fetal MRI significantly enhances the evaluation of urogenital abnormalities by providing detailed structural and functional insights beyond those achievable with ultrasound alone. Studies indicated that MRI improves the diagnostic accuracy, enabling better presurgical planning and management of conditions such as lower urinary tract obstruction [104]. Utilizing SSFSE techniques, fetal MRI can comprehensively assess the urinary tract, especially in cases with late-gestation anomalies identified on ultrasound [105]. It effectively visualizes findings related to the posterior urethral valves including bilateral hydronephrosis, hydroureteronephrosis, increased bladder volume, and proximal urethra dilatation. 3D virtual cystoscopy offers non-invasive, accurate imaging to guide fetoscopic interventions [106]. Fetal MRI can also evaluate the relationships between the three bladder angles, namely the bladder neck angle, vesico-urethral angle, and detrusor-bladder neck angle, allowing assessment of the anatomical constraints and physiological curvature of the enlarged fetal bladder, indicating the feasibility of fetoscopic procedures [107].
Since 1988, MRI was utilized to detect vasa previa with sagittal T1-weighted imaging offering clearer visualization of the placental location relative to the cervical os compared with prenatal ultrasound [108]. The half-Fourier single-shot turbo spin-echo T2-weighted sagittal sequence provides further enhancement by revealing the relationship of the flow voids representing the previa vessels to the fetus, placenta, and cervical os. This detailed imaging guides the fetoscopic laser ablation approach [109, 110]. The timing of surgery for amniotic band syndrome is crucial and significantly influenced by MRI findings. Amniotic bands are characterized by their linear structures with low T2 signals, distinguishing them from movement artifacts in the amniotic fluid (Figure 5). MRI provides a clear visualization of the limb involvement in amniotic band syndrome and allows assessment of the potential effects on other organs including the head, neck, and abdomen [111, 112]. This comprehensive evaluation aids in determining the feasibility of surgery and informs the optimal timing for intervention.
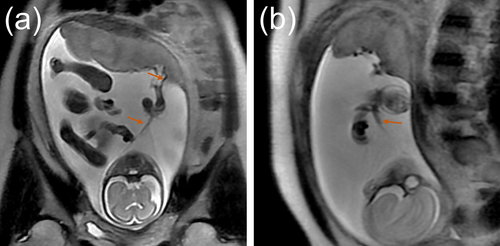
Fetal MRI with T2-weighted imaging showing hypointensity of the amniotic band (arrows) against the amniotic fluid background. (a) Maternal SSFSE sequence, coronal plane, (b) Maternal SSFSE sequence, sagittal plane. MRI, magnetic resonance imaging; SSFSE, single shot fast spin echo.
4.4 Percutaneous Procedures
MRI assumes a preeminent role in contemporary prenatal surgical planning, particularly in the management of thoracic shunts, urinary decompression procedures, radiofrequency ablations, and intracardiac catheter interventions. By providing high-resolution multiplanar imaging capabilities, MRI significantly enhances diagnostic accuracy and operative precision, thereby contributing to improved maternal-fetal outcomes.
Fetal MRI serves as an indispensable diagnostic modality for the evaluation of congenital pulmonary airway malformations (CPAMs) [113, 114]. It enables precise characterization of the lesion topography, cystic architecture, and histological subtype according to the modified Stocker classification (types 0–4). MRI also allows a detailed assessment of the parenchymal involvement, mediastinal displacement, and hydrops fetalis while differentiating CPAMs from pulmonary sequestration and congenital diaphragmatic hernias. Although not directly utilized for in utero therapeutic interventions, MRI-derived anatomical insights are critical for guiding clinical decision-making including prenatal corticosteroid administration for microcystic CPAMs (Type 3) and cyst aspiration for macrocystic variants (Type 1) (Figure 6). Serial post-treatment imaging facilitates monitoring of lesion progression, informing decisions regarding an EXIT procedure, OFS, or postnatal resection [115].
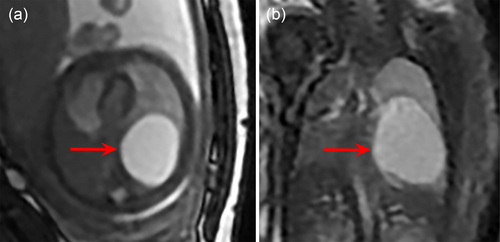
Fetal MRI of a congenital pulmonary airway malformation case revealing the characteristics of a single large cyst in the left lung (arrows), facilitating percutaneous drainage for surgical intervention. (a) Fetal chest, 3D FIESTA sequence, axial plane, (b) Fetal chest, 3D FIESTA sequence, coronal plane. FIESTA, fast imaging employing steady-state acquisition; MRI, magnetic resonance imaging.
In the evaluation of vein of Galen malformations, T2-weighted MRI sequences offer distinct advantages by visualizing flow voids that represent anomalous vasculatures. This enables accurate localization of arteriovenous shunts, quantification of hemodynamic parameters, and assessment of cerebral parenchymal involvement. These imaging characteristics are instrumental for preoperative embolization planning and post-interventional follow-up, ensuring timely management of these life-threatening cerebrovascular anomalies [66, 116, 117].
Regarding fetal cardiac interventions, MRI provides unparalleled anatomical and functional assessments that are essential for percutaneous procedures such as balloon valvuloplasty and atrial septostomy [74, 118]. Since its introduction in the 1990s, cardiac MRI has complemented echocardiography for the diagnosis of aortic stenosis by visualizing post-stenotic dilation and quantifying the flow dynamics in the aortic isthmus and descending aorta [119]. This capability aids in identifying fetuses with critical left ventricular outflow tract obstruction, characterized by retrograde aortic flow and reduced cardiac output [120]. Postoperatively, MRI serves as the gold standard for evaluating structural remodeling and functional recovery [121].
In the field of radiofrequency ablation, MRI is increasingly recognized for its role in the management of fetal tumors and other lesions. It facilitates precise localization and characterization of tumors which are essential for planning ablation procedures. By providing detailed information on the relationships between the tumor and its surrounding structures, MRI facilitates safer and more effective interventions [121]. Fetal MRI plays a crucial role in enhancing preoperative planning across these surgical approaches. For EXIT procedures, MRI provides vital anatomical details about the fetal airway, whereas in OFS, it aids in assessing complex structural defects. In fetoscopic surgery, MRI helps to identify placental and vascular anomalies, and for percutaneous procedures, it maps anatomical structures to ensure accurate needle placement and intervention, ultimately improving surgical outcomes.
5 Fetal MRI Complements Ultrasound in Fetal Surgery
For fetuses with a high risk of malformations identified during prenatal ultrasound screening, fetal surgery can serve as a successful management approach [58, 121]. All pregnant women receive routine ultrasound examinations at 11–14 weeks and 22–26 weeks of gestation. Early pregnancy nuchal translucency on a scan may indicate neck lesions or the risk of an abnormality [122]. Prenatal ultrasound can detect tumors and congenital lesions in a timely and effective manner, initially indicating the size, location, cystic solidity, blood supply, and other characteristics of the lesion. Ultrasound can evaluate the presence of esophageal and airway obstruction in the fetus through indirect images (mast volume, swallowing, and tongue frequency). Doppler imaging can assess the fetal cardiovascular status (heart, umbilical artery, middle cerebral artery, and venous catheter) [123]. However, on ultrasound, it is difficult to assess the degree of tumor compression, which is susceptible to the physical condition of the pregnant woman and the location of the fetal lesion, and challenging to visualize directly in the throat and trachea for fetus. Obstetric ultrasound shows less effective anatomical details, complicating treatment planning for surgeons [89].
MRI offers high-resolution imaging capabilities, enabling precise characterization of pathological lesions and their spatial relationships with anatomical structures. Its unique capacity to generate multiplanar, multiangular, and multisequence datasets confers distinct advantages for the evaluation of complex fetal cardiac morphologies and pulmonary developmental trajectories. Unlike ultrasound, which may be limited by the maternal body habitus or oligohydramnios, MRI provides artifact-free visualization of the fetal spine which is particularly critical for the detection of occult neural tube defects. In CDH, MRI surpasses ultrasonography in quantifying the herniated abdominal viscera and calculating the fetal lung volumes, thereby improving the prognostic accuracy and predicting the likelihood of requiring extracorporeal membrane oxygenation postnatally [124, 125].
6 Limitations and Future Directions of Fetal MRI
Although fetal MRI is valuable for prenatal diagnostics and surgical planning, it faces significant limitations that restrict its universal application. Key challenges include the lack of real-time intraoperative monitoring [126], motion artifacts that degrade the image quality [127], and gestational age constraints [107], specifically poor resolution in the first trimester and obscured anatomical details in the third trimester due to fetal crowding. Diagnostic accuracy varies by anomaly type with safety concerns like acoustic noise and electromagnetic fields posing additional risks. Maternal factors such as obesity and claustrophobia exclude 15%–20% of cases from undergoing fetal MRI, whereas high costs and specialized expertise limit accessibility, particularly in low-income regions [128]. Addressing motion artifacts, improving resolution, and enhancing global access are crucial for maximizing the potential of fetal MRI in prenatal care.
7 Conclusions
Fetal MRI has significantly advanced the field of fetal surgery by providing superior imaging capabilities that complement traditional ultrasound. MRI leverages high-resolution anatomic visualization, enhanced tissue contrast resolution, and multiplanar imaging capabilities to optimize preoperative planning, refine intervention timing, and ultimately improve neonatal outcomes. Future research should focus on refining MRI protocols, integrating artificial intelligence for advanced image analysis, and evaluating the long-term effects of MRI-guided interventions.
Author Contributions
Wei Bian: writing – original draft (lead). Weizeng Zheng: writing – original draft (lead). Zesi Liu: writing – review and editing (supporting). Qiong Luo: writing – review and editing (lead). Liqun Sun: writing – review and editing (lead).
Acknowledgments
The authors have nothing to report.
Ethics Statement
The authors have nothing to report.
Consent
All imaging data used in this article were obtained with written informed consent from the patients or their legal guardians.
Conflicts of Interest
This article belongs to a special issue (SI)—Fetal Imaging, Maternal and Children Imaging. As the SI's Guest Editor, Professor Liqun Sun is excluded from all the editorial decision related to the publication of this article. The other authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed.