Efficacy of prostatectomy using a Retzius-sparing approach as an additional excision in anal canal carcinoma after brachytherapy for prostate adenocarcinoma
Abstract
Introduction
Standard treatments for squamous cell carcinoma of the anal canal include chemoradiotherapy and surgical resection. We report a rare case of squamous cell carcinoma of the anal canal with prostate invasion treated with curative surgical methods using a Retzius-sparing robot-assisted approach.
Case presentation
A 76-year-old male had undergone brachytherapy for prostate adenocarcinoma (cT2aN0M0). Nine years later, the patient was diagnosed with anal canal carcinoma (cT2N0M0) following the onset of anal pain. During a robot-assisted abdominoperineal resection, prostate invasion was suspected and a prostatectomy was performed as an additional excision of the prostate using a Retzius-sparing approach. Although an anastomotic leak was observed postoperatively, it was conservatively managed with bilateral ureteral stent placement. The patient remained recurrence-free after surgery.
Conclusion
A Retzius-sparing robot-assisted approach in radical prostatectomy may be a safe and feasible option for cases of anal canal carcinoma with suspected prostate invasion.
Abbreviations & Acronyms
-
- CRT
-
- chemoradiotherapy
-
- CT
-
- computed tomography
-
- Hb
-
- hemoglobin
-
- MRI
-
- magnetic resonance imaging
-
- Pn1b
-
- perineural invasion
-
- pRM1
-
- positive resection margin
-
- RS-RARP
-
- Retzius-sparing robot-assisted radical prostatectomy
-
- RT
-
- radiotherapy
-
- SCC
-
- squamous cell carcinoma
-
- SJ
-
- single J-type stent
-
- V1c
-
- vascular invasion
Keynote message
This case report highlights the successful application of a Retzius-sparing robot-assisted approach in radical prostatectomy for anal canal squamous cell carcinoma with suspected prostate invasion.
Introduction
Anal cancer occurs relatively rarely as a malignancy, making up approximately 1% of colorectal cancers.1 The treatment of SCC of the anal canal varies according to the stage of the tumor, with CRT and surgical treatment being considered for locally advanced cases.2, 3 Robotic surgery has become widespread in recent years, and an established optimal treatment strategy for anal canal carcinoma. Here, we report a patient with anal canal carcinoma who required additional excision of the prostate in radical surgery. We successfully performed a RS-RARP even after brachytherapy for prostate adenocarcinoma.
Case presentation
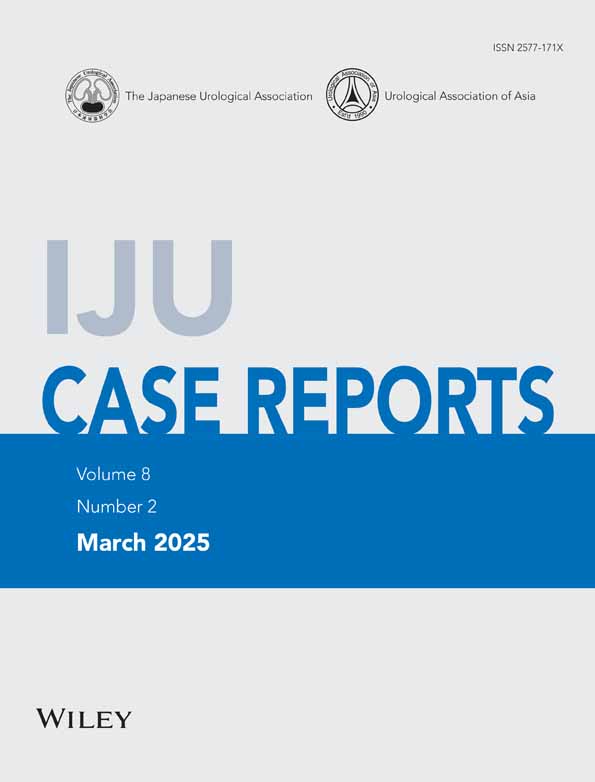
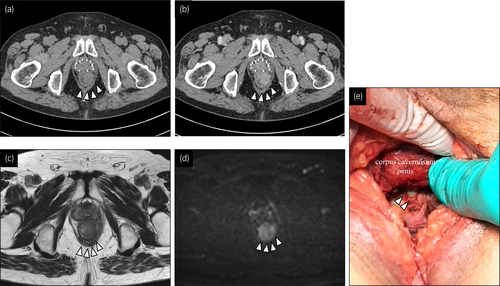
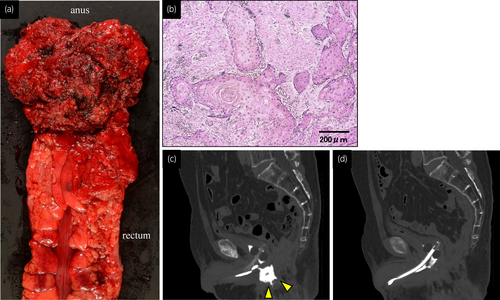
The patient was a 76-year-old man who visited the hospital complaining of anal pain. A hard mass, 3 cm from the anal verge, with poor mobility was found in a rectal examination. Colonoscopy demonstrated a type 3 elevated lesion from the lower rectum to the anal canal. Pathological results of the biopsy revealed an SCC. CT (Fig. 1a,b) and pelvic MRI (Fig. 1c,d) did not reveal any obvious metastasis or invasion of the prostate or urinary tract. The patient was diagnosed with anal canal SCC, cT2N0M0. CRT was considered a treatment for the anal canal SCC; however, considering a past history of brachytherapy that had been performed for a prostate adenocarcinoma 9 years ago, it was decided that this patient would be treated with surgery. A robot-assisted abdominoperineal resection was performed by an experienced gastroenterological surgeon. During the radical surgery, when performing an anal excision after the removal of the rectum and bowel using a transperitoneal approach, a urethral catheter was directly observed (Fig. 1e) and, based on operative findings, prostatic invasion was strongly suspected. After the creation of a colostomy, a combined additional prostatectomy was performed by an experienced urologist using an RS-RARP approach (Fig. 2a,b). Histopathological findings showed moderately differentiated SCC with keratinization originating from the anal canal. A diagnosis of pT3N0 was made, indicating no regional lymph node metastasis. However, V1c, Pn1b, and a pRM1 were observed. The prostate specimen showed no remnants of adenocarcinoma (Fig. 2c) or infiltration of SCC from the anal canal (Fig. 3a), and degeneration was noted that mainly consisted of fibrous components (Fig. 3b). One week after surgery, CT demonstrated a ruptured suture of the vesicourethral anastomosis (Fig. 3c). Conservative treatment involved the placement of bilateral ureteral stents and a urethral catheter, and anastomotic leakage resolved completely 6 weeks after surgery (Fig. 3d). Although urinary incontinence continued for 6 months after the patient's discharge from hospital, no recurrence of cancer was evident and the patient did not require a urinary catheter.

Discussion
Because the 5-year survival rate for CRT ranges from 40% to 70% in patients with SCC from the anal canal, and in cases of residual disease or local recurrence after CRT, surgical resection remains a viable salvage treatment option.2 In this case, due to the previous history of brachytherapy, and considering the rectal tolerance dose of radiation (60 Gy), radical surgery was performed.3 To date, several reports exist regarding cases requiring excision of the prostate in advanced rectum cancer after radiation; en-bloc resection of the rectum and prostate was performed in almost all cases. No report exists of the additional excision of the prostate due to a suspicion of its involvement from anal canal carcinoma after the removal of the rectum and anal canal.
In general, salvage surgery after radiotherapy for prostate adenocarcinoma is associated with a higher risk of bleeding and rectal injury compared to primary prostatectomy due to adhesions between the prostate and adjacent structures. With regard to the additional excision of the prostate after radiation, the structures and blood vessels around the prostate and pelvis are prone to be destroyed. In a conventional RARP, by removal of the bladder and prostate via dissection of the Retzius space, a clear operative field is attained. However, this procedure can damage various nerves and structures of the bladder associated with tissue repair, including feeding vessels and the pelvic fascia. In comparison, in an RS-RARP approach, the pelvic floor muscle can also be maximally preserved; this minimizes surgical trauma and preserves normal anatomical structures. In addition, in this case, to remove the rectum and anal canal, the entire posterior surface of the prostate had been removed; therefore, we selected an RS-RARP for an additional excision. Several case reports described he efficacy in urinary continence in abdominoperineal resection with en-bloc prostatectomy with vesicourethral anastomosis in patients with advanced rectum cancer,4, 5 however, no report exists describing the recovery of urinary continence after radical surgery with prostatectomy in case of anal canal patient. However, undoubtedly, wide excision of rectum and anus including pelvic floor muscles, can result in severe injury to important structures and nerves of the bladder associated with urine continence. By accumulating the data of future cases, the feasibility of the RS approach should be conducted.
A ruptured suture of the vesicourethral anastomosis occurred; however, this was controlled by conservative treatment. Long-term observations, including voiding function, are required in the future. With appropriate case selection, an RS-RARP approach is safe and better surgical outcomes would be expected. This approach may also have potential applications in the pelvic exenteration of malignancies originating from the intestinal tract, particularly in cases where bladder preservation is feasible. In robotic prostatectomy, the incidence of vesicourethral anastomotic leak remains high at approximately 20%.6 Anastomotic leakage occurs in 0.3% to 15.4% of cases after radical prostatectomy but more frequently in 33% to 50% of cases after radical prostatectomy following rectal resection.7 Several reports described how risk factors included inversion of the bladder mucosa during anastomosis, ischemic heart disease, radiation therapy, and loss of supporting tissue around the anastomosis.8 In this case, the risk of anastomotic leakage was extremely high due to the loss of supporting tissue behind the urethra caused by the rectal resection, and a blood flow disorder caused by radiation therapy and the wide resection of the rectum and anal. Conservative treatment of an anastomotic leakage involves extending the placement period of the urethral catheter; however, difficult cases that do not improve occur in 0.9% to 2.5% of cases.9 The placement of a bilateral single 6-Fr J-type stent (SJ), vesicostomy, and nephrostomy could be effective in such cases. Elmor et al. described an endoscopic approach that involved placing a 6-Fr bilateral SJ to reduce persistent vesicourethral anastomotic leak and promote closure.10, 11 Taking into consideration our case, even after radiation therapy, bilateral ureteral stent placement may be a promising first choice of treatment.
Conclusion
This report is the first to describe an RS-RARP approach applied to the SCC of the anal canal with suspected prostate invasion. This procedure might be a safe and feasible option for prostatectomy as an additional excision.
Acknowledgments
None.
Author contributions
Takahiro Yanase: Conceptualization; data curation; writing – original draft. Taku Naiki: Supervision; writing – review and editing. Aya Naiki-Ito: Writing – review and editing. Ryosei Okawa: Writing – review and editing. Sosuke Niwa: Writing – review and editing. Nobuhiko Shimizu: Writing – review and editing. Shuzo Hamamoto: Writing – review and editing. Yoshiaki Fujii: Writing – review and editing. Hiroki Takahashi: Writing – review and editing. Takahiro Yasui: Supervision; writing – review and editing.
Conflict of interest
The authors declare no conflicts of interest.
Approval of the research protocol by an Institutional Reviewer Board
This study was approved by the ethics committees of Nagoya City University Graduate School of Medical Sciences. Written informed consent was acquired according to the World Medical Association Helsinki Declaration (in 1975) (IRB No. 60-23-0155).
Informed consent
Written informed consent was given by the patient for the publication of this article and the accompanying images.
Registry and the Registration No. of the study/trial
Not applicable.