A case of testicular dysgenesis syndrome with squamous cell carcinoma of the prostate harboring a CDK12 mutation
Abstract
Introduction
Primary squamous cell carcinoma of the prostate is rare, and genetic profiling of this disease has not been established yet.
Case presentation
We present a case of primary squamous cell carcinoma in a patient with testicular dysgenesis syndrome. The patient was diagnosed with prostate squamous cell carcinoma following intractable dysuria, and his serum prostate-specific antigen level was low. The patient had multiple lymph node and lung metastases, which led to administration of platinum-based chemotherapy. Additionally, targeted next-generation genome sequencing was performed to detect CDK12 mutations.
Conclusion
Early imaging studies should be considered, even if the patient's prostate-specific antigen level is low when dysuria persists despite medical treatment. To the best of our knowledge, this is the first reported case of primary squamous cell carcinoma with a CDK12 mutation in a patient with TDS.
Abbreviations & Acronyms
-
- BPH
-
- benign prostatic hyperplasia
-
- ICI
-
- immune checkpoint inhibitor
-
- mCRPC
-
- metastatic castration resistance prostate cancer
-
- MRI
-
- magnetic resonance imaging
-
- PSA
-
- prostate-specific antigen
-
- SCC
-
- squamous cell carcinoma
-
- TDS
-
- testicular dysgenesis syndrome
Keynote message
To the best of our knowledge, this is the first reported case of primary SCC of the prostate harboring a CDK12 mutation in a patient with TDS.
Introduction
Prostate SCC is rare, and accounts for only 0.5% to 1% of all prostate cancers.1 This unusual carcinoma has a poor prognosis due to the lack of standardized therapy. While precision medicine based on genomic profiling may serve as a viable treatment option, only one case report of prostate SCC genomic profiling is available to date.2
Several male gonadal dysfunction-related disorders, including, hypospadias, testicular cancer, and poor semen quality are believed to be symptoms of underlying diseases, with TDS reported to be a common factor in the context of these features.3, 4
We report a case of primary SCC of the prostate in a patient with TDS.
Case presentation
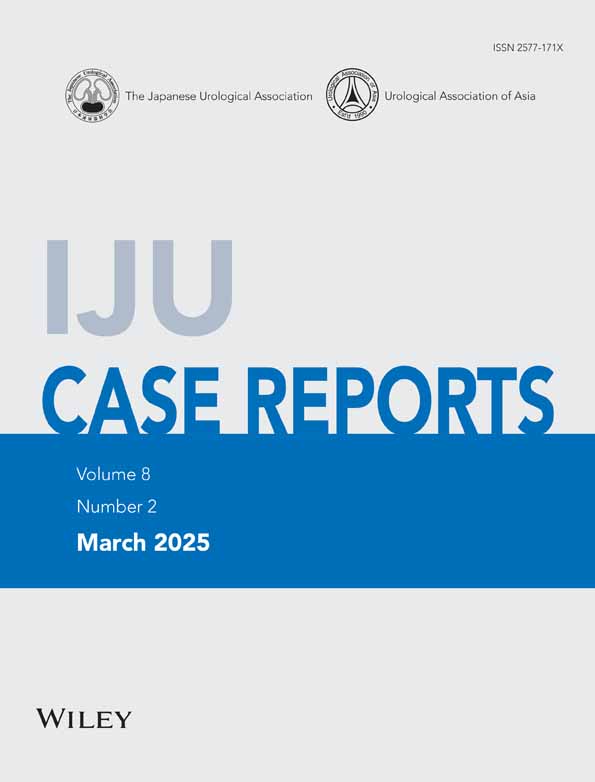
A 70-year-old man visited his physician with complaints of dysuria. Based on his medical history which included hypospadias and cryptorchidism, he was considered to have TDS. The patient's dysuria did not improve despite the administration of medication for BPH. He subsequently underwent MRI, which revealed a prostate tumor with extra-prostatic extension (Fig. 1). The patient was then referred to our hospital, where his serum PSA and testosterone levels were found to be <0.003 and 0.32 ng/mL, respectively. The patient had a history of hypospadias, and urethral stricture was considered as a differential diagnosis for dysuria. Cystourethroscopy was previously performed by the referring physician; however, it was reported to be difficult to insert. To evaluate for the presence of urethral stricture, we performed urethrography instead of cystourethroscopy, which revealed a defect in the prostatic urethra along with contrast leakage (Fig. 2). The leakage of the contrast agent was suspected to be iatrogenic, possibly related to urethral bougienage or cystoscopy performed at a previous institution; however, the exact cause could not be determined. We also performed the digital rectal examination. The prostate was palpated as a large hen's egg-sized, stony, and painless.

We performed a transperineal prostate needle biopsy. A cystostomy was performed concomitantly with the biopsy because we anticipated that the patient's dysuria would worsen. In addition, a temporary urethral catheter was placed postoperatively.
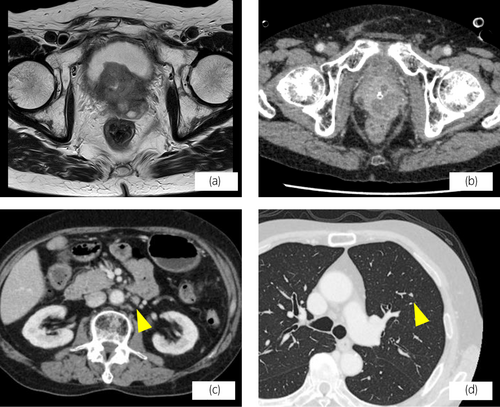
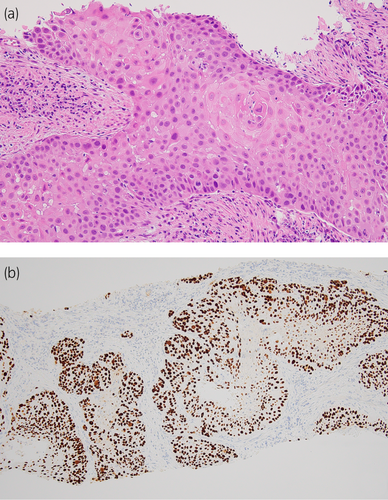
Pathological examination of a prostate needle biopsy sample revealed SCC of the prostate, based on the proliferation of atypical squamous epithelial cells with keratinization. Immunohistochemically, the tumor cells were positive for p40 and HM34βE12 which confirmed the diagnosis of SCC of the prostate (Fig. 3). The patient's serum SCC was 5.2 ng/mL (normal <1.5 ng/mL). Computed tomography revealed multiple lung metastases and lymphadenopathies (Fig. 1), and bone scintigraphy revealed no bone metastasis. Platinum-based chemotherapy was thus initiated. Genomic sequencing of prostate biopsy specimens revealed a genetic variant in CDK12 (P526fs*84), which led to the administration of an ICI. However, post several cycles of ICI therapy, the patient was unable to continue the treatment due to diarrhea and hyponatremia. His serum SCC antigen levels increased to a maximum of 15.8 ng/mL, and computed tomography revealed enlargement of the primary tumor and lung and lymph node metastases. Additionally, peritoneal and pleural dissemination and multiple bone metastases were also evident. After recovery from the adverse events, we reintroduced ICI; however, the patient's general condition continued to worsen and systemic therapy was thus ceased (Fig. 4).
Discussion
Primary SCCs of the prostate are extremely rare cancers that account for less than 1% of all prostate cancer cases.1 Although patients with primary SCC of the prostate often present with dysuria,2, 5 the lack of specific clinical symptoms and tumor markers renders the diagnosis of this rare carcinoma difficult.
Mott suggested five criteria for the diagnosis1: (1) a clear malignant neoplasm demonstrating invasion, disordered growth, and cellular anaplasia; (2) definite squamous features of keratinization, squamous pearls, and/or numerous distinct intercellular bridges; (3) the lack of any glandular or acinar pattern; (4) no prior estrogen therapy; (5) the absence of primary squamous cancer elsewhere, particularly in the bladder. While several therapies, including, prostatectomy, radiotherapy, and chemotherapy have been employed to treat SCC of the prostate,2, 6-8 no effective or definitive treatments have been established to date.
We detected a point mutation in CDK12, a cyclin-dependent kinase that contributes to DNA repair by regulating homologous recombination of DNA repair genes9 in the SCC biopsy sample of our patient. CDK12 variations have been frequently associated with prostate cancer with aggressive clinical features.10 A study in 2022 reported that CDK12 variations were most commonly detected in Japanese cases of mCRPC.10 However, a few patients with mCRPC harboring CDK12 mutations are known to have benefited clinically from ICIs.11 To the best of our knowledge, this is the first report of SCC of the prostate harboring CDK12 mutations. The clinical significance of CDK12 mutations in the SCC of the prostate remains unclear, and further accumulation of clinical data is needed.
TDS is believed to underlie a variety of male reproductive function-related disorders, including, undescended testes, hypospadias, impaired spermatogenesis, and testicular cancer.3, 4 Our patient had a history of undescended testes and hypospadias. Further, his serum testosterone level was within the castrated range when he was diagnosed with prostate cancer. Low circulating free testosterone levels are associated with a lower risk of prostate adenocarcinoma.12
The potential diagnosis of prostate cancer should be thus considered in patients presenting with dysuria and a history of sex development disorders, such as undescended testis and hypospadias. Toward this end, early imaging studies should be conducted, despite low PSA levels.
Conclusion
To the best of our knowledge, this is the first reported case of primary SCC of the prostate harboring a CDK12 mutation in a patient with TDS.
Author contributions
Yasuaki Murata: Writing – original draft. Takeo Kosaka: Writing – review and editing; conceptualization. Kohei Nakamura: Writing – review and editing. Yuto Baba: Writing – review and editing. Eri Arai: Writing – review and editing. Yota Yasumizu: Writing – review and editing. Kazuhiro Matsumoto: Writing – review and editing. Hiroshi Nishihara: Writing – review and editing. Mototsugu Oya: Supervision.
Conflict of interest
The authors declare no conflict of interest.
Approval of the research protocol by an Institutional Reviewer Board
Not applicable.
Informed consent
Written informed consent was obtained.
Registry and the Registration No. of the study/trial
Not applicable.