A case of bladder paraganglioma completely resected by transurethral endoscopic en-bloc resection of bladder tumor
Abstract
Introduction
En-bloc resection of bladder tumors is performed for bladder cancer with the goal of achieving precise tumor resection and providing an informative pathology specimen. We report the first case of a safely resected bladder paraganglioma by en-bloc resection.
Case presentation
A 57-year-old woman presented with an incidental bladder tumor detected on computed tomography. Cystoscopy revealed a 10 mm submucosal tumor. Magnetic resonance imaging indicated a suspected bladder paraganglioma, whereas endocrinological tests showed no abnormalities. The tumor was completely resected in one piece without an intraoperative increase in blood pressure or bladder perforation. Pathological examination revealed a bladder paraganglioma with negative surgical margins. No evidence of recurrence was observed at 9 months follow-up.
Conclusion
En-bloc resection of bladder tumors may be a useful approach for selected cases of bladder paragangliomas, potentially decreasing the risk of intraoperative blood pressure fluctuations and ensuring complete tumor resection.
Keynote message
Transurethral resection of bladder tumor (TURBT) has been performed in 20% of bladder paragangliomas. Even in patients with non-functional paragangliomas, intraoperative blood pressure fluctuations have been reported during conventional TURBT. We have successfully treated bladder paraganglioma with en-bloc resection of bladder tumor alone without any adverse events and intraoperative blood pressure fluctuations.
Abbreviations & Acronyms
-
- CT
-
- computed tomography
-
- ERBT
-
- en-bloc resection of bladder tumor
-
- MRI
-
- magnetic resonance imaging
-
- PPGL
-
- pheochromocytoma and paraganglioma
-
- TURBT
-
- transurethral resection of bladder tumor
Introduction
Paragangliomas are rare non-epithelial neuroendocrine neoplasms with the potential to metastasize.1 Bladder paragangliomas, which account for <0.05% of all bladder tumors, are thought to originate from the ganglia within bladder walls.2 ERBT is a transurethral surgical procedure for bladder cancer in which the tumor is resected in one piece. ERBT can provide a more informative pathology specimen and precise tumor resection than conventional transurethral resection of bladder tumors (cTURBT) with comparable complication rates.3 To our knowledge, no reports on the treatment of bladder paragangliomas with ERBT alone are available. Herein, we report the first case of a bladder paraganglioma that was safely treated with complete resection using ERBT.
Case presentation
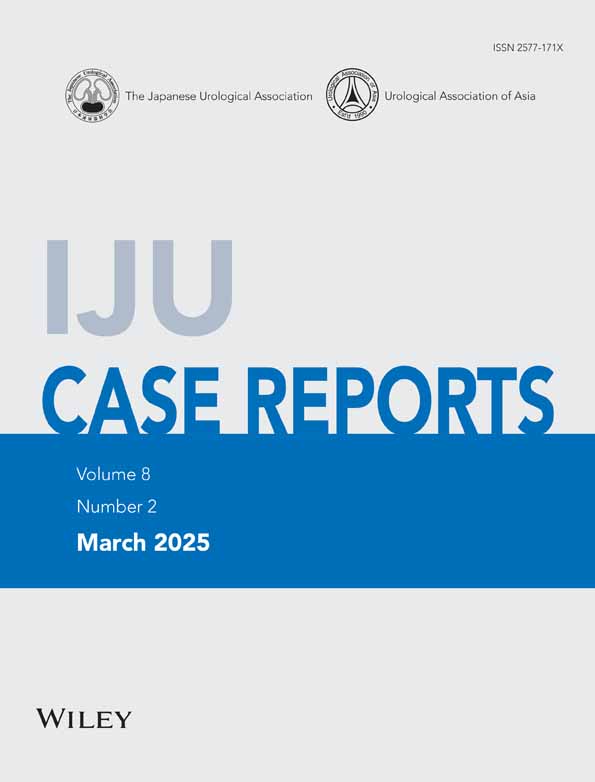
A 57-year-old woman with no relevant medical or family history underwent a contrast-enhanced CT following an abdominal examination that revealed gastric abnormalities. Although no malignant findings were detected in the gastrointestinal tract, an incidental bladder tumor was observed without evidence of metastasis (Fig. 1a). Cystoscopy showed a 10 mm submucosal tumor on the anterior wall of the bladder (Fig. 1b). Urine cytology results were classified as class II. Bladder MRI was performed, and T2-weighted imaging revealed a circumscribed tumor with moderate signal intensity in the bladder wall (Fig. 1c). Diffusion-weighted imaging (b = 1000) showed high signal intensity in the same lesion, and apparent diffusion coefficient maps showed low signal intensity (Fig. 1d,e). Dynamic contrast-enhanced images of the early phase showed an enhancement in the tumor, suggesting bladder paraganglioma (Fig. 1f). The muscle invasion was not demonstrated on MRI. There were no reported symptoms, including headache or palpitations. Her blood pressure was 94/61 mmHg, and her urinary metanephrine level was 0.18 mg/day, which was within the normal range.
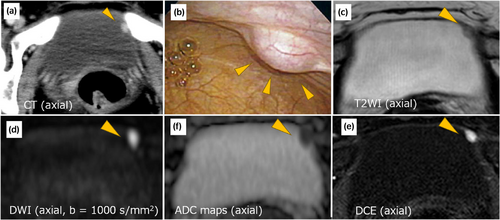
The patient was preoperatively diagnosed with non-functional bladder paraganglioma. To avoid making a direct incision into the tumor, we performed surgical resection using ERBT as follows (Fig. 2). First, a sufficient surgical margin was marked around the tumor. A circular incision was made using a needle electrode to ensure an adequate surgical margin. Finally, the tumor was resected in one piece without cutting into the tumor. A 26 Ch resectoscope (Olympus, Tokyo, Japan) and bipolar generator (THUNDERBEAT, Olympus) were used. She did not receive perioperative adrenergic blockers as recommended by the endocrinologist. The operative time was 21 min. The intraoperative blood pressure was stable throughout the procedure, and postoperative hypotension was not observed. The urethral catheter was removed on postoperative day 3, and the patient was discharged without adverse events.
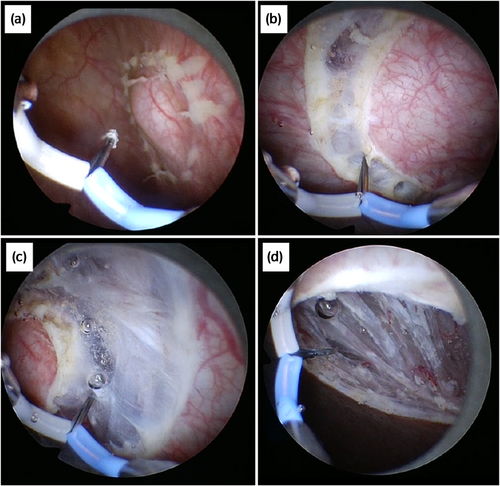
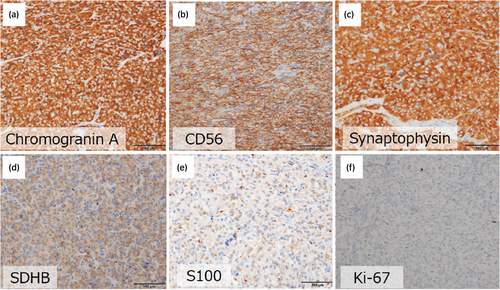
The resected tumor measured 16 × 14 mm in size. Pathological examination revealed a characteristic growth pattern with solid nests known as the Zellballen appearance, with negative surgical margins (Fig. 3). Immunohistochemical evaluation supports a pathological diagnosis of bladder paraganglioma (Fig. 4). The Ki-67 labeling index was <1%. Pathologically, the muscle invasion was not observed. Genomic analysis revealed no apparent mutations associated with paragangliomas, including the succinate dehydrogenase complex. No signs of local recurrence or distant metastasis were observed at 9 months follow-up.
Discussion
Bladder paragangliomas are rare and account for only 1% of all pheochromocytomas and paragangliomas (PPGLs).4 Forty percent of the retroperitoneal PPGLs are reported to be non-functional.5, 6 Preoperative adrenergic blockers are recommended to prevent unpredictable increases in blood pressure during surgery for non-functional bladder paragangliomas according to the guideline.7 However, in this case, preoperative adrenergic blockers were not administered as a result of careful discussion with the endocrinologist mainly due to the small tumor size and the use of ERBT. Finally, EBRT achieved no apparent increases in the intraoperative blood pressure.
A systematic review reported that 20%, 70%, and 10% of the patients underwent TURBT, partial cystectomy, and total cystectomy, respectively.4 The reported size of bladder paraganglioma ranges from 1.6 to 5.4 cm.8 For large bladder paragangliomas, complete removal from the urethra may be challenging, and thus partial or radical cystectomy may be necessary. A combination of partial cystectomy and ERBT has also been reported.9 cTURBT for bladder paraganglioma causes an intraoperative increase in blood pressure owing to a direct incision into the tumor.10 Given that intraoperative blood pressure fluctuations have been reported in patients with preoperatively diagnosed non–functional bladder paragangliomas, careful resection is recommended, and ERBT may be a suitable option.11 Because ERBT does not involve direct incision into the tumor, it may reduce the risk of intraoperative blood pressure fluctuations compared to cTURBT.3 In appropriately selected cases, this method allows for complete resection with the least invasive approach compared to partial or total cystectomy.
In conclusion, this case demonstrates complete and safe resection of bladder paraganglioma by ERBT alone. Considering the risk of intraoperative blood pressure fluctuations and to ensure complete resection, ERBT may be a useful approach in selected cases of bladder paraganglioma.
Acknowledgments
Not applicable.
Author contributions
Shunya Matsumoto: Conceptualization; writing – original draft. Yudai Ishikawa: Writing – review and editing. Hiroshi Fukushima: Writing – review and editing. Kouhei Yamamoto: Writing – review and editing. Kazutaka Tsujimoto: Writing – review and editing. Koichiro Kimura: Writing – review and editing. Yuma Waseda: Writing – review and editing. Hajime Tanaka: Writing – review and editing. Soichiro Yoshida: Writing – review and editing. Yasuhisa Fujii: Supervision.
Conflict of interest
The authors have no conflicts of interest to declare.
Approval of the research protocol by an Institutional Reviewer Board
Not applicable.
Informed consent
Written informed consent was obtained from the patient.
Registry and the Registration No. of the study/trial
Not applicable.