Revisiting Afghanistan's Drug Policy: A Policy Analysis of Eradication, Harm Reduction, and Economic Dependencies
ABSTRACT
Background
Afghanistan's responses to illicit drugs have oscillated between punitive eradication and limited harm-reduction initiatives. Two decades of heavy external spending, entrenched conflict, and an economy intertwined with opium have blunted policy effectiveness.
Methods
Guided by Walt and Gilson's policy-triangle, we undertook a document-based review (2001–2024). Twenty-seven national laws, strategies, and analytical reports were retrieved from government and multilateral repositories. Data were coded thematically using Braun-and-Clarke's six-phase approach to map policy content, actors, context, and implementation barriers.
Results
Four themes emerged. First, Afghan drug policy has passed through distinct phases—post-2001 tolerance, eradication campaigns, a harm-reduction window, and the current Afghan government's prohibition—each shaped by shifting political economies. Second, a complex actor constellation spans ministries, insurgent groups, multilateral donors, and opium-dependent farming communities, often with conflicting incentives. Third, implementation is hampered by corruption, chronic insecurity, rural poverty, and a shrinking treatment infrastructure (113 centres for an estimated 1.5 million users in 2024). Fourth, persisting failures fuel cycles of addiction, rural impoverishment, and insurgent financing, while recent poppy bans have accelerated a pivot to methamphetamine production.
Conclusion
Sustainable progress demands moving beyond short-term enforcement toward an integrated rural-development and public-health agenda. Priorities include: (i) secure livelihood alternatives for farmers; (ii) restoration and scale-up of evidence-based treatment and harm-reduction services; (iii) transparent governance mechanisms that engage local communities. A balanced, context-sensitive policy mix offers the best prospect of reducing drug-related harm while addressing the structural drivers that have long frustrated Afghan counter-narcotics efforts.
1 Introduction
Drug abuse encompasses a wide range of psychoactive drugs that have the potential for misuse, dependence, and adverse health consequences. These drugs include alcohol, nicotine, cannabis, opioids, cocaine, amphetamines, and other illicit or prescription drugs with abuse potential. Among these, alcohol and nicotine are the most commonly used drugs globally, with alcohol use disorder and nicotine use disorder representing significant public health concerns. Cannabis remains the most frequently used illicit drug, whereas opioids, including heroin and prescription pain relievers, are responsible for the highest number of drug-related fatalities. Stimulants such as cocaine and amphetamines also contribute to drug use disorders, particularly among young adults [1]. The societal impact of illicit drug use is notably characterized by adverse health outcomes among its members and the imposition of significant financial burdens on individuals, families, and the broader community [2]. Drug abuse is associated with several common risk factors and comorbidities. Younger age, male sex, lower educational attainment, unemployment, and lower income increase the risk of drug use disorders. Additionally, psychiatric conditions such as anxiety disorders and other drug use disorders significantly elevate the likelihood of developing an addiction. Medical comorbidities, including HIV, hepatitis C, bacterial infections (such as endocarditis and cellulitis), and neonatal abstinence syndrome in newborns, are prevalent among people who inject drugs (such as opioids). Social, economic, and legal factors further complicate access to healthcare, often leading to undertreatment of these conditions. According to WHO estimates, injection drug use is responsible for about 10% of HIV infections worldwide and 30% of cases outside Africa [3]. Drug abuse not only increases the risk of cancers such as lung, gastric, oral, colorectal, and liver cancer but also severely impacts overall quality of life. Tobacco and alcohol exposure contribute to these cancers, while poor dietary habits further elevate susceptibility. Addiction also leads to physical and mental health deterioration, causing increased pain, lower vitality, and reduced social functioning. Economic struggles and limited healthcare access further worsen the well-being of individuals with drug use disorders [4, 5].
Globally, 6% of the population aged 15–64 has used illicit drugs at least once. Over 140 countries report injecting drug use, while more than 120 report HIV infections among drug users [6]. Given the concerns about the medical, social, legal, and health consequences, drug abuse has emerged as a substantial global policy concern [7]. Various countries have employed distinct strategies to address this challenge, with the “war on drugs” (WOD) representing a commonly utilized approach over the years [8]. Under this policy, strict measures such as imprisonment and the death penalty have been implemented for buying, selling, and using drugs [9]. However, numerous global studies have scrutinized the outcomes of this policy, revealing that the anticipated benefits of a strict approach, such as reducing drug abuse and relapse, did not materialize [10]. Consequently, these findings underscore the need for an alternative strategy in addressing drug abuse, emphasizing another policy known as harm reduction (HR) [11].
Harm Reduction International (HRI) defines harm reduction as policies, programs, and practices that aim to minimize the negative health, social, and legal impacts associated with drug use. Grounded in justice and human rights, drug policies and laws focus on positive change and working with people without judgment, coercion, discrimination, or requiring that they stop using drugs as a precondition for support [12].
1.1 Global Drug Abuse Policies
Drug abuse policies vary across different nations, with countries adopting distinct approaches depending on sociopolitical influences, public health priorities, and legal frameworks. Iran and the United States, despite their differences in governance and ideology, have both transitioned from strictly punitive measures to incorporating harm reduction and treatment-oriented strategies.
In Iran, drug abuse policies have evolved from a strict war-on-drugs approach to incorporating harm reduction and treatment-based strategies. Initially, Iran focused on criminalization and compulsory treatment, but the rapid spread of HIV among people who inject drugs (PWID) and the increasing prevalence of drug use disorder led to policy shifts. Since 2004, Iran has adopted harm reduction measures, including methadone maintenance therapy, needle exchange programs, and drop-in centers providing healthcare and social support. However, policy implementation fluctuates depending on political leadership, with ideological and governmental influences playing a significant role in shaping drug policies [13].
Similarly, the United States follows a dual approach to drug abuse laws and punishments, combining criminal enforcement with public health strategies. Historically, drug policies have been punitive, emphasizing strict enforcement, incarceration, and mandatory minimum sentences, particularly under laws such as the Controlled Drugs Act and the Anti-Drug Abuse Act. However, in recent years, there has been a shift toward treatment-oriented approaches, recognizing drug use disorder as a public health issue rather than solely a criminal offense. At the federal level, penalties vary based on drug type, quantity, and intent (possession, distribution, or trafficking). While simple possession can lead to fines and imprisonment, trafficking carries harsher sentences, including mandatory minimums. Some states have decriminalized or legalized certain drugs, such as marijuana, reflecting a growing trend of harm reduction and alternative sentencing programs. Additionally, drug courts and diversion programs have been introduced to offer treatment instead of jail time for nonviolent offenders, aiming to reduce drug relapses. The US also enforces harm reduction policies like the increased availability of naloxone for overdose prevention and Good Samaritan laws, which protect individuals seeking medical help during an overdose from prosecution [14, 15].
The US has also prioritized increasing access to medication-assisted treatment (MAT) with medications such as methadone, buprenorphine, and extended-release naltrexone, which have been shown to improve treatment outcomes. However, challenges remain in expanding access to these treatments due to provider shortages and stigma surrounding opioid use disorder. Additionally, the US has focused on overdose prevention by broadening the availability of naloxone, an opioid overdose reversal drug. The Helping to End Addiction Long-term (HEAL) Initiative, funded by the National Institutes of Health (NIH), aims to enhance research on pain management, opioid addiction treatment, and alternative therapies. Despite these efforts, barriers such as regulatory restrictions and disparities in access to care persist, necessitating continued policy adaptations to effectively combat the opioid epidemic [3].
1.2 Drug Abuse in Afghanistan
Afghanistan has a complex history of drug production and abuse, largely influenced by sociopolitical factors, including ongoing conflict and instability. The production and availability of opium have significantly contributed to widespread addiction, impacting both public health and security in the region [7]. Opium is the drug most commonly abused in Afghanistan, consistent with its status as a major global producer of opium. The use of opium has historical roots and is influenced by its availability, owing to domestic production. Ongoing conflicts have contributed to increased drug abuse, with displacement, unemployment, and psychological trauma exacerbating the issue. This instability makes the implementation and maintenance of effective drug treatment programs challenging. Additionally, societal factors such as cultural norms and gender-based restrictions have a significant impact on access to treatment. Women face particular challenges in accessing drug treatment services due to societal barriers [8].
In 2001, Afghanistan had around 200,000 users of opium and heroin, but by 2015, this number had surged to between 1.9 and 2.4 million people. The 2015 Afghanistan National Drug Use Survey (ANDUS) found that drug use impacted about one-third of households, with 2.9–3.6 million people testing positive for drugs. Afghanistan's adult drug use rate was 12.6%, more than double the global average of 5.2%. The survey also noted that 16.1% of men and 9.5% of women in Afghanistan used drugs, with opioids being the most commonly used drugs among all groups, except urban women, who preferred cannabinoids, which were the second most prevalent drug overall. Benzodiazepines were the third most commonly used medication, with an estimated 1.4% of adults using them. Barbiturates and alcohol were used at similar rates: approximately 0.2% among adults and 0.1% in the general population. Additionally, amphetamine-type stimulants were used by approximately 0.5% of adults. These high rates of drug use highlight the availability of drugs and reflect the social and economic challenges Afghanistan has faced over the past 40 years [8].
Afghanistan plays a significant role in global illicit drug production, contributing 85% of the world's opium in 2020 [16]. The opium economy has historically accounted for 10%–15% of Afghanistan's GDP, generating billions of dollars annually, sustaining both livelihoods and insurgent groups. Poppy cultivation in Afghanistan has historically been concentrated in the southern and western provinces, particularly Helmand, Kandahar, and Farah, which served as the epicenter of opium production for the past two decades, including through 2023. However, in 2024, cultivation patterns shifted significantly, with over two-thirds of opium production relocating to the northeastern provinces, particularly Badakhshan. This geographic shift reflects changing enforcement dynamics, evolving trafficking routes, and local adaptations to counternarcotics measures implemented by the Islamic Emirate of Afghanistan (IEA) in 2022. Most opium produced in Afghanistan is transported out of the country, contributing to its role as a major global supplier [17]. Afghanistan remains a major producer of cannabis resin, ranking as the second-largest reported origin of global cannabis resin seizures. However, following the IEA's 2022 ban on poppy cultivation, opium production has sharply declined, leading traffickers to shift from heroin processing to methamphetamine production. Unlike conventional synthesis methods, Afghan meth is derived from wild ephedra plants, a naturally abundant precursor, making production both cost-effective and difficult to regulate. This transition has been reflected in record meth seizures across Pakistan, Iran, and Central Asia, as well as increasing detections of Afghan meth in European drug markets. As heroin profits dwindle, methamphetamine has emerged as a critical economic substitute, sustaining traffickers, traders, and farmers seeking alternative revenue sources. Meanwhile, cannabis cultivation continues despite a March 2023 ban, with enforcement remaining inconsistent and trafficking networks persisting, leading to rising prices in illicit markets [16, 17].
The U.N. found that drug abuse in Afghanistan is linked to domestic violence, unemployment, and poverty. Family members of drug users noted that many lost their jobs after beginning drug use, and nearly 75% reported that it led to severe financial problems. Furthermore, schooling and education in Afghanistan face significant challenges, and the already low school attendance rates drop further when children are forced to leave school because of family members' drug use. Lastly, drug abuse leads to an increase in criminal behavior in both men and women, although the increase is more pronounced in men [8].
The US-led war on drugs in Afghanistan proved to be a costly failure, ultimately exacerbating the very problems it sought to resolve. Following the US invasion in 2001, which aimed to dismantle the Taliban's government of Islamic Emirate of Afghanistan (IEA), policymakers also sought to eliminate Afghanistan's opium economy, believing it was a major source of insurgent funding. Ironically, before the US invasion, opium cultivation in Afghanistan had reached its lowest levels at the end of Taliban rule. In 2000, the IEA implemented a strict ban on opium production, leading to a 95% reduction in cultivation. However, after the US ousted the Taliban in late 2001, opium production rebounded rapidly. Despite spending approximately $8.4 billion on counternarcotics efforts between 2002 and 2014, the United States failed to curb Afghanistan's opium industry. Instead, cultivation surged from 76,000 hectares in 2002 to a record 209,000 hectares in 2013, making the country the dominant supplier of the world's illicit opium. Rather than eliminating the drug trade, US eradication efforts pushed production into the black market, fostering instability and enabling the Taliban to regain control over the industry. As smaller producers were targeted, the opium economy became increasingly concentrated in the hands of insurgents, who used drug revenues to fund their operations. The criminalization of poppy cultivation further alienated rural farmers, many of whom turned to the IEA for protection. Additionally, corruption within Afghan institutions deepened as officials at various levels profited from the illicit drug trade. Far from weakening the insurgency, the war on drugs strengthened it, ensuring that the insurgents remained well-funded and deeply entrenched. By the time US combat forces withdrew from Afghanistan in 2014, it was clear that the counternarcotics campaign had not only failed to achieve its objectives but had also become closely linked to the ongoing conflict and continued opium production in Afghanistan [18].
Despite the turmoil, political instability, and the American commitment to a prohibitionist War on Drugs model, the post-Taliban era in Afghanistan was also marked by significant harm reduction initiatives. Recognizing the limitations of eradication-focused approaches, the Afghan government integrated harm reduction into its National Drug Control Strategy in 2003, making explicit references to such interventions in national policy documents. By 2005, the ministries of public health and counternarcotics launched a National Harm Reduction Strategy, approving numerous harm reduction and treatment programs. The Afghan government continued to prioritize harm reduction in national policies, including the National Drug Demand Reduction Policy (2012–2016) and the National AIDS Control Program, despite opposition from conservative groups advocating abstinence-based solutions aligned with Islamic laws on intoxicants. When the IEA regained control in August 2021, economic and social disruption followed, displacing millions and reducing access to health care. In April 2022, the IEA reinstated its pre-2001 policy of criminalizing drug use to boost international credibility. The IEA has shifted its aproach to drug use by reducing support for harm reduction and HIV prevention programs. their current strategy focuses on detaining people who use drugs (PWUD) and placing them in rehabilitation centers. these facilities are often overcrowded and have limited access to medical care, food, hygiene supplies and mental health services [19].
As of 2021, Afghanistan had 129 drug treatment centers, a number that decreased to 113 by December 2024, according to the UNDP. Despite this reduction, the availability of treatment services remains insufficient to meet the needs of the estimated 1.3–1.6 million individuals requiring support, leaving a significant gap between demand and available care [7, 12, 16, 20]. However, the Afghanistan drug treatment study demonstrated that residential, outpatient, and home-based Drug Treatment Centers (DTCs) positively impacted patients' lives. Significant reductions in illegal drug use and criminal behavior were observed. While the evaluation findings are crucial for public health in Afghanistan, improvements are necessary, particularly in increasing treatment capacity. Moreover, medically assisted treatment (MAT) approaches are essential for expanding capacity, and efforts should focus on building infrastructure to support the implementation and monitoring of MAT and enhance current treatment strategies [7].
Considering the dimensions of drug problems in Afghanistan, it is critical to evaluate drug abuse policies in this developing country. The purpose of this analysis was to scrutinize drug abuse policies in Afghanistan and seek potential solutions to the multifaceted problems related to drug abuse in the country. This study aims to evaluate the effectiveness and challenges of Afghanistan's drug abuse policies and lay the foundation for future evidence-based approaches to address ongoing issues.
2 Methods
2.1 Design
This study conducts an evaluative analysis of Afghanistan's drug abuse policies over the decades, examining shifts in approach, effectiveness, challenges, and the broader impact and consequences of these policies over time. We employed a structured, systematic approach to search, select, and critically analyze relevant documents from both grey literature and peer-reviewed sources. This method aimed to highlight key concerns for stakeholders in improving policy effectiveness. By examining these materials, we identified gaps in legal and policy frameworks, providing a strong and balanced basis for informed discussions and recommendations.
2.2 Data Extraction
In this study, data were extracted from policy documents, literature reviews, and stakeholder reports. Electronic documents were obtained from the official sites of the Ministry of Counter Narcotics, UNODC, UNDP, World Bank, and WHO. A systematic search strategy was employed across multiple databases, including PubMed and Google Scholar, using combinations of keywords such as “drug abuse”, “policy analysis”, and “Afghanistan”. The inclusion criteria encompassed policy documents, research studies, and reports published between 2001 and 2024 that focused on drug abuse policies, their implementation, and their impact in Afghanistan. We screened titles and abstracts for relevance, followed by full-text reviews. Quality appraisal of included documents was conducted based on authorship credibility, methodological transparency, and publication source. Data extraction was guided by a standardized form, capturing variables such as policy objectives, implementation strategies, reported outcomes, barriers to success, and socioeconomic impacts. Only English-language sources were included.
2.3 Data Analysis
The Walt and Gilson Policy Triangle Framework, widely used in health policy analysis, organizes policy evaluation into four key domains: context, actors, process, and content (Figure 1) [21]. In this study, this Framework was used to guide the analysis of Afghanistan's drug abuse policies.
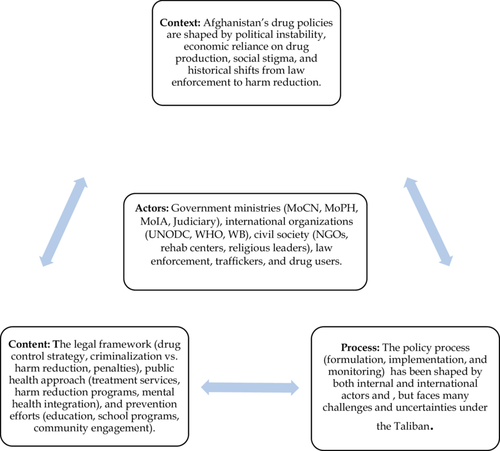
For context analysis, we focused on understanding the background conditions that influenced drug policy in Afghanistan. We reviewed national policy documents, historical reports, and international publications from organizations like UNODC, WHO, and the World Bank. We looked for political changes, such as changes in government, major economic factors like the opium economy, social attitudes towards drug use, and important historical events. To do this, we read the introductions, situation analyses, and background sections of the documents and took notes on important factors that shaped the environment around drug policy.
For actor analysis, we identified and mapped the key individuals and organizations involved in making and influencing drug policies. We reviewed government reports, legislative documents, and international publications to find out who the main actors were. These actors included government ministries, international organizations, nongovernmental organizations (NGOs), and community leaders. We noted their roles, their levels of influence, and their interests or positions.
For process analysis, we studied how the policies were made, implemented, and monitored. We read strategic plans, implementation reports, and evaluation documents from the government and international agencies. We tried to understand how drug policy issues were put on the agenda, how decisions were made, how the policies were rolled out in practice, and what challenges were faced during implementation. We also paid attention to how different organizations coordinated their activities and where there were delays or failures. We used timelines and summaries to organize this information and to track how the policy processes developed over time.
For content analysis, we carefully reviewed the actual content of Afghanistan's drug laws and policies. We focused mainly on important documents like the Counter Narcotics Law (2005, revised 2009) [22], the Afghan National Drug Action Plan (2015–2019) [23], U.S. Counternarcotics Strategy for Afghanistan (2007) [24], and National Drug Control Strategy (NDCS) of Afghanistan (2006) [25]. We read these documents in detail and used thematic analysis to identify major goals, strategies, and target groups. For example, we looked for whether the policies focused more on the eradication of drugs, harm reduction strategies, or public health responses. We also paid attention to how the content of the policies changed over the years and whether they followed international recommendations for best practices.
To systematically extract and organize information, a two-phase approach was used. First, document review involved analyzing policy and legislative documents, research articles, and stakeholder reports. Data sources included the Counter Narcotics Law of Afghanistan (2005, revised 2009) [22], the Afghan National Drug Action Plan (2015–2019) [23], US Counternarcotics Strategy for Afghanistan (2007) [24], National Drug Control Strategy (NDCS) of Afghanistan (2006) [25], and reports from organizations such as UNODC, UNDP, WHO, and the World Bank. Research papers retrieved from PubMed and Scopus-indexed journals were also included. Each document was summarized in a structured data collection sheet capturing title, date, key actors, use of evidence, and a short summary.
A total of 27 documents met the inclusion criteria (Table 1).
| No. | Exact title | Year | Purpose/Key content |
|---|---|---|---|
| 1 | Afghanistan Drug Insights Vol. 1: Opium-poppy Cultivation 2024 | 2024 | UNODC brief giving latest provincial cultivation figures and price trends one-year after the IEA ban (UNODC). |
| 2 | Afghanistan Drug Insights Vol. 2: 2024 Opium Production and Rural Development | 2024 | Analyses yield, farmer income and socioeconomic impacts of continued poppy suppression (UNODC). |
| 3 | Afghanistan Drug Insights Vol. 3: Mapping of Facilities for Treatment of Substance-Use Disorders | 2024 | Nation-wide inventory of drug-treatment centres, service coverage gaps and humanitarian constraints (UNODC). |
| 4 | Afghanistan's Opium Drug Economy (World Bank Report No. 30903) | 2004 | Macro-economic assessment showing opium accounted for > ⅓ of national income and detailing value-chains (World Bank). |
| 5 | Drugs and Development in Afghanistan (World Bank Working Paper) | 2004 | Explores how illicit crops interact with rural livelihoods, governance, and aid effectiveness (World Bank). |
| 6 | Counter-Narcotics Law of the Islamic Republic of Afghanistan | 2005 | First comprehensive narcotics statute: schedules, penalties, special courts, and covert-operations powers (UNODC). |
| 7 | National Drug Control Strategy (NDCS) | 2006 | Government blueprint built on four pillar—interdiction, eradication, alternative livelihoods, demand-reduction (UNODC). |
| 8 | Afghan National Drug Action Plan 2015–2019 | 2015 | Road-map aiming to cut cultivation 40%, disrupt trafficking, and scale treatment nationwide (FAO). |
| 9 | U.S. Counternarcotics Strategy for Afghanistan | 2007 | Aligns eradication, interdiction, and justice reform with counter-insurgency doctrine (State Department Archive). |
| 10 | Afghanistan Opium Survey 2023: Cultivation and Production After the Ban | 2023 | Remote-sensing survey confirming 95% drop in poppy area but sharp price spike (UNODC). |
| 11 | International Narcotics Control Strategy Report (INCSR) Vol. I | 2018 | Annual US review tracking Afghan seizures, legal reforms, and assistance programs (State Department). |
| 12 | INCSR Vol. I | 2021 | Updates on synthetic-drug emergence and enforcement capacity under IEA rule (State Department). |
| 13 | Drug Situation in Afghanistan 2021—UNODC Brief | 2021 | Concise data-snapshot on opium dominance, trafficking routes and nascent meth production (UNODC). |
| 14 | National Survey on Drug Use in Afghanistan (NSDA) | 2023 | UNDP household survey estimating 12.6% adult drug-use prevalence and profiling users (UNDP). |
| 15 | The Ups and Downs of Harm Reduction in Afghanistan (Lancet Regional Health SEA) | 2023 | Narrative review of two decades of HR programming and post-2021 roll-backs (The Lancet). |
| 16 | From Bad to Worse? Drug Use and Treatment in Afghanistan (GDPO Policy Brief 19) | 2023 | Policy analysis documenting collapse of treatment infrastructure and human-rights abuses in Afghanistan (Swansea University). |
| 17 | The War on Drugs in Afghanistan: Another Failed Experiment with Interdiction | 2016 | Independent Review article critiquing US eradication spending and insurgency pay-offs (JSTOR). |
| 18 | A Qualitative Assessment of Injection Drug Use and Harm-Reduction Programmes in Kabul (2006–07) | 2009 | Focus-group study comparing NSP users vs. non-users to inform service design (PubMed). |
| 19 | Implementing Harm Reduction for Heroin Users in Afghanistan, the Worldwide Opium Supplier | 2010 | Case-study of Médecins du Monde opium-tincture OST pilot and lessons for scale-up (PubMed). |
| 20 | Drug Use among the Afghanistan National Police: A National Assessment | 2012 | Urine-testing survey revealing 9% positivity (mainly THC/opioids) and policy gaps (PubMed). |
| 21 | Opiate Use, Treatment and Harm Reduction in Afghanistan: Recent Changes and Future Directions | 2012 | Commentary outlining progress and barriers to OST/NSP in a fragile setting (PubMed). |
| 22 | Baseline Assessment of Community Knowledge and Attitudes toward Drug Use and Harm Reduction in Kabul | 2012 | Cross-sectional KAP survey establishing pre-intervention stigma and awareness levels (PubMed). |
| 23 | Change in Attitudes and Knowledge of Problem Drug Use and Harm Reduction among a Community Cohort in Kabul | 2016 | Pre-post evaluation measuring shifts after HR outreach expansion (EMRO). |
| 24 | Understanding Injecting Drug Use in Afghanistan: A Scoping Review | 2022 | Systematic mapping of epidemiology, risk behaviours, and service gaps among PWID (PubMed). |
| 25 | A Review of Drug Policy in the Golden Crescent: Towards the Development of More Effective Solutions | 2014 | Comparative analysis of Afghanistan, Iran and Pakistan calling for evidence-based reforms (ScienceDirect). |
| 26 | Opium Trade, Insurgency, and HIV/AIDS in Afghanistan: Relationships and Regional Consequences | 2010 | Explores nexus between opium revenue, conflict financing, and infectious-disease spread (PubMed). |
| 27 | Surveillance, Addiction and Policy: The Examples of South Africa and Afghanistan | 2002 | Editorial on challenges of drug-use surveillance in conflict settings (SpringerLink). |
Two independent reviewers (MFW and MQA) assessed the documents separately to ensure consistency and minimize bias. Second, thematic analysis was conducted according to Braun and Clarke's [26] six-phase framework: familiarization with the data, generation of initial codes, searching for themes, reviewing themes, defining and naming themes, and producing the final report. Additionally, four researchers were involved in the coding and interpretation process to enhance the reliability of the findings. Themes and sub-themes were continuously refined through repetitive comparison with the research questions. To ensure trustworthiness, multiple strategies were adopted, including peer debriefing, triangulation of data across diverse sources (laws, national strategies, international reports), and detailed team discussions until full agreement was reached. An external validation session with a senior expert (former head of a rehabilitation organization) was conducted to critically review and confirm the relevance and accuracy of the identified themes and interpretations. This structured approach enabled a comprehensive and credible evaluation of Afghanistan's drug policy landscape from 2001 to 2024, highlighting evolutions in governmental and international approaches over time.
3 Results
We identified 27 relevant reports, documents, and research papers. The key documents reviewed in this study included The Counter Narcotics Law of Afghanistan (2005, revised 2009) [22], the Afghan National Drug Action Plan 2015–2019 [23], Afghanistan's Drug Insights 2024 (Volumes 1, 2, and 3) by UNODC [17], The War on Drugs in Afghanistan: Another Failed Experiment with Interdiction [18], Ups and Downs of Harm Reduction in Afghanistan [19], and From Bad to Worse? Drug Use and Treatment in Afghanistan [12]. The key themes that emerged from framework analyses of these documents include the evolution of Afghanistan's drug policies (2001–2024), key actors in drug policy development, Policy Implementation Challenges, and the consequences of drug policy failures (Table 2).
| Theme | Subtheme | Category | Subcategory/illustrative codes |
|---|---|---|---|
| 1. Evolution of drug policy (2001–2024) | 1.1 Policy phases | Security-driven eradication (2003–09); Harm-reduction turn (2005–10); Alternative-livelihoods (2009–21); Taliban prohibition (2022--) | Early tolerance for warlord alliances → aggressive eradication → partial HR integration → strict bans and synthetic shift |
| 1.2 Regulatory instruments | Laws and strategies | Counter-narcotics law 2005; NDCS 2006; action plan 2015–19 | |
| 2. Policy actors landscape | 2.1 State | Ministries and judiciary | MoCN, MoPH, MoIA, specialised drug courts |
| 2.2 International | Multilaterals and donors | UNODC, World Bank, US INL, Global Fund | |
| 2.3 Non-state | Insurgents and civil society | Taliban financing networks; NGO rehab providers | |
| 2.4 Community | Farmers and PWUD | Opium-dependent rural households; treatment-seeking users | |
| 3. Implementation challenges | 3.1 Governance | Corruption; weak enforcement | Bribes, selective policing, low institutional capacity |
| 3.2 Socioeconomic | Rural dependency; poverty | Lack of viable crops; price shocks; farmer indebtedness | |
| 3.3 Security | Conflict and insurgency | Violence hampers eradication and service delivery | |
| 3.4 Health-system | Treatment infrastructure gaps | < 15% coverage; decline from 129 to 113 DTCs (2021–24) | |
| 4. Consequences of policy failure | 4.1 Public health | Addiction and infectious-disease burden | Rising opioid and meth use; HIV outbreaks |
| 4.2 Socioeconomic | Entrenched rural poverty | Income loss after eradication; migration | |
| 4.3 Security | Insurgent financing | Drug revenue sustaining conflict | |
| 4.4 Environmental | Crop-switch effects | Ephedra harvesting for meth; land degradation |
3.1 Evolution of Afghanistan's Drug Policies (2001–2024)
The evolution of drug policies in Afghanistan from 2001 to 2024 has been shaped by the interplay between political regimes, economic factors, international influences, and the complex relationship between the Afghan state and the drug trade. Over this period, Afghanistan has seen dramatic shifts in its approach to drug control, transitioning from a government-backed counter-narcotics effort to IEA-imposed bans, each with varying degrees of enforcement, challenges, and effectiveness.
Afghanistan's drug abuse policies have been undermined by conflict, political instability, and geopolitical interests. A brief IEA-imposed opium ban in 2000 earned US support but shifted the trade to the Northern Alliance. Post-2001 conflict saw all sides funding operations through opium exports, making drug trafficking central to the war economy. These dynamics hindered stable policy enforcement, as actors adapted to maintain control of illicit markets, exposing the limits of drug policies detached from the political economy of conflict [27]. Cultivation of opium resumed after IEA's ousting by US-led forces [28] Following the 2001 invasion, the Afghan government, backed by Western powers, struggled to enforce eradication policies due to corruption, weak infrastructure, and farmers' economic dependence on opium [17]. The US initially tolerated opium cultivation (2001–2002) to secure alliances with warlords, then shifted to aggressive eradication (2003–2009), followed by an alternative livelihoods strategy (2009 onward), all of which failed to curb production [18]. By 2004, opium cultivation had risen from 74,000 hectares in 2002 to 131,000, contributing 33%–35% to GDP, with the total opium economy valued at $2.8 billion [29]. Recognizing the need for harm reduction, Afghanistan incorporated it into the 2003 National Drug Control Strategy, leading to the 2005 National Harm Reduction Strategy [19]. That same year, the Counter-Narcotics Law criminalized cultivation and trafficking, introduced strict penalties, and established special tribunals. It classified drugs into four categories, criminalized corruption and organized crime, and allowed law enforcement to conduct covert operations. Despite its comprehensive framework, enforcement was undermined by corruption, insurgent financing, and economic instability, limiting its effectiveness [22]. Between 2006 and 2009, Médecins du Monde (MdM) established Afghanistan's first harm reduction team through its Kabul program, delivering comprehensive services including antiretroviral therapy and methadone, which received official import certification in October 2009. A Training and Resource Centre (TRC) launched in 2008 was designated by the Ministry of Public Health as the national hub for drug user services, training NGO staff under the World Bank and Global Fund initiatives. This model aimed to scale up harm reduction nationally and to involve 20–40 NGOs potentially by 2011. To further strengthen this effort, the creation of the National Organization for Harm Reduction in Afghanistan (NOHRA) was proposed as an independent civil society body to lead strategy, innovation, and advocacy. Innovations included opium tincture as a unique, officially approved opioid substitution therapy (OST) option, and a new economic-social model to improve long-term treatment sustainability [30]. Although a national strategy for HIV prevention among injecting drug users had been introduced, practical implementation was weak [31, 32]. Only a few needle and syringe programs (NSPs) operated in Kabul, with no access to opioid substitution therapies like methadone, which were not legally permitted. Existing services struggled with limited resources, irregular supply distribution, and restricted coverage. Additionally, social stigma, police interference, and resistance from pharmacies made it difficult for drug users to access clean injecting equipment and support. Overall, harm reduction efforts existed but were insufficient and poorly integrated [31]. The 2006 National Drug Control Strategy (NDCS) aimed at interdiction, border security, and alternative livelihoods but faced resistance due to insurgency and economic instability [25]. The 2007 US Counternarcotics Strategy sought greater coordination with counterinsurgency efforts and targeted high-value traffickers, but the IEA's control over opium supply chains continued to fuel the insurgency against the republic government [24]. Between 2005 and 2010, the US allocated $2 billion for drug eradication but only $18 million for treatment, leaving 99% of drug users without access to care by 2015 [12]. Meanwhile, despite continued eradication efforts, opium cultivation reached unprecedented levels, with Afghanistan supplying 90% of the world's illicit opium by the mid-2000s [17]. From 2012 onward, the Afghan republic government and international actors made a renewed push to combat drug production, including increased law enforcement operations, poppy eradication, and drug trafficking interdiction efforts. This period marked a shift toward more coordinated efforts under the National Drug Control Strategy (NDCS), which emphasized reducing both supply and demand, promoting legal livelihoods, and strengthening institutional capacity. With support from partners like the United States, programs such as the Good Performers Initiative (GPI) rewarded poppy-free provinces with development aid, aligning counter-narcotics with broader state-building goals. Meanwhile, regional neighbors Pakistan and Iran—also part of the Golden Crescent—maintained similar goals and occasionally collaborated on border control and intelligence-sharing, although such cooperation was often limited by political tensions. Despite these efforts, corruption and weak enforcement continued to hinder long-term impact, pointing to the need for greater transparency and more sustainable, locally owned strategies in the evolution of Afghanistan's drug policy landscape [33]. By this point, the narcotics trade had become deeply embedded in Afghanistan's rural economy, with tens of thousands of farmers relying on opium cultivation as their primary source of income. Despite significant investments in antinarcotics initiatives, including efforts to promote alternative crops and strengthen law enforcement capacity, the Republic government struggled to maintain control in rural areas, where opium poppy cultivation continued to thrive. The ongoing insurgency, widespread corruption, and the lack of a coherent alternative development strategy meant that the drug trade remained a dominant force in the Afghan economy. During this period, the US and NATO forces began to gradually draw down their military presence, leaving Afghan security forces with greater responsibility for counter-narcotics efforts. This transition proved difficult, as the Afghan National Police (ANP) and other security agencies were often ill-equipped, poorly trained, and complicit in the drug trade [17]. The 2015 Afghan National Drug Action Plan (2015–2019) introduced a comprehensive approach focusing on reducing cultivation, disrupting trafficking networks, and improving treatment and prevention services. It aimed to reduce opium cultivation by 40%, strengthen law enforcement, and promote sustainable livelihoods. Strategies included alternative development programs, eradication efforts, and enhanced law enforcement, with a strong emphasis on expanding rehabilitation services and public awareness campaigns. However, challenges such as corruption, security instability, and insurgent financing hindered its success, and opium cultivation peaked at 328,304 hectares in 2017 despite counter-narcotics interventions [23, 28, 34, 35]. From 2012 to 2016, Afghanistan's National Drug Demand Reduction Policy marked a pivotal shift by formally incorporating harm reduction strategies, including the implementation of needle exchange and opioid therapy programs. This period laid the groundwork for changing public perceptions, which began to shift slowly in favor of harm reduction from 2016 onward. By 2020, these programs had expanded further, supported by increased media coverage and community outreach [19]. Public concern around drug use also evolved—from focusing on health risks to emphasizing social consequences such as family disapproval and imprisonment, reflecting the central role of the family unit in Afghan society. While acceptance of harm reduction grew, less than half of the participants fully endorsed such measures, and misconceptions remained, including beliefs that injecting was medically advised [36]. Following the IEA's return in 2021, a strict drug ban was issued in April 2022, leading to a 95% reduction in opium cultivation from 233,000 hectares in 2022 to 10,800 hectares in 2023. However, this caused a 92% decline in farmer incomes, shrinking the opiate economy by 90%, and led to a shift toward methamphetamine production and rising drug prices [28]. Enforcement has been inconsistent, with some Taliban factions allowing limited harm reduction efforts while others strictly punish drug offenses [17]. Afghanistan's drug abuse policies have been predominantly punitive, focusing on imprisonment and forced detoxification, which limits access to harm reduction services like Needle and Syringe Programs (NSP), Opioid Substitution Therapy (OST), and HIV testing. Fear of police harassment, stigma, and resource constraints has further hindered service uptake. Despite high incarceration rates among people who inject drugs (PWID), prisons have not been used for treatment delivery [37].
3.2 Key Actors in Drug Policy Development
Multiple actors have shaped Afghanistan's drug policies, reflecting shifting governance and competing priorities. Government institutions—both under the former Republic government and the current Islamic Emirate—have played central roles in drug control, including the Ministry of Counter-Narcotics (MCN), the Ministry of Public Health, the Ministry of Interior Affairs, and the Judiciary. These bodies have been responsible for prevention, treatment, law enforcement, and prosecution related to substance abuse. Although the Afghan government has repeatedly voiced its commitment to tackling narcotics, implementation has often been slow and inconsistent. The dissolution of the MCN in 2019 under President Ashraf Ghani marked a turning point, with its functions transferred to other ministries, primarily the Ministry of Interior and other agencies such as, The Criminal Justice Task Force and Counter Narcotics Justice Center (CNJC) [17, 19, 25, 28, 38]. The Afghan government transitioned from eradication-focused approaches under U.S. influence to harm reduction policies in the mid-2000s and back to strict enforcement under the IEA post-2021 [17, 19, 28]. From 2001 to 2024, international actors significantly influenced Afghanistan's drug abuse policies through funding, technical assistance, and strategic partnerships. The United States played a central role in counter-narcotics efforts, including law enforcement training, crop eradication, and alternative livelihood programs. Despite this, opium production remained high, and addiction rates persisted, highlighting challenges in policy effectiveness [17-19, 28, 34, 35]. International organizations like UNODC, WHO, and the World Bank provided technical and financial assistance, supporting initiatives such as harm reduction and the 2015–2019 Drug Action Plan, though these efforts were often undermined by corruption and instability [23, 29]. The IEA, despite banning opium in 2000 and again in 2022, has historically profited from the drug trade, taxing farmers and controlling trafficking networks to fund their insurgency efforts against the Republic government [24, 28]. Local communities and NGOs played a role in harm reduction, including needle exchange and treatment services, but these initiatives remained underfunded, particularly under IEA rule [12, 19]. The interplay between these actors has contributed to the cyclical nature of Afghanistan's drug crisis, where policy shifts often fail to yield lasting solutions.
3.3 Policy Implementation Challenges
A review of policy documents and implementation reports highlights several key obstacles to effective drug control in Afghanistan. Weak law enforcement has been a persistent issue, as corruption, limited resources, and political interference have significantly undermined the enforcement of drug laws. The 2005 Counter-Narcotics Law introduced stringent measures against cultivation and trafficking, but these were often selectively applied due to the influence of warlords, insurgents, and corrupt officials [18, 22, 29]. Economic dependence on opium remains another major challenge, as poppy cultivation has long served as a critical livelihood for Afghan farmers. Efforts to promote alternative crops under initiatives like the 2015–2019 Drug Action Plan met limited success due to inadequate financial incentives, security concerns, and a lack of viable market alternatives [17, 23]. Despite formal policy endorsements of harm reduction and opioid substitution therapy (OST) as early as 2012, implementation in Afghanistan was repeatedly hindered by political resistance, conflicting donor priorities, and interministerial gridlock, highlighting a persistent gap between policy and practice [39]. Harm reduction services, such as needle and syringe programs, were poorly recognized and rarely endorsed, even in communities where such services existed [40]. By 2015, this disconnect was evident in the extremely limited access to treatment, with only about 1% of drug users receiving formal care. Although some harm reduction initiatives—such as needle exchange programs and OST—were introduced with international support, their reach remained minimal. After the IEA takeover in 2021, these programs were drastically reduced or discontinued, further worsening the public health crisis and leaving many individuals with substance use disorders without support or services [12, 28]. These structural challenges have contributed to Afghanistan's enduring struggle with drug control, with policy shifts often failing to address the root causes of the opium trade.
3.4 Consequences of Drug Policy Failures
The failure of Afghanistan's drug policies led to severe social, economic, and security consequences. One of the most alarming outcomes was the rise in drug addiction, with an estimated 2.9–3.6 million Afghans suffering from substance use disorders by 2015 due to severe underfunding and an abstinence-based approach that often violated human rights [12]. Additionally, despite decades of eradication efforts and billions of dollars invested in counter-narcotics programs, Afghanistan remained the world's largest producer of opium, with cultivation peaking at 328,304 hectares in 2017, accounting for approximately 87% of the global opium supply [28]. The failure to curb drug production not only sustained Afghanistan's illicit economy but also significantly benefited the IEA, as various factions within the group profited from drug taxation and trafficking, using the revenues to finance their insurgency while simultaneously imposing bans to enhance their political legitimacy [24].
Since the IEA's return to power in 2021, their drug policies have had a notable impact on the country's economic conditions and public health situation. The 2022 opium ban led to a 95% decline in poppy cultivation, from 233,000 hectares in 2022 to just 10,800 hectares in 2023. While this policy dramatically reduced opium production, it also devastated the livelihoods of farmers, resulting in a 92% decline in income from opium sales and an estimated $1 billion loss in potential revenue [28]. Many former opium farmers have turned to methamphetamine production, as trafficking networks shift toward synthetic drugs, creating new challenges for drug enforcement and addiction treatment [17]. Additionally, the IEA's strict abstinence-based policies have led to the detention of people who use drugs (PWUD), compulsory rehabilitation in overcrowded facilities, and the dismantling of harm reduction services, raising concerns among health experts about increased risks of HIV, hepatitis C and tuberculosis [19]. Without viable economic alternatives for farmers and evidence-based treatment for addiction, Afghanistan's drug crisis continues to evolve, posing long-term threats to both its domestic population and global drug markets.
4 Discussion
Afghanistan's drug policies between 2001 and 2024 reflect a cycle of eradication, interdiction, harm reduction, and shifting political priorities. While policies have had varying degrees of success, long-term structural challenges—such as political instability, economic dependence on opium, and weak law enforcement—have limited their effectiveness. This discussion interprets the results in the context of policy effectiveness, gaps, and international comparisons, leading to recommendations for a more sustainable approach to drug control.
4.1 Policy Effectiveness Assessment
4.1.1 Eradication Policies: Short-Term Success, Long-Term Failures
Eradication efforts, particularly under US influence (2003–2009), resulted in temporary declines in opium cultivation but failed to provide sustainable alternatives for farmers, leading to recurrent production surges [18, 29]. Eradication efforts disproportionately affected small-scale farmers while leaving the larger drug trafficking networks intact. This led to a consolidation of the drug trade under IEA control, transforming them into a more financially resilient insurgent force [12]. Moreover, the eradication-first approach inadvertently fueled insurgency by driving rural communities toward the Taliban, who offered protection and financial incentives to opium cultivators. The $8.4 billion spent on counternarcotics yielded little success, as opium production nearly tripled between 2002 and 2013 [18]. The IEA's 2022 ban drastically reduced cultivation by 95% within a year, but this resulted in devastating economic consequences, pushing many toward methamphetamine production [28]. These findings highlight the limitations of prohibition-driven policies that do not account for economic realities.
4.1.2 Impact of International Funding: Dependency vs. Sustainability
International aid played a crucial role in counter-narcotics efforts, but funding was disproportionately allocated to eradication rather than treatment. The US spent $2 billion on eradication but only $18 million on addiction treatment between 2005 and 2010, leaving 99% of drug users without access to care by 2015 [12]. Short-term financial injections, such as those in the 2015–2019 National Drug Action Plan, often failed due to corruption and poor coordination [23]. International funding played a crucial role but created dependency rather than long-term sustainability. Programs like the Good Performers Initiative (GPI) rewarded provinces for reducing poppy cultivation, yet many farmers returned to illicit drug production after funding cycles ended. Additionally, corruption among Afghan republic officials further undermined these efforts, with financial incentives often being redirected for personal gain rather than genuine enforcement [18].
4.1.3 Treatment and Harm Reduction: Progress and Barriers
Harm reduction policies in Afghanistan gained traction in the mid-2000s, with the introduction of Needle Syringe Programs (NSPs) and Opioid Agonist Therapy (OAT) under the 2005 National Harm Reduction Strategy. These programs, aimed at reducing HIV and other infections and providing treatment for people who use drugs (PWUD), made significant strides but remained underfunded and politically contentious [19]. Despite progress, by 2021, IEA restrictions led to the dismantling of most harm reduction efforts. The failure to institutionalize harm reduction as a core public health strategy left drug users vulnerable, with mass incarcerations and forced detoxifications exacerbating health risks. The IEA's restrictive policies, including forced withdrawal approaches, lacked long-term efficacy and worsened the situation, further limiting access to treatment [17, 28].
4.2 Gaps and Challenges in Drug Policy Implementation
4.2.1 Lack of Coordination Between Key Actors
Afghanistan's drug policies have suffered from fragmented governance [17]. Despite efforts to address substance abuse in Afghanistan, major gaps were present in the implementation of drug policies. One key challenge was the lack of public awareness about existing laws and services. Most community stakeholders in Kabul were unaware that Afghan law mandates treatment—not incarceration—for first-time drug users, revealing a critical disconnect between policy and public understanding. This gap is further compounded by limited training for frontline workers, including police officers and pharmacists, who play a vital role in early intervention and referral. Additionally, the absence of culturally appropriate and accessible treatment services—especially in rural areas—has hindered effective policy execution [40]. The Afghan government oscillated between eradication and harm reduction, while international organizations like UNODC and WHO promoted treatment-based approaches [17, 23, 29]. The IEA's inconsistent stance—banning opium while historically profiting from its trade—further complicated implementation [28]. These policy shifts have created uncertainty, undermining long-term planning. The failure to integrate counternarcotics, economic development, and public health strategies by key actors has led to fragmented responses that have failed to produce meaningful results [12].
4.2.2 Security and Instability as Barriers to Policy Success
Decades of conflict have limited the effectiveness of drug policies. Many counter-narcotics efforts were sidelined due to more immediate security concerns, and regions under insurgent control often operated outside the reach of government interventions [17]. The insurgency and warlord influence allowed traffickers to operate with impunity, while law enforcement efforts were constrained by corruption and inadequate resources [18, 22, 29]. Even with legal frameworks such as the 2005 Counter-Narcotics Law, selective enforcement and political interference prevented meaningful implementation [22]. Similarly, Afghanistan's drug abuse policies within the ANP have struggled amid corruption, political instability, and weak institutional capacity. A 2009–2010 nationwide screening found a 9% drug-positive rate, mostly for THC and opiates. Positive cases declined from 21% to 4% during the testing period; however, proper implementation of the policy was hindered by poor infrastructure, lack of confirmatory testing, and political interference, which allowed selective enforcement and impunity [38]. The IEA's post-2021 policies have further exacerbated instability, leading to unpredictable enforcement and economic displacement [17].
4.2.3 Failure to Integrate Community Perspectives
Alternative development initiatives, such as the 2015–2019 Drug Action Plan, aimed to transition farmers away from opium but lacked community buy-in. Without viable economic alternatives, poppy eradication programs left farmers financially vulnerable, increasing reliance on illicit activities [17, 23]. A top-down approach to policy implementation, without grassroots participation, has repeatedly led to failure.
4.2.4 Shifting Taliban Policies Creating Policy Uncertainty
The IEA's return to power in 2021 introduced a strict drug ban, similar to their previous rule, which outright banned opium and illicit drug production. However, enforcement has been inconsistent. While some factions have allowed limited harm reduction programs, others have resorted to mass arrests and forced detoxification. The IEA's stance on drug control has varied between strict prohibition and tacit dependence on drug revenues, complicating long-term policy planning [17, 28].
5 Comparisons and Lessons From Other Countries
5.1 Colombia and Bolivia: The Limits of Eradication
Colombia and Bolivia's experiences with drug eradication offer important lessons for Afghanistan. Colombia and Bolivia's experiences with coca eradication highlight the limits of forced eradication without viable alternatives. In Colombia, US-backed efforts led to temporary declines but failed to address economic issues, pushing farmers toward insurgent groups and relying on unsustainable aid. However, Colombia also implemented positive policies, such as peace-building initiatives and the gradual integration of coca farmers into legal economies. The government improved rural development by creating sustainable alternatives to illicit crops and emphasizing economic incentives for legal agricultural production. Bolivia's approach with its “controlled cultivation” model allowed farmers to grow limited amounts of coca for legal use while promoting alternative crops. This conflict-sensitive, gradual approach avoided the displacement and insurgency linked to forced eradication and emphasized sustainability [41]. Afghanistan could consider a similar gradual transition strategy rather than abrupt eradication.
5.2 Portugal: A Public Health-Centered Approach
Portugal's decriminalization of drug use in 2001 significantly reduced addiction rates and drug-related deaths. By redirecting funding from enforcement to treatment, Portugal created a sustainable harm reduction model [42]. Full decriminalization may not be feasible in Afghanistan's context, given that mind-altering drugs are prohibited according to the Islamic Sharia. Nonetheless, Afghanistan could benefit from a shift toward public health-centered approaches, for example, expanding addiction treatment centers.
5.3 Iran: Regional Lessons in Harm Reduction
Iran's success with methadone treatment and needle exchange programs in the 2000s provides a regional example of harm reduction's effectiveness. Despite political conservatism, Iran institutionalized evidence-based treatment, reducing HIV and addiction rates among drug users [35]. Afghanistan, with its similar cultural and geographic challenges, could adopt a similar approach rather than continuing with purely punitive policies. Afghanistan's previous harm reduction programs showed potential before being dismantled post-2021 [19]. Reviving these initiatives under Taliban rule could help mitigate public health crises.
5.4 Policy Recommendations for the Future
5.4.1 Balancing Security and Public Health in Drug Policy
Afghanistan's drug policy must shift from a security-focused approach to one that integrates public health considerations. While the IEA's 2022 opium ban led to short-term reductions, its economic impact highlights the need for alternative strategies to prevent shifts to the illicit market. A more balanced approach should combine selective enforcement with harm reduction and rural development. This means targeting high-level traffickers rather than small-scale farmers, regulating production, and expanding harm reduction programs. Investment in rehabilitation should be prioritized, treating drug users as patients rather than criminals, and addressing public health alongside security concerns to ensure long-term success [12, 17, 28].
5.4.2 Sustainable Alternatives for Farmers
Afghanistan's alternative livelihood strategies must move beyond temporary aid and focus on long-term rural development. This includes investing in infrastructure, improving market access for legal crops, and offering financial incentives for farmers transitioning away from opium, methamphetamine, and other illicit drugs. Future initiatives should prioritize creating sustainable, viable legal markets, such as introducing regulated opium production for pharmaceutical use, following the models of India and Turkey. Supporting cash crops like saffron, nuts, and fruits, along with strengthening value chains, will help reduce dependency on poppy cultivation. Additionally, investing in rural infrastructure, irrigation, and market access is essential to make legal agriculture more profitable and sustainable, ensuring long-term success for farmers [12, 17, 18, 24, 29, 43].
5.4.3 Strengthening Addiction Treatment and Harm Reduction
Expanding evidence-based treatment is crucial for addressing drug addiction in Afghanistan. Harm reduction strategies, such as opioid substitution therapy and needle exchange programs, should be reinstated where possible, with international actors negotiating with the IEA to ensure these programs align with culturally acceptable frameworks. Despite the IEA's restrictive policies, there remains potential for expanding harm reduction services. International organizations and local NGOs should advocate for the continuation of methadone maintenance therapy and needle exchange programs, train community health workers to provide low-cost, decentralized treatment, and develop mobile treatment units to reach rural areas with high addiction rates. Increased international cooperation is essential to fund these programs independently of government restrictions, with advocacy efforts pushing for the restoration of harm reduction services as a condition for international aid [12, 19, 24].
5.4.4 Incorporating Community-Based Approaches
For Afghanistan's drug policy to succeed, it must adopt bottom-up strategies that engage local communities in decision-making. Programs that offer cooperative-based models, microfinance opportunities, and vocational training have proven successful in other post-conflict settings and should be prioritized in Afghanistan [12, 18, 19, 24]. To address the persistent implementation gaps in Afghanistan's drug abuse policies, broad-based educational initiatives are essential. These should target both the general public and key professionals—such as police officers and pharmacists—who often serve as gatekeepers to treatment and support. Building awareness of existing legal protections and treatment mandates can help reduce stigma and encourage early intervention. Engaging local communities—particularly religious leaders, tribal elders, and farmers—is crucial to improving policy compliance and legitimacy. Culturally adapted strategies, such as involving local mullahs and integrating religious instruction, can enhance acceptance of harm reduction and treatment services. Additionally, involving women and families in prevention and rehabilitation efforts and empowering former drug users to serve as peer educators can strengthen community-based responses. Embedding these approaches within Afghanistan's social and religious fabric ensures that legal reforms are supported by sustained community engagement and capacity-building among frontline service providers [12, 18, 19, 40]. Drug policy must be tailored to local economic conditions and cultural sensitivities, strengthening local governance structures to ensure accountability. By creating economic incentives aligned with local realities and fostering community-based harm reduction programs, we can reduce stigma, raise awareness, and provide peer support, ensuring that drug treatment and prevention are embraced by local communities [12, 18, 19, 24].
5.5 Limitations
The study could be limited by our understanding of the law, policy, and the development of analytical frameworks as the interpretations and views of the policymakers, lawmakers, and other researchers in this area of study could vary significantly.
6 Conclusion
Afghanistan's drug-control trajectory demonstrates that neither eradication nor prohibition alone can produce durable gains in a context where rural livelihoods, conflict financing, and weak institutions remain tightly coupled to the opium economy. Two decades of cyclical policy shifts have delivered only transient reductions in cultivation while treatment coverage has stagnated and synthetic-drug production has risen. Lasting progress hinges on reframing drug control as a development and public-health challenge. This requires: (1) sustained investment in legitimate income opportunities for poppy-growing communities; (2) nationwide expansion of evidence-based treatment, opioid-substitution therapy and harm-reduction services; (3) governance reforms that curb corruption and embed transparent monitoring; and (4) meaningful involvement of local leaders, religious authorities and civil society to enhance legitimacy and compliance. Embedding these elements within an adaptive policy framework will help prevent repeated cycles of prohibition-driven displacement, strengthen community resilience and ultimately reduce the health, economic and security burdens imposed by Afghanistan's drug economy.
Author Contributions
Mohammad Qais Azizi: conceptualization, writing – original draft, writing – review and editing, visualization, methodology, investigation. Mohammad Faisal Wardak: writing – original draft, writing - review and editing, conceptualization, visualization, methodology, investigation. Edris Afzali: conceptualization, writing – original draft, writing – review and editing, visualization, methodology, investigation. Ali Rahimi: writing – review and editing, conceptualization, supervision, visualization, methodology. Jerico Bautista Ogaya: writing – review and editing. Enayatollah Ejaz: writing – review and editing. Basir Ahmad Hasin: supervision, conceptualization. Mohammad Masudi: writing – review and editing. Don Eliseo Lucero-Prisno: supervision, writing – review and editing.
Acknowledgments
The authors express their gratitude to Jami University and the Global Health Focus for their invaluable support. The authors received no specific funding for this work.
Ethics Statement
The authors have nothing to report.
Consent
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Transparency Statement
The corresponding author, Ali Rahimi, affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
Data Availability Statement
Data sharing is not applicable to this article as no data sets were generated or analysed during the current study.




