Assessment of patient safety culture among healthcare providers in tertiary hospitals in Malaysia—A cross-sectional study
Abstract
Background and Aim
Patient safety culture is crucial for every health care institution, as a lack of it may harm patients seeking treatment. The current study aimed to identify the level of safety culture and assess the knowledge, attitude, and perception of patient safety culture among healthcare providers (HCPs') in tertiary hospital settings.
Methods
A cross-sectional study was conducted among HCPs from two private tertiary hospitals in Johor and Selangor. A structured validated questionnaire, including the Hospital Survey on Patient Safety Culture, was used to assess the level of patient safety culture in these hospitals.
Results
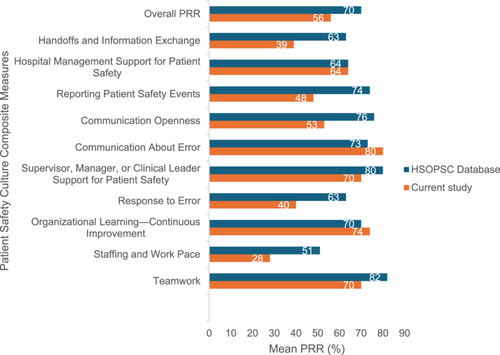
In this study, the calculated sample size was 320, and all 550 eligible participants from both hospitals were approached to participate. However, only 158 responded, resulting in a response rate of 49.38%. The majority of the HCPs (n = 110; 69%) rated their hospital as very good or excellent in maintaining an overall patient safety culture. The study revealed that communication about the errors (PRR = 80) and organizational learning and continuous improvement (PRR = 74) were good in their hospital settings. However, staffing and work pace (PRR = 28), response to errors (PRR = 40), reporting patient safety events (PRR = 48), and handoffs and information exchange (PRR = 39) were inadequate. These findings indicate the negative attitudes among HCPs and the need for further improvement to maintain a culture of patient safety.
Conclusion
HCPs in the study settings had optimal knowledge but negative attitudes towards the culture of patient safety in their organization. Inadequate staffing, work pace, and a lack of response to mistakes were commonly observed, which may increase the chances of errors and pose health threats to patients that need to be addressed immediately. Every healthcare organization is urged to address the issue of patient safety culture as a matter of urgency.
1 INTRODUCTION
Patient safety culture is crucial in preventing unintended or unexpected harm to patients while providing healthcare services. In the United States, approximately 400,000 hospitalized patients experience some form of preventable harm each year,1 while in Malaysia, 93.5% errors were deemed preventable, with 39.9% having the potential to cause serious harm.2 The term “safety culture” refers to the attitudes and behaviors towards patient safety that are evident when a patient enters a healthcare facility.3 The Royal College of Nursing has stated that attitudes and behaviors that discourage staff from learning from preventable incidents increase the risk of repeating the same incident.4 Organizations with a strong safety culture exhibit communication based on mutual trust, consensus on the importance of safety, and confidence in the positive effects of preventive measures.5 Successful implementation of patient safety strategies requires clear policies, strong leadership, qualified healthcare professionals, and information to inspire safety improvement.6
Intending to challenge and encourage healthcare institutions to strengthen patient safety, the Malaysia Patient Safety Goals (MPSG) 2.0 has integrated the World Health Organization (WHO) Global Patient Safety Challenges. It focuses on seven goals in hospitals; infection prevention and control, surgical safety, medication safety, transfusion safety, patient fall prevention, correct patient identification, and incident reporting and learning systems.'7 One key aspect of patient safety is the safe use of medication. It is crucial to actively advocate the use of adverse drug reactions and medication error reporting systems among HCPs. Despite the presence of several policies, rules, and regulations aimed at ensuring and maintaining a patient safety culture across the country, there remains a gap in patient safety awareness. Not all private hospitals are aware of the MPSG, and their performance in this area is not well-known.8 The Malaysia Country Health Plan recognizes that additional resources are necessary to provide better quality healthcare and improve patient safety.
The demand for healthcare services is increasing and the demand for private healthcare is similar to that in government facilities. Malaysia's total healthcare spending for 2019 amounted to RM 64.31 billion, with RM 33,371 million (52%) coming from the public sector and RM 30,575 million (48%) from the private sector. In 2019, private household out-of-pocket expenditure was the single largest private source of health financing, totaling RM 22.49 billion (74%).9 Patients are looking forward to receiving quality healthcare services, especially those who pay out of pocket.10-12
In Malaysia, the study of patient safety culture has been limited. Some studies have been conducted in hospitals and communities in urban areas,10-12 but tertiary care hospitals have largely been ignored, with no studies conducted in private tertiary hospitals in Johor or Selangor. Therefore, this present study was conducted to assess the knowledge, attitudes, and perceptions of HCPs on patient safety culture in tertiary care hospitals.
2 MATERIAL AND METHODS
2.1 Study design and population
A cross-sectional study was conducted over 6 months at two tertiary level hospitals namely Hospital-A, and Hospital-B, in Malaysia. HCPs, including doctors, nurses, pharmacists, physiotherapists, and nutritionists who were working at the study sites and willing to participate in the survey were included. Temporary staff, interns, or students were excluded from the study as they are not permitted to carry out tasks independently and must be supervised by senior faculty members to uphold the patient safety culture. Additionally, their turnover rate is high, so the study team believes their responses may not accurately reflect their approach to patient safety. The calculated sample size for the study was 320 HCPs. [Correction added on 28 November 2024, after online publication: The names of the participating hospitals have been removed.]
2.2 Study instruments
The survey included two questionnaires; a self-developed 21-item validated questionnaire to assess the HCPs' knowledge of patient safety, and the latest Hospital Survey on Patient Safety Culture (HSOPSC) questionnaire prepared by the Agency for Healthcare Research and Quality (AHRQ) to assess the attitudes and perceptions of HCPs towards patient safety culture.13
The knowledge assessment questionnaire consists of 21 items focusing on 5 domains of patient safety, such as awareness of errors, understanding of the human factor, proactive to avoid risks in security, system complexity and interrelationship, and openness in communication. The responses were grouped into Nett Positive Response (NPR) and Nett Other Response (NOR). NPR included responses marked as “strongly agree“ and “agree,“ while the sum of “strongly disagree,“ “disagree,“ “neither agree nor disagree” or “does not apply or don't know” were considered as NOR. The Positive Response Rate (PRR) was calculated using NPR from the total number of responses.11
The HSOPSC questionnaire consists of 40 items that measure the patient safety culture of an organisation. HCPs' attitudes and perceptions of patient safety were assessed using 32 items focusing on 10 domains/composites of patient safety, such as “teamwork, staffing, and work pace, organizational learning-continuous improvement, response to error, supervisor, manager, or clinical leader support for patient safety, communication about the error, communication openness, reporting patient safety events, hospital management support for patient safety, and handoffs and information exchange.”
The remaining eight items focus on the frequency of reporting patient safety events, overall rating on patient safety grade at the unit/area, and background details such as staff position, current unit/work area, years of experience, working hours, and their direct interaction with patients.13 Healthcare providers (HCPs) need to assess the overall patient safety grade of their unit/work area. They should use a 5-point Likert scale rating from poor to excellent to indicate how well patient safety aspects are being followed in their work area/unit.
The survey had a total of 61 items and varying responses. In this study, thirteen questions were negatively worded such as A3, A5, A6, A7, A9, A11, A13, A14, B2, C7, F3, F4, and F5 in the questionnaire to obtain fair responses from the participants. A positive response rate (PRR) was used to evaluate attitudes towards patient safety culture across various dimensions. The PRR was calculated using the formula outlined in the PSOPSC user's guide. The results were compiled based on the agreement indices provided in the PSOPSC guide. The questionnaire primarily used a Likert five-point response scale ranging from “strongly disagree” to “strongly agree,” with “strongly disagree” assigned 1 point and “strongly agree” assigned 5 points. Some items in the questionnaire used a frequency scale from “never” to “always,” with “never” receiving 1 point and “always” receiving 5 points. Scores of 4 and 5 were considered as “positive responses,” while scores of 1, 2, and 3 were categorized as “other responses.” The comparison of results was based on the number of positive responses versus the number of other responses.11-13 The questionnaire was validated and used in several countries for assessment of the culture of patient safety in hospitals14, 15 and again it was revalidated by the Department of Pharmacy Practice faculties of International Medical University (IMU) and selected HCPs from the study site. The questionnaire's consistency and reliability were measured using internal consistency based on Cronbach's α. The overall internal consistency of this study was excellent, with a Cronbach's α of 0.920. Additionally, the study showed that Cronbach's α ranged from 0.762 to 0.890 for eleven dimensions, indicating good internal consistency across all eleven dimensions (α > 0.7).
2.3 Data collection and analysis
A specially designed poster containing study information and a QR code linked to the questionnaires was distributed to eligible participants through the hospital email system. All HCPs have unique email IDs created by hospital management for official and professional communication with HCPs and hospital authorities. The invitation to participate in the current study was sent through the email system, which HCPs frequently check. Written informed consent was obtained from all participants before enrolling in the study. One reminder per week was sent to participants for a total of 4 weeks. Data analysis was conducted at the end of the fourth week. The collected data were tabulated and analyzed using the Statistical Package for Social Sciences (SPSS) version 28.0. Descriptive statistics were calculated and presented as tables, graphs, and frequencies. To determine the relationship between dependent and independent variables, logistic regression analysis was used. The crude and adjusted odds ratios, along with their respective 95% confidence intervals, were calculated. In multivariate analysis, all predictors associated with the outcome variable in bivariate analyses with p value < 0.25 were chosen to fit the logistic regression model. A P-value of <0.05 was considered statistically significant in the multivariate analysis.
3 RESULTS
3.1 Demographic characteristics of the respondents
In this study, the calculated sample size was 320, and all 550 eligible participants from both hospitals were approached to participate. However, only 158 responded, resulting in a response rate of 49.38%. Out of the 158 respondents, most were pharmacists (who have at least a bachelor's degree in pharmacy) or pharmacy assistants (diploma in pharmacy holders) (n = 67, 42.4%), followed by staff nurses (n = 32, 20.3%) and staff in supervisory roles such as supervisor, managers, department managers, clinical leaders, administrator or director) (n = 22, 13.9%). Most participants were from the pharmacy department (n = 57, 36.1%), followed by the medical or surgical ward (n = 21, 13.3%). In terms of working experience, most of them (n = 66, 42%) had been working 1 to 5 years in the current hospital and 72 of them (46%) had been working 1–5 years in the current unit in the hospital. The majority of respondents (n = 138, 87%) worked more than 40 h per week and 139 of them (88%) had direct interaction or contact with patients. The details are presented in Table 1.
| Characteristics | Hospital-A 107 (67.72%) n (%) | Hospital-B 51 (32.28%) n (%) | Total 158 (100%) |
|---|---|---|---|
| Position in hospital | |||
| Administration/management | 3 (2.8) | 2 (3.9) | 5 (3.2) |
| Clinical instructor | 1 (0.9) | 0 (0.0) | 1 (0.6) |
| Clinical resource nurse | 1 (0.9) | 0 (0.0) | 1 (0.6) |
| Dentist | 6 (5.6) | 3 (2.8) | 9 (5.7) |
| Consultant | 3 (2.8) | 0 (0.0) | 3 (1.9) |
| Dietician | 0 (0.0) | 1 (2.0) | 1 (0.6) |
| Infection control nurse | 3 (2.8) | 2 (3.9) | 5 (3.2) |
| Medical lab scientist | 1 (0.9) | 0 (0.0) | 1 (0.6) |
| Medical officer | 4 (3.7) | 1 (2.0) | 5 (3.2) |
| Nursing education team | 1 (0.9) | 1 (2.0) | 2 (1.3) |
| Patient care assistant | 0 (0.0) | 2 (3.9) | 2 (1.3) |
| Pharmacist/pharmacy assistant | 59 (55.1) | 8 (15.7) | 67 (42.4) |
| Physical, occupational or speech therapist | 1 (2.0) | 1 (2.0) | 2 (1.3) |
| Staff nurse | 15 (14.0) | 17 (33.3) | 32 (20.3) |
| Supervisory roles | 9 (8.4) | 13 (25.5) | 22 (13.9) |
| Work unit | |||
| Accident & emergency | 3 (2.8) | 2 (3.9) | 5 (3.2) |
| Administrative | 0 (0.0) | 3 (5.9) | 3 (1.9) |
| Critical care unit | 6 (5.6) | 1 (2.0) | 7 (4.4) |
| Haemodialysis | 1 (0.9) | 2 (3.9) | 3 (1.9) |
| Laboratory | 2 (1.9) | 1 (2.0) | 3 (1.9) |
| Labor room | 0 (0.0) | 2 (3.9) | 2 (1.3) |
| Many different hospital units/no specific unit | 9 (8.4) | 2 (3.9) | 11 (7.0) |
| Medical/surgical wards | 9 (8.4) | 12 (23.5) | 21 (13.3) |
| Medical oncology | 1 (0.9) | 2 (3.9) | 3 (1.9) |
| NICU/nursery | 1 (0.9) | 2 (3.9) | 3 (1.9) |
| Nursing educations | 3 (2.8) | 1 (2.0) | 4 (2.5) |
| OT/OT recovery/cath lab/surgical daycare | 2 (1.9) | 2 (3.9) | 4 (2.5) |
| Outpatient clinics | 3 (2.8) | 0 (0.0) | 3 (1.9) |
| Pharmacy & retail pharmacy | 49 (45.8) | 8 (15.7) | 57 (36.1) |
| Quality resources | 1 (0.9) | 0 (0.0) | 1 (0.6) |
| Radiology | 4 (3.7) | 1 (2.0) | 5 (3.2) |
| Radiotherapy & nuclear medicine | 1 (0.9) | 5 (9.8) | 6 (3.8) |
| Rehabilitation medicine centre | 1 (0.9) | 1 (2.0) | 2 (1.3) |
| Staff health clinic | 2 (1.8) | 0 (0.0) | 2 (1.3) |
| Telemedicine command centre | 1 (0.9) | 0 (0.0) | 1 (0.6) |
| Wellness centre | 4 (3.7) | 0 (0.0) | 4 (2.5) |
| Women & children wards | 4 (3.7) | 4 (7.8) | 8 (5.1) |
| Years of working in the hospital | |||
| Less than 1 year | 31 (29.0) | 11 (21.6) | 42 (26.6) |
| 1–5 years | 44 (41.1) | 22 (43.1) | 66 (41.8) |
| 6–10 years | 19 (17.8) | 18 (35.3) | 37 (23.4) |
| 11–15 years | 13 (12.1) | 0 (0.0) | 13 (8.2) |
| 16–20 years | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 21 years or more | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Years of working in the current unit | |||
| Less than 1 year | 36 (33.6) | 14 (27.5) | 50 (31.6) |
| 1–5 years | 48 (44.9) | 24 (47.1) | 72 (45.6) |
| 6–10 years | 14 (13.1) | 13 (25.5) | 27 (17.1) |
| 11 or more years | 8 (7.5) | 0 (0.0) | 8 (5.1) |
| 16–20 years | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 21 years or more | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing data | 1 (0.9) | 0 (0.0) | 1 (0.6) |
| Hours worked per week | |||
| Less than 30 h per week | 0 (0.0) | 1 (2.0) | 1 (0.6) |
| 30 to 40 h per week | 16 (15.0) | 2 (3.9) | 18 (11.4) |
| More than 40 h per week | 90 (84.1) | 48 (94.1) | 138 (87.3) |
| Missing | 1 (0.9) | 0 (0.0) | 1 (0.6) |
| Direct contact with patients | |||
| Yes | 98 (91.6) | 41 (80.4) | 139 (88.0) |
| No | 9 (8.4) | 10 (19.6) | 19 (12.0) |
3.2 Assessment of HCP's knowledge of patient safety
The highest overall positive response rate (PRR) of 89% was achieved by the domain “proactive to avoid risks in security,” followed by “understanding of human factors” (88%) and “openness in communication” (79%) domains. The domains “awareness of errors” and “system complexity and interrelationship” had a low PRRs of 46% and 25% respectively. The mean PRR for all 21 items was 73%. The details of the PRR of each domain and item are presented in Table 2. The awareness of errors among HCPs is significant in both Hospital A and Hospital B. HCPs from both hospitals have learned to properly inform patients who have suffered harm or injury as a result of an error (p < 0.05). The details of the comparison of NPR and NOR of HCPs in the assessment of patient safety knowledge are provided in Supporting Information S1: Tables S1 and S2.
| Item | Overall PRR (%) |
|---|---|
| 1. Awareness of errors | 46 |
| 1. During my training, on at least one occasion I have done something that was not safe for the patient | 41 |
| 2. During my training, I have seen a fellow student doing something that was not safe for the patient | 49 |
| 3. During my training, I have observed professionals doing something that was not safe for the patient | 48 |
| 2. Understanding of human factors | 88 |
| 1. In services where I have done clinical training practice, teachers explained to me the safety standards they follow with patients | 90 |
| 2. Teachers insisted on the importance of following treatment protocols for better health care | 91 |
| 3. During my training, teachers have insisted on the importance of the proper use of therapeutic resources for patient safety | 91 |
| 4. Teachers have insisted on the importance of hand-washing | 80 |
| 3. Proactive to avoid risks in security | 89 |
| 1. During my studies, my teachers explained to me what to do to avoid common mistakes and ensure patient safety | 89 |
| 2. During my practices, I have learned that, when an error occurred, steps must be taken to ensure it will not happen in the future | 95 |
| 3. Teachers discuss in class errors that are easy to make and provide us with recommendations on how to avoid them | 82 |
| 4. During my training, my teachers have explained the objectives and priorities for safer health care | 89 |
| 4. System complexity and interrelationship | 25 |
| 1. In my clinical training practice, I have found that most medical errors are impossible to avoid | 19 |
| 2. During my clinical training practice, I have observed that the protocols implemented to ensure patient safety are outdated | 32 |
| 5. Openness in communication | 79 |
| 1. I have learned to properly inform patients who have suffered harm or injury as a result of an error | 66 |
| 2. During my training, I have learned to assess the risks for patient safety | 88 |
| 3. In my training, I have learned what I do if I make a mistake | 89 |
| 4. During my training, I was able to discuss with my instructors or supervisors any unsafe situation that I had seen | 83 |
| 5. During my training, I acquired skills of how to properly report an error to colleagues and bosses | 82 |
| 6. During my training, I worked on the feelings that I could have if I make a mistake | 69 |
| 7. We have learned how to better communicate with patients to prevent medication errors | 90 |
| 8. In the hospital where I did my clinical training practice, a nonpunitive culture was promoted so that if an error occurred we knew how to prevent it from recurring | 65 |
| Overall positive response rate (PRR) for 21 items | 73 |
- Abbreviation: PRR, positive response rate.
3.3 Assessment of HCPs' attitudes and perceptions of patient safety
Among the domains, “communication about error” scored the highest PRR, which was 80%. “Organizational learning-continuous improvement” scored the second highest PRR of 74%, followed by both “teamwork” and “supervisor, manager, or clinical leader support for patient safety” with a PRR of 70%. “Responses to error” and “handoffs and information exchange “scored a PRR of 40% and 39%, respectively. The lowest PRR was observed for “staffing and work pace” at 28%. The overall mean PRR for attitude and perception of patient safety was 56%. The details of the PRR on the assessment of HCPs' attitudes and perceptions of patient safety are presented in Table 3. The comparison of the overall PRR of the current study and the HSOPSC-AHRQ database is presented in Figure 1. The comparison of NPR and NOR of the different professions in Hospital A and Hospital B for HSOPSC revealed that the culture of patient safety is significantly higher in Hospital A than in Hospital B. Most importantly, the nursing profession significantly scored higher than other professions. The details are presented in Supporting Information S1: Table S3.
| Dimensions/items | Overall PRR (%) |
|---|---|
| 1. Teamwork | 70 |
| A1. In this unit, we work together as an effective team. | 82 |
| A8. During busy times, staff in this unit help each other. | 74 |
| A9. There is a problem with disrespectful behavior by those working in this unit. (Negatively worded) | 53 |
| 2. Staffing and work pace | 28 |
| A2. In this unit, we have enough staff to handle the workload. | 22 |
| A3. Staff in this unit work longer hours than is best for patient care. (Negatively worded) | 27 |
| A5. This unit relies too much on temporary, float, or PRN staff. (Negatively worded) | 39 |
| A11. The work pace in this unit is so rushed that it negatively affects patient safety. (Negatively worded) | 25 |
| 3. Organizational learning—continuous improvement | 74 |
| A4. This unit regularly reviews work processes to determine if changes are needed to improve patient safety. | 81 |
| A12. In this unit, changes to improve patient safety are evaluated to see how well they worked. | 79 |
| A14. This unit lets the same patient safety problems keep happening. (Negatively worded) | 62 |
| 4. Response to error | 40 |
| A6. In this unit, staff feel like their mistakes are held against them. (Negatively worded) | 22 |
| A7. When an event is reported in this unit, it feels like the person is being written up, not the problem. (Negatively worded) | 34 |
| A10. When staff make errors, this unit focuses on learning rather than blaming individuals. | 47 |
| A13. In this unit, there is a lack of support for staff involved in patient safety errors. (Negatively worded) | 56 |
| 5. Supervisor, manager, or clinical leader support for patient safety | 70 |
| B1. My supervisor, manager, or clinical leader seriously considers staff suggestions for improving patient safety. | 74 |
| B2. My supervisor, manager, or clinical leader wants us to work faster during busy times, even if it means taking shortcuts. (Negatively worded) | 56 |
| B3. My supervisor, manager, or clinical leader takes action to address patient safety concerns that are brought to their attention. | 81 |
| 6. Communication about error | 80 |
| C1. We are informed about errors that happen in this unit. | 81 |
| C2. When errors happen in this unit, we discuss ways to prevent them from happening again. | 82 |
| C3. In this unit, we are informed about changes that are made based on event reports. | 77 |
| 7. Communication openness | 53 |
| C4. In this unit, staff speak up if they see something that may negatively affect patient care. | 59 |
| C5. When staff in this unit see someone with more authority doing something unsafe for patients, they speak up. | 48 |
| C6. When staff in this unit speak up, those with more authority are open to their patient safety concerns. | 61 |
| C7. In this unit, staff are afraid to ask questions when something does not seem right. (Negatively worded) | 41 |
| 8. Reporting patient safety events | 48 |
| D1. When a mistake is caught and corrected before reaching the patient, how often is this reported? | 42 |
| D2. When a mistake reaches the patient and could have harmed the patient, but did not, how often is this reported? | 54 |
| 9. Hospital management support for patient safety | 64 |
| F1. The actions of hospital management show that patient safety is a top priority. | 81 |
| F2. Hospital management provides adequate resources to improve patient safety. | 76 |
| F3. Hospital management seems interested in patient safety only after an adverse event happens. (Negatively worded) | 34 |
| 10. Handoffs and information exchange | 39 |
| F4. When transferring patients from one unit to another, important information is often left out. (Negatively worded) | 34 |
| F5. During shift changes, important patient care information is often left out. (Negatively worded) | 40 |
| F6. During shift changes, there is adequate time to exchange all key patient care information. | 45 |
| Overall Positive Response Rate (PRR) for 32 items | 56 |
- Abbreviations: HSOPSC, Hospital Survey on Patient Safety Culture; PRR, positive Response Rate.
An assessment of the number of safety events reported in the last 12 months revealed that 37% (n = 59) of HCPs did not report any patient safety events, while 34% (n = 54) reported 1 to 2 patient safety events in the same period. The details are presented in Table 4. Each participant in this study was asked to rate the overall patient safety of their unit or work area. The majority of respondents rated their unit or work area as “very good” (n = 78; 49%), 28% rated it as “good” (n = 44) and 20% rated it as “excellent” (n = 32. Only 3% rated the patient safety in their unit or work area as “poor.” The details are presented in Table 5.
| Number of patient safety events reported | Number of respondents n (%) | Total n (%) | |
|---|---|---|---|
| Hospital-A | Hospital-B | ||
| None | 36 (34) | 23 (45) | 59 (37) |
| 1–2 | 37 (35) | 17 (33) | 54 (34) |
| 3–5 | 24 (22) | 6 (12) | 30 (19) |
| 6–10 | 6 (6) | 3 (6) | 9 (6) |
| >11 | 3 (3) | 2 (4) | 5 (3) |
| Missing | 1 (1) | 0 (0) | 1 (1) |
| Total | 107 (100) | 51 (100) | 158 (100) |
| Patient safety grade | Number of respondents n (%) | Total n (%) | |
|---|---|---|---|
| Hospital-A | Hospital-B | ||
| Excellent | 18 (17) | 14 (27) | 32 (20) |
| Very good | 61 (57) | 17 (33) | 78 (49) |
| Good | 28 (26) | 16 (31) | 44 (28) |
| Fair | 0 (0) | 3 (6) | 3 (2) |
| Poor | 0 (0) | 1 (2) | 1 (1) |
| Total | 107 (100) | 51 (100) | 158 (100) |
The bivariate analysis revealed that all 10 dimensions of patient safety culture were significantly associated with overall patient safety grade. A stronger patient safety culture suggests a greater likelihood of receiving a high overall patient safety grade. Additionally, physicians, pharmacists, technicians, and those with no direct patient contact were also correlated with higher overall patient safety grades. However, working experience and weekly working hours did not show a significant association with overall patient safety grade.
The results of the multivariate analysis showed that all domains of patient safety culture, except for reporting patient safety events, support from hospital management, and handoff and information exchange, were significantly associated with overall patient safety grades. Additionally, the position of healthcare providers, no direct contact with patients, and the number of patient safety events reported were also associated with a high overall patient safety grade. However, there was no correlation found between working experience, weekly working hours, and the overall patient safety grade. The details are presented in Supporting Information S1: Table S4.
4 DISCUSSION
The response rate of HCPs in the present study was less than 50%, significantly lower than in earlier studies.10, 16 Previous studies conducted at King Fahd University Hospital (KFUH) in Saudi Arabia had a response rate of 67%,16 while a study at Sarawak General Hospital (SGH) in Malaysia had a response rate of 81.4%,10 both higher than the present study. One possible explanation for this difference is that the current study was conducted by working pharmacists at the hospital, whereas the KFUH survey was carried out by healthcare authorities such as the Saudi Central Board for Accreditation of Healthcare Institutions (CBAHI) and Joint Commission International (JCI) to meet their annual accreditation requirements. The higher response rate in the SGH study may be attributed to the fact that it included all hospital staff, whereas the current study focused solely on HCPs. Involving healthcare authorities in research related to healthcare services is crucial for obtaining desired responses from healthcare workers, which can help assess the current status of patient safety culture and implement effective strategies to maintain the highest standards of healthcare services.3, 5, 17, 18
The majority of respondents in the present study were pharmacists, pharmacy assistants, staff nurses, and individuals in supervisory roles. In a previous study conducted at SGH in Malaysia, most respondents were staff nurses (42.5%) followed by medical officers (17.2%).10 In comparison to a study at KFUH, in the Kingdom of Saudi Arabia, the majority of participants were registered nurses (58%), followed by respiratory therapists (13%), with no responses from administration/management staff.16 Unlike other studies,10, 16, 19, 20 pharmacists or pharmacy assistants were responsive in the present study. Pharmacists and nurses at the study hospitals showed more enthusiasm to participate in patient safety-related research while other HCPs showed less interest. This may be because medical officers or prescribers in these hospitals were overwhelmed with workloads due to staff shortages in their units/areas, making it challenging to find time for healthcare research. Despite having higher workloads and working long hours in the day and night shifts, it is highly essential to participate in health care research and express their views and opinions for better strategic planning to minimse the errors. A previous study revealed that increased night shifts may result in more reports of adverse events and near misses. Working hours, the number of night shifts, and the number of days off have different influences on the patient safety culture of physicians and nurses.21
Pharmacists hold a unique position at the intersection of medication and patient care. Their expertise in drugs and daily interactions with patients makes them invaluable assets in healthcare research. Hospital pharmacists play a prominent role in reducing medication errors, adverse drug events, and promoting medication safety activities.22 Pharmacists' participation in research projects can bridge the gap between theoretical treatments and real-world effectiveness upholding a culture of patient safety. They can design studies or interventions relevant to everyday practice, monitor medication adherence, and provide valuable insights into patient experiences. This expanded role for pharmacists would ultimately benefit patients by leading to more effective and personalized treatments and reducing preventable errors.23
HCPs from the pharmacy department and medical or surgical ward, especially those with fewer years of experience played a significant role in this study. In comparison, 27.7% of HCPs at SGH10 and 11.7% at KFUH16 were from the medical or surgical ward. HCPs with less work experience were keen to participate in the study, demonstrating their commitment to learning more about patient safety and maintaining a culture of patient safety in their units/areas. Junior or new staff members were more willing to speak up about issues than senior or experienced staff, which may explain why there were more junior staff members in this study. Hierarchical leadership is an antiquated practice common in the health care industry in which clearly defined roles and their importance are overemphasised. In a high-pressure environment, this can have unintended negative consequences. Hierarchical leadership significantly impacts healthcare outcomes by affecting employee morale, affecting patient safety. Individuals may be blamed, rather than encouraging a collectively responsible mentality.24-26
The study assessed the practical knowledge of patient safety among HCPs, focusing on their ability to apply knowledge in real-life situations rather than just theoretical understanding. The results showed that respondents from Hospital A scored higher in the “Awareness of error” domain than those from Hospital B. Interestingly, 19% of the participants believed that most medical errors they experienced during their training were unavoidable. In a study conducted among medical students at a university in Malaysia to determine awareness and attitude toward patient safety, 40% of the medical students agreed that most healthcare workers commit errors.27 Similarly, in a Pakistani Medical School, undergraduate medical students agreed that human error is inevitable (Mean = 5.25, SD = 1.58).28 A similar study conducted at Children's Hospital Lahore showed consistent findings in postgraduate residents (Mean = 5.20, SD = 1.622) and nurses (Mean = 5.32, SD = 1.727).29 A study conducted among second and third-year nursing students at a private university college in Malaysia found that nearly all (99%) nursing students had a good knowledge of patient safety.30 The difference in response to the items might be due to the different curriculum offered during their training in terms of exposure to patient safety aspects. The theoretical and practical knowledge of HCPs on patient safety, their practices in healthcare settings, and the provisions and facilities provided to them play a significant role in the highest level of patient safety culture. Any negative perception and poor practice may lead to adverse outcomes, ultimately harming the patient population.
In 2011, WHO developed the Multi-professional Patient Safety Curriculum Guide to assist in teaching and learning patient safety in universities and schools for dentistry, medicine, midwifery, nursing, and pharmacy students. The guide also supports the continuous training of all HCPs.31 The topics covered in this guide provide an introduction to patient safety, the importance of applying human factors in patient safety, being a great and helpful team player, understanding the complexity of the healthcare system on patient care, learning from mistakes to prevent harm, using quality improvement strategies to enhance patient care, understanding clinical risk and its management, engaging with patients and carers, infection control and prevention, improving the safe use of medication, patient safety, and invasive procedures. In 2017, the Director General of Health Malaysia implemented a compulsory patient safety awareness course for house officers before they began their posting in healthcare institutions.32 This strategy aimed to improve the knowledge of patient safety in HCPs thus enhancing the quality of healthcare in Malaysia.
In the present study, the overall mean PRR score for the 10 composites of the HSOPSC was lower than the AHRQ database, which was 70% in AHRQ,33 and lower than the scores reported in studies from Bulgaria (59%)34 and Vietnam (74%).35 However, this score is higher than the results of the study from Sarawak (50.1%)10 and Southeast Ethiopia (44%).20 A low PRR score, indicating a weak patient safety culture, can significantly impact patient well-being. It discourages staff from reporting errors, hindering the identification and prevention of future incidents. This can lead to increased medication mistakes, infections, and other avoidable harm. Addressing these weaknesses through open communication and a just culture is crucial for patient safety.36-38
In the present study, the “communication about error” domain scored the highest PRR followed by “organizational learning-continuous improvement.” Both domains scored higher compared to the data from AHRQ. In terms of communication about errors, the score was higher than in studies conducted in Ethiopia (71%),20 Saudi Arabia (56%),39 and Afghanistan (43%).40 This may be because hospital staff in the present study are aware of errors that occurred in their unit and share opinions or ideas for preventive measures. Additionally, staff in both hospitals are informed of workflow changes based on reported events and regularly review these changes to enhance patient safety. Clear communication among HCPs reduces errors and misunderstandings, improving patient safety by ensuring that everyone involved has the same critical information. This leads to better care and fewer complications.41-43
The domain “staffing and work pace” had the lowest PRR in this study, which aligns with findings from previous studies in Bulgaria19 and China,34 where this domain generally scored lower compared to others. This contrasts with AHRQ data, which showed a higher score (51%) than the current study. According to WHO, there is a projected shortage of 10 million healthcare workers by 2030, particularly in low- and lower-middle-income countries.44 The Centers for Disease Control and Prevention (CDC) emphasizes the importance of maintaining adequate staff levels in healthcare institutions to ensure a safe working environment for healthcare workers and improve patient safety.45 Staff in this study expressed feeling a shortage of staff in their department/unit, attributed to various factors such as HCPs falling ill during the COVID-19 pandemic, requiring those in close contact to quarantine at home or take leave to care for infected family members. Additionally, the recent resignations of experienced staff have further depleted staffing levels, with new hires who are still in training struggling to keep up with operations. This has resulted in staff having to work faster to accommodate the increased number of patients in the hospital.
The majority of respondents in this study worked more than 40 h per week, which is similar to a patient safety study conducted at Sarawak General Hospital, in Malaysia.10 These findings are higher compared to studies in China,19 Afghanistan,39 Sweden,46 and AHRQ data33 where only 72%, 66%, 50%, and 28% of respondents worked more than 40 h per week. According to the Malaysian Employment Act Amendment 2022, the maximum working hours have been reduced from 48 to 45 h. However, some healthcare staff may still need to work overtime or double shifts to cover for colleagues who are absent due to illness or on personal leave. Working long hours can be a recipe for disaster. The more hours worked each week, the more fatigue creeps in. This fatigue can cloud an HCP's judgment, slow reaction times, and weaken the ability to focus. As a result, errors become more likely. Simple tasks take longer, and complex ones become more prone to mistakes. This not only impacts the quality of work but can also lead to safety hazards. To avoid this downward spiral, it is crucial to find a healthy work-life balance and prioritize sufficient rest.47, 48
More than half of the respondents in this study reported at least one patient safety event in the last 12 months. This finding was slightly lower compared to a study in Egypt (70%)49 but higher than the studies reported in Saudi Arabia (58%),40 Afghanistan (50%),39 AHRQ database (45%),33 China (40%),19 and Turkey (20%).50 Many reasons could influence the frequency of events reported. As highlighted in a previous study, HCPs believe there will be a possible negative effect on the relationship with employees when they report a patient safety event, which was considered the most common barrier in incident reporting.51 The practice of medication error reporting could vary among hospital setups. In another study, 11% of the staff would not report their colleagues when a medication error happened, while half of them would report their colleagues if they made a medication error.52 The reasons for the failure of incident reporting could be an inappropriate reporting system, failure of leadership to encourage incident reporting, not making incident reporting a priority, a “filter system” of the incident reports instead of escalating to higher management by the immediate supervisor or focusing on a large number of incident reports rather than an appropriate review of the incident and an effective response after the incident.53
In the present study, more than two-thirds of the respondents considered the overall patient safety grade of their hospital to be excellent or very good, which is consistent with AHRQ data and a study in Saudi Arabia.33, 40 In a study conducted in Malaysia, the majority of the respondents rated patient safety grades as acceptable.10 Around half of the nursing staff in the present study reported that patient safety in their hospital is very good, which was similar to an earlier study, where 47% of the nurses rated patient safety grades as very good.54 On the contrary, 32% of the nurses in another study rated their hospital's patient safety grade as fair or poor.55 In 2019, the World Health Assembly (WHA) recognised patient safety as a priority in global health and adopted a resolution on Patient Safety which endorsed the establishment of World Patient Safety Day on September 17 to be observed annually by member states.6 Patient Safety Week was conducted annually in both hospitals of the present study to raise awareness of patient safety among HCPs, which could be another reason for the respondents rating better scores in the overall patient safety grade of these hospitals. Additionally, International Patient Safety Goals (IPSGs)56, 57 training was conducted annually by the Quality Department in both hospitals for all staff as an initiative to improve patient safety. Overall, the staff in both hospitals have considerably optimal levels of knowledge of patient safety, but this is not sufficient to ensure that harm does not reach the patient. There is room for burnout among the HCPs as staffing and work pressure are big issues among the HCPs in these hospitals and encouragement to report patient safety incidents is warranted.
There are a few limitations to this study. Firstly, the sample size was smaller than expected, which does not allow for generalization to the entire hospital. Secondly, some staff members were reluctant to provide responses related to work and hospital management because they would need to sign a consent form and provide their identity before participating. As a result, they chose not to participate. Although researchers reassured that the anonymity of respondents would be maintained, the level of participation was lower than expected. Additionally, since the study was conducted in only two different tertiary-level hospitals, the findings may not accurately represent the patient safety culture of all Malaysian hospital settings. The interval in the number of patient safety events created by AHRQ is not uniform, hence, the current study's findings on the number of patient safety events were not in the uniform interval nature and may not reflect the actual events reported by the HCPs.
The study recommends that in the future, staff from all departments—including business, facility, support services, and information technology—should be included, as they play a direct or indirect role in patient safety management. Future studies can be conducted both online and in face-to-face mode for the convenience of participants, rather than focusing on just one mode of research. It is also recommended to include public hospitals alongside private hospitals to compare patient safety culture in both settings.
5 CONCLUSION
Staff at both hospitals have an optimal level of knowledge regarding patient safety culture. Staffing, work pace, handoffs, information exchange, and response to errors are the areas identified for improvement. In the present study, most dimensions of HSOPSC were found to be lower compared to the benchmark in the AHRQ database. A well-structured intervention programme focusing on all essential domains of patient safety should be conducted periodically to improve the patient safety culture in healthcare settings. To investigate overall patient safety practices in hospital settings, future research should be carried out in a wider population and include nonclinical departments.
AUTHOR CONTRIBUTIONS
Cheong Sok May: Data curation; formal analysis; project administration; resources; writing—review and editing; writing—original draft; validation. Palanisamy Sivanandy: Conceptualization; data curation; writing—original draft; software; methodology; funding acquisition; supervision. Pravinkumar V. Ingle: Conceptualization; data curation; formal analysis; investigation; methodology; supervision. Priya Manirajan: Software; resources; validation; visualization; writing—review and editing.
ACKNOWLEDGMENTS
We would like to thank the management of International Medical University, and the two tertiary level hospitals, for the necessary support to carry out this research. This research is funded by the International Medical University, Kuala Lumpur, Malaysia (Grant approval number is MPP 1-2022(02)). [Correction added on 28 November 2024, after online publication: The names of the participating hospitals have been removed.]
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
The study was approved by the Joint Committee on Research and Ethics of the IMU (approval number MPP 1-2022(02)), Hospital A (SREC: 01/2022/IND/ER), and Clinical Research Centre (CRC), Hospital B Research Board (SRB: SRB/IIR/SMC/NF/22/007). [Correction added on 28 November 2024, after online publication: The names of the participating hospitals have been removed.]
TRANSPARENCY STATEMENT
The lead author Palanisamy Sivanandy affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.